Abstract
Purpose
Some patients do not have the expected weight loss, and the post-surgical diet may partially explain these differences.
Objectives
To estimate the impact of macronutrient substitution on obesity remission after RYGB, considering the protein source.
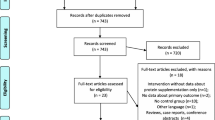
Materials and Methods
This study included 58 patients undergoing RYGB. Data collection was performed preoperatively, 3 and 12 months after surgery. Eight participants dropped out of the study at 3 months, and the others remained for 12 months. The foods consumed were registered using a 24-h, 3-day food recall. For the isocaloric substitution analysis, foods were classified according to the protein source. The groups were compared using hypothesis tests, and Cox proportional hazard ratio regression was used to analyze isocaloric substitution.
Results
At three months after surgery, every 5% energy from plant protein replaced by animal protein increased by 3.50 [CI 1.204 — 10.205; p = 0.021] the probability of obesity remission. Stratified analysis by protein groups indicated that replacing vegetable protein with white meat was positively associated with remission of obesity. Every 5% vegetable protein replaced with white meat increased by 3.20 [CI 1.026 — 9.981; p = 0.045] the probability of obesity remission. Both results were independent of age, body mass index (BMI), and the presence of comorbidities.
Conclusion
The results suggest that the consumption of animal proteins after RYGB, mainly white meat, favors weight loss.
Graphical Abstract





Similar content being viewed by others
References
Cooper TC, Simmons EB, Webb K, et al. Trends in weight regain following Roux-en-Y gastric bypass (RYGB ) bariatric surgery. Obes Surg. 2015;25(8):5–12.
Nicoletti CF, de Oliveira BAP, de Pinhel MAS, et al. Influence of excess weight loss and weight regain on biochemical indicators during a 4-year follow-up after Roux-en-Y gastric bypass. Obes Surg. 2015;25(2):279–84.
Sarwer DB, Wadden TA, Moore RH, et al. Preoperative eating behavior, postoperative dietary adherence and weight loss following gastric bypass surgery. Surg Obes Relat Dis. 2008;4(5):640–6.
Robinson AH, Adler S, Stevens HB, et al. What variables are associated with successful weight loss outcomes for bariatric surgery after 1 year? Surg Obes Relat Dis. 2014;10(4):697–704.
Tabesh MR, Maleklou F, Ejtehadi F, et al. Nutrition, physical activity, and prescription of supplements in pre- and post-bariatric surgery patients: a practical guideline. Obes Surg. 2019;29:3385–400.
Pinto SL, Juvanhol LL, Bressan J. Increase in protein intake after 3 months of RYGB is an independent predictor for the remission of obesity in the first rear of surgery. Obes Surg. 2019;29(12):3780–5.
van den Broek M, de Heide LJM, Veeger NJGM, et al. Influence of dietary protein and its amino acid composition on postoperative outcomes after gastric bypass surgery: a systematic review. Nutr Rev. 2016;74(12):749–73.
World Medical Association (WMA). World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;27;310(20):2191–4.
Pereira DAA, Vieira SA, Fogal AS, et al. Aspectos metodológicos na construção de projetos de pesquisa em Nutrição Clínica. Rev Nutr Campinas. 2014;27(5):597–604.
Barufaldi LA, Abreu GDA, da Veiga GV, et al. Software to record 24-hour food recall: application in the study of cardiovascular risks in adolescents. Rev Bras Epidemiol. 2016;19(2):464–8.
Jelliffe DB. The assessment of the nutritional status of the community (with special reference to field surveys in develo** regions of the world). World Heal Organ. monograph series. 1968. p. 271.
Consultation WHO. Obesity: preventing and managing the global epidemic. WHO techni. Geneva: World Health Organization; 2000.
Callaway CW, Chumlea WC, Bouchard C et al. Circumference. Anthro standardization reference manual, champaign (IL). In: Lohman TG, Roche AF MR, Martorell R (eds.). Human Kinetics Books. 1988. pp. 39–54.
Ben-noun LL, Laor A. Relationship of neck circumference to cardiovascular risk factors. Obes Res. 2003;11(2):226–31.
Geloneze B, Carolina A, Vasques J, et al. HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome – Brazilian metabolic syndrome study (BRAMS). Arq Bras Endocrinol Metab. 2009;53(2):281–7.
Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome — a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469–80.
Gilbert J, Bendsen NT, Tremblay A, et al. Effect of proteins from different sources on body composition. Nutr Metab Cardiovasc Dis. 2011;21(2):B16-31.
Larsen TM, Dalskov S-M, van Baak M, et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N Engl J Med. 2010;363(22):2102–13.
Kanerva N, Larsson I, Peltonen M, et al. Changes in total energy intake and macronutrient composition after bariatric surgery predict long-term weight outcome: Findings from the Swedish Obese Subjects (SOS) study. Am J Clin Nutr. 2017;106(1):136–45.
Halton TL, Hu FB. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. J Am Coll Nutr. 2004;23(5):373–85.
Moizé V, Andreu A, Rodríguez L, et al. Protein intake and lean tissue mass retention following bariatric surgery. Clin Nutr. 2013;32:550–5.
Evans EM, Mojtahedi MC, Thorpe MP, et al. Effects of protein intake and gender on body composition changes: a randomized clinical weight loss trial. Nutr Metab (Lond). 2012;9(55):1–9.
Alfenas RCG, Bressan J, de Paiva AC. Effects of protein quality on appetite and energy metabolism in normal weight subjects. Arq Bras Endocrinol Metabol. 2010;54(1):45–51.
Berrazaga I, Micard V, Gueugneau M, et al. The role of the anabolic properties of plant- versus animal-based protein sources in supporting muscle mass maintenance: a critical review. Nutrients. 2019;11(1825):1–21.
Wilson J, Wilson GJ. Contemporary issues in protein requirements and consumption for resistance trained athletes. J Int Soc Sports Nutr. 2006;3(1):7–27.
Zarshenas N, Tapsell LC, Neale EP, et al. The relationship between bariatric surgery and diet quality: a systematic review. Obes Surg. 2020;30(5):1768–92.
Steenackers N, Vanuytsel T, Augustijns P, et al. Adaptations in gastrointestinal physiology after sleeve gastrectomy and Roux-en-Y gastric bypass. Lancet Gastroenterol Hepatol. 2021;6(3):225–37.
Mikkelsen PB, Toubro S, Astrup A. Effect of fat-reduced diets on 24-h energy expenditure: comparisons between animal protein, vegetable protein, and carbohydrate. Am J Clin Nutr. 2000;72:1135–41.
Westerterp-Plantenga MS, Nieuwenhuizen A, Tomé D, et al. Dietary protein, weight loss, and weight maintenance. Annu Rev Nutr. 2009;29:21–41.
Yang Y, Churchward-venne TA, Burd NA, et al. Myofibrillar protein synthesis following ingestion of soy protein isolate at rest and after resistance exercise in elderly men. Nutr Metab (Lond). 2012;9(57):1–9.
Giuberti G, Morlacchini M, Crippa L, et al. Effect of omnivorous and vegan diets with different protein and carbohydrate content on growth and metabolism of growing rats. Int J Food Sci Nutr. 2018;69(5):574–83.
Van BMA, Larsen TM, Jebb SA, et al. Dietary intake of protein from different sources and weight regain, changes in body composition and cardiometabolic risk factors after weight loss: The DIOGenes Study. Nutrients. 2017;9(1326):1–13.
Hoffman JR, Falvo MJ. Protein – which is best ? J Sport Sci Med. 2003;3:118–30.
Bernstein AM, Pan A, Rexrode KM, et al. Dietary protein sources and the risk of stroke in men and women. Stroke. 2012;43:637–44.
Bernstein AM, Sun Q, Hu FB, et al. Major dietary protein sources and risk of coronary heart disease in women. Circulation. 2010;122:876–83.
Funding
The coordination for the improvement of higher education personnel—CAPES Foundation (Ministry of Education, Brazil) for Scholarships awarded to D.L.S.V. and A.S. (Funding Code 001) and the National Council for Scientific and Technological Development—CNPq (Ministry of Science, Technology and Innovation, Brazil) of which J.B. is a productivity scholar.
Author information
Authors and Affiliations
Contributions
Darlene Larissa de Souza Vilela: contributed to the study design, formal analysis and interpretation of the data, drafting of the manuscript, and approval of the final version.
Alessandra da Silva: contributed to the study design, formal analysis and interpretation of the data, critical review of the manuscript, and approval of the final version.
Sônia Lopes Pinto: contributed to study design, data collection and interpretation, supervision, critical review of the manuscript, and approval of the final version.
Josefina Bressan: contributed to study design, supervision, acquisition of funding for English revision, interpretation of data, critical review of the manuscript, and approval of the final version.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
Darlene L.S Vilela has no conflict of interest; Alessandra Silva has no conflict of interest; Sônia L. Pinto has no conflict of interest; Josefina Bressan has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Replace plant protein for animal protein increase probability of obesity remission.
• Replace plant protein for white meat increase probability of obesity remission.
• The group that achieved remission of obesity had lower BMI at baseline.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vilela, D.L., Silva, A., Pinto, S.L. et al. Animal Protein Intake Is Associated with Obesity Remission After Roux-en-Y Gastric Bypass: an Isocaloric Replacement Analysis. OBES SURG 33, 1382–1389 (2023). https://doi.org/10.1007/s11695-023-06539-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-023-06539-w