Abstract
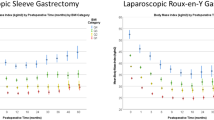
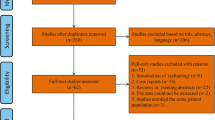
Percentage total weight loss (%TWL) might be better than percentage excess weight loss to express weight loss in bariatric surgery. In this systematic review, performed according to the PRISMA statement, results of laparoscopic sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (LRYGB) are assessed in %TWL. A total of 13,426 studies were screened and 49 included, reporting data of 24,760 patients. The results show that, despite limiting data, LRYGB is favorable over LSG in terms of weight loss in short-term follow-up. Although recent guidelines recommend to use %TWL when reporting outcome in bariatric surgery, this study shows that there is still insufficient quality data in %TWL, especially on LSG. The use of %TWL as the primary outcome measure in bariatric surgery should be encouraged.
Graphical abstract




Similar content being viewed by others
References
Dixon JB, Mcphail T, O’Brien PE. Minimal reporting requirements for weight loss : current methods Not Ideal. Obes Surg. 2005;15:1034–9.
Dallal RM, Quebbemann BB, Hunt LH, et al. Analysis of weight loss after bariatric surgery using mixed-effects linear modeling. Obes Surg. 2009;19:732–7.
van de Laar A, de Caluwé L, Dillemans B. Relative outcome measures for bariatric surgery. Evidence against excess weight loss and excess body mass index loss from a series of laparoscopic Roux-en-Y gastric bypass patients. Obes Surg. 2011;21:763–7.
van de Laar AWJM. Algorithm for weight loss after gastric bypass surgery considering body mass index, gender, and age from the Bariatric Outcome Longitudinal Database (BOLD). Surg Obes Relat Dis [Internet]. Elsevier; 2014;10:55–61. Available from: https://doi.org/10.1016/j.soard.2013.05.008
van de Laar AW, Dollé MH, de Brauw LM, et al. Validating the alterable weight loss (AWL) metric with 2-year weight loss outcome of 500 patients after gastric bypass. Obes Surg. 2014;24:1085–9.
Hatoum IJ, Kaplan LM. Advantages of percent weight loss as a method of reporting weight loss after Roux-en-Y gastric bypass. Obesity. 2013;21:1519–25.
Corcelles R, Boules M, Froylich D, et al. Total weight loss as the outcome measure of choice after Roux-en-Y gastric bypass. Obes Surg. 2016;26:1794–8.
Sczepaniak JP, Owens ML, Shukla H, et al. Comparability of weight loss reporting after gastric bypass and sleeve gastrectomy using BOLD Data 2008–2011. Obes Surg. 2015;25:788–95.
Grover BT, Morell MC, Kothari SN, Borgert AJ, Kallies KJ, Baker MT. Defining weight loss after bariatric surgery : a call for standardization. Obes Surg Obesity Surgery; [Epub adea.
van de Laar AW. The %EBMIL/%EWL double-booby trap. A comment on studies that compare the effect of bariatric surgery between heavier and lighter patients. Obes Surg. 2016;26:612–3.
van de Laar AW, De Brauw LM, Meesters EW. Relationships between type 2 diabetes remission after gastric bypass and different weight loss metrics: arguments against excess weight loss in metabolic surgery. Surg Obes Relat Dis [Internet]. Elsevier; 2016;12:274–82. Available from: https://doi.org/10.1016/j.soard.2015.07.005
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg [Internet]. 2015;25:587–606. Available from: http://springer.longhoe.net/10.1007/s11695-015-1645-3
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses : the PRISMA statement. BMJ [Internet]. 2009;2535:1–8. Available from: https://doi.org/10.1136/bmj.b2535
Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24:42–55.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses [Internet]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Inge TH, Courcoulas AP, Jenkins TM, et al. Five-year outcomes of gastric bypass in adolescents as compared with adults. N Engl J Med. 2019;380:2136–45.
Celio AC, Wu Q, Kasten KR, et al. Comparative effectiveness of Roux-en-Y gastric bypass and sleeve gastrectomy in super obese patients. Surg Endosc Springer US. 2017;31:317–23.
Monpellier VM, Antoniou EE, Aarts EO, et al. Improvement of health-related quality of life after Roux-en-Y gastric bypass related to weight loss. Obes Surg Obesity Surgery. 2017;27:1168–73.
Abdulrazzaq S, Elhag W, El Ansari W, et al. Is revisional gastric bypass as effective as primary gastric bypass for weight loss and improvement of comorbidities? Obes Surg Obesity Surgery. 2020;30:1219–29.
Aelfers SC, Schijns W, Ploeger N, et al. Patients ’ preoperative estimate of target weight and actual outcome after bariatric surgery. Obes Surg Obesity Surgery. 2017;27:1729–34.
Aftab H, Risstad H, Søvik TT, et al. Five-year outcome after gastric bypass for morbid obesity in a Norwegian cohort. Surg Obes Relat Dis. 2014;10:71–8.
Andreu A, Jimenez A, Vidal J, et al. Bariatric support groups predicts long-term weight loss. Obes Surg Obesity Surgery. 2020:3–8.
Aridi HD, Khazen G, Safadi BY. Comparison of outcomes between laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy in a Lebanese bariatric surgical practice. Obes Surg Obesity Surgery. 2018;28:396–404.
Bergh I, Kvalem IL, Mala T, et al. Predictors of physical activity after gastric bypass—a prospective study. Obes Surg Obesity Surgery. 2017;27:2050–7.
Bettencourt-Silva R, Neves JS, Pedro J, et al. Comparative effectiveness of different bariatric procedures in super morbid obesity. Obes Surg Obesity Surgery. 2019;29:281–91.
Bhandari M, Nautiyal HK, Kosta S, Mathur W, Fobi M. Comparison of one-anastomosis gastric bypass and Roux-en-Y gastric bypass for treatment of obesity: a 5-year study. Surg Obes Relat Dis. Elsevier Inc.; 2019;15:2038–44.
Calvo B, Gracia JA, Bielsa MA, Martínez M. Metabolic effects and outcomes of sleeve gastrectomy and gastric bypass: a cohort study. Surg Endosc [Internet]. Springer US; 2020; Available from: https://doi.org/10.1007/s00464-019-07355-z
Chahal-Kummen M, Salte OBK, Hewitt S, Blom-Høgestøl IK, Risstad H, Kristinsson J, et al. Health benefits and risks during 10 years after Roux-en-Y gastric bypass. Surg Endosc [Internet]. Springer US; 2020; Available from: https://doi.org/10.1007/s00464-019-07328-2
Chiappetta S, Schaack H, Wölnerhannsen B, et al. The impact of obesity and metabolic surgery on chronic inflammation. Obes Surg Obesity Surgery. 2018;28:3028–40.
Dogan K, Homan J, Aarts EO, et al. A short or a long Roux limb in gastric bypass surgery : does it matter? Surg Endosc Springer US. 2017;31:1882–90.
Faria G, Sc M, Preto J, et al. D M, et al. Fasting glycemia : a good predictor of weight loss after RYGB. Surg Obes Relat Dis. Elsevier. 2014;10:419–26.
Gero D, Favre L, Allemann P, et al. Laparoscopic Roux-en-Y gastric bypass improves lipid profile and decreases cardiovascular risk: a 5-year longitudinal cohort study of 1048 patients. Obes Res Obesity Surgery. 2018;28:805–11.
Gullick AA, Graham LA. Association of race and socioeconomic status with outcomes following laparoscopic Roux-en-Y Gastric Bypass. Obes Surg. 2015;25:705–11.
Hanvold SE, Vinknes KJ, Bastani NE, Turner C, Løken EB, Mala T, et al. Plasma amino acids, adiposity, and weight change after gastric bypass surgery : are amino acids associated with weight regain ? Eur J Nutr. Springer Berlin Heidelberg; 2018;57:2629–2637.
Høgestøl IK, Chahal-Kummen M, Eribe I, et al. Chronic abdominal pain and symptoms 5 years after gastric bypass for morbid obesity. Obes Surg Obesity Surgery. 2017;27:1438–45.
Jurgensen JA, Reidt W, Kellogg T, et al. Impact of patient attrition from bariatric surgery practice on clinical outcomes. Obes Surg Obesity Surgery. 2018;29:579–84.
Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Adams TD. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis. American Society for Metabolic and Bariatric Surgery; 2009;5:250–256.
Kvalem IL, Bårdstu S, Bergh I, Nordvik T, Sogg S, Mala T. Associations between perceived somatic symptoms and mental health after Roux-en-Y gastric bypass: a 3-year prospective cohort study. Surg Obes Relat Dis [Internet]. American Society for Bariatric Surgery; 2020;16:626–32. Available from: https://doi.org/10.1016/j.soard.2019.12.018
Lent MR, Hu Y, Benotti PN, et al. Demographic, clinical and behavioral determinants of seven-year weight change trajectories in Roux-en-Y gastric bypass patients. Surg Obes Relat Dis Elsevier Inc. 2018;14:1680–5.
Li RA, Fisher DP, Dutta S, O’Brien RM, Ackerson LM, Sorel ME, et al. Bariatric surgery results : reporting clinical characteristics and adverse outcomes from an integrated healthcare delivery system. Surg Obes Relat Dis [Internet]. Elsevier; 2015;11:1119–25. Available from: https://doi.org/10.1016/j.soard.2015.03.002
Madhok BM, Mahawar KK, Hadfield JN, et al. Haematological indices and haematinic levels after mini gastric bypass : a matched comparison with Roux-en-Y gastric bypass. Clin Obes. 2018;8:43–9.
Mantziari S, Dayer A, Duvoisin C, et al. Long-term weight loss, metabolic outcomes, and quality of life at 10 years after Roux-en-Y gastric bypass are independent of patients’ age at baseline. Obes Surg Obesity Surgery. 2020;30:1181–8.
Marek RJ, Tarescavage AM, Ben-Porath YS, et al. Using presurgical psychological testing to predict 1-year appointment adherence and weight loss in bariatric surgery patients : predictive validity and methodological considerations. Surg Obes Relat Dis Elsevier. 2015;11:1171–81.
Mazzini GS, Khoraki J, Browning MG, et al. Population diversity challenge the external validity of the european randomized controlled trials comparing laparoscopic gastric bypass and sleeve gastrectomy. Obes Surg Obesity Surgery. 2020;30:992–1000.
Ramírez EM, Espinosa O, Berrones R, et al. The impact of preoperative BMI (obesity class I, II, and III) on the 12-month evolution of patients undergoing laparoscopic gastric bypass. Obes Surg Obesity Surgery. 2018;28:3095–101.
Slegtenhorst BR, van der Harst E, Demirkiran A, de Korte J, Schelfhout LJ, Klaassen RA. Effect of primary versus revisional Roux-en-Y gastric bypass : inferior weight loss of revisional surgery after gastric banding. Surg Obes Relat Dis [Internet]. Elsevier Inc.; 2013;9:253–8. Available from: https://doi.org/10.1016/j.soard.2012.01.022
Thereaux J, Corigliano N, Poitou C, et al. Comparison of results after one year between sleeve gastrectomy and gastric bypass in patients with BMI Z 50 kg/m 2. Surg Obes Relat Dis [Internet]. Elsevier; 2015;11:785–90. Available from. 2015; https://doi.org/10.1016/j.soard.2014.11.022.
Vagenas K, Panagiotopoulos S, Kehagias I, et al. Prospective evaluation of laparoscopic Roux en Y gastric bypass in patients with clinically severe obesity. World J Gastroenterol. 2008;14:6024–9.
van de Laar AW, van Rijswijk AS, Kakar H, et al. Sensitivity and specificity of 50 % excess weight loss (50 % EWL) and twelve other bariatric criteria for weight loss success. Obes Surg Obesity Surgery. 2018;28:2297–304.
Wood GC, Benotti PN, Lee CJ, et al. Evaluation of the association between preoperative clinical factors and long-term weight loss after Roux-en-Y gastric bypass. JAMA Surg. 2016;151:1056–62.
Bettini S, Bordigato E, Fabris R, et al. Pra’ CD, Belligoli A, et al. Modifications of resting energy expenditure after sleeve gastrectomy. Obes Surg. Obes Surg. 2018;28:2481–6.
Caron M, Hould FS, Lescelleur O, Marceau S, Lebel S, Julien F, et al. Long-term nutritional impact of sleeve gastrectomy. Surg Obes Relat Dis. Elsevier Inc.; 2017;13:1664–75.
Erdogdu UE, Cayci HM, Tardu A, et al. Health literacy and weight loss after bariatric surgery. Obes Surg Obesity Surgery. 2019;29:3948–53.
Gadiot RPM, Biter LU, van Mil S, et al. Long-term results of laparoscopic sleeve gastrectomy for morbid obesity : 5 to 8-year results. Obes Surg [Internet]. Obesity Surgery; 2017;27:59–63. Available from. 2017; https://doi.org/10.1007/s11695-016-2235-8.
Guerreiro V, Neves JS, Salazar D, et al. Long-Term weight loss and metabolic syndrome remission after bariatric surgery: the effect of sex, age, metabolic parameters and surgical technique-a 4-year follow-up study. Obes Facts. 2019;12:639–52.
Johari Y, Ooi G, Burton P, et al. Long-term matched comparison of adjustable gastric banding versus sleeve gastrectomy: weight loss, quality of life, hospital resource use and patient-reported outcome measures. Obes Surg. 2020;30:214–23.
Kansou G, Lechaux D, Delarue J, et al. Laparoscopic sleeve gastrectomy versus laparoscopic mini gastric bypass : one year outcomes. Int J Surg. 2016;33:18–22.
Kim G, Tan CS, Tan KW, et al. Sleeve gastrectomy and Roux-en-Y gastric bypass lead to comparable changes in body composition in a multiethnic asian population. J Gastrointest Surg. 2019;23:445–50.
Makaronidis JM, Neilson S, Cheung W-H, Tymoszuk U, Pucci A, Finer N, et al. Reported appetite , taste and smell changes following Roux-en-Y gastric bypass and sleeve gastrectomy : effect of gender, type 2 diabetes and relationship to post-operative weight loss. Appetite [Internet]. Elsevier Ltd; 2016;107:93–105. Available from: https://doi.org/10.1016/j.appet.2016.07.029
Ricci MA, Ministrini S, De Vuono S, et al. Sleeve gastrectomy efficacy on metabolic and cardiovascular dysfunction with a focus on the role of comorbidities. Angiology. 2018;69:475–82.
Shanti H, Almajali N, Al-Shamaileh T, et al. Helicobacter pylori does not affect postoperative outcomes after sleeve gastrectomy. Obes Surg Obesity Surgery. 2017;27:1298–301.
Tranchart H, Rebibo L, Gaillard M, Dhahri A, Lainas P, Regimbeau JM, et al. Short-term outcomes of single-port versus conventional laparoscopic sleeve gastrectomy: a propensity score matched analysis. Surg Endosc [Internet]. Springer US; 2019; Available from: https://doi.org/10.1007/s00464-019-07175-1
Vigilante A, Signorini F, Marani M, et al. Impact on dyslipidemia after laparoscopic sleeve gastrectomy. Obes Surg Obesity Surgery. 2018;28:311–3115.
Watanabe A, Seki Y, Haruta H, et al. Preoperative weight loss and operative outcome after laparoscopic sleeve gastrectomy. Obes Surg Obesity Surgery. 2017;27:2515–21.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide : baseline demographic description and one-year outcomes from the fourth IFSO Global Registry Report 2018. Obes Surg Obesity Surgery. 2019;29:782–95.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med [Internet]. Elsevier Inc.; 2009;122:248–56. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0002934308010644
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish Obese Subjects. N Engl J Med [Internet]. 2007;357:741–52. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa066254
van de Laar AWJM, Acherman YIZ. Weight loss percentile charts of large representative series: a benchmark defining sufficient weight loss challenging current criteria for success of bariatric surgery. Obes Surg [Internet]. 2013;727–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24234735
van de Laar AW, Nienhuijs SW, Apers JA, et al. The Dutch bariatric weight loss chart: a multicenter tool to assess weight outcome up to 7 years after sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis [Internet]. Elsevier Inc.; 2019;15:200–10. Available from. 2019; https://doi.org/10.1016/j.soard.2018.11.024.
Zhao K, Liu J, Wang M, et al. Safety and efficacy of laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass: a systematic review and meta-analysis. J Eval Clin Pract. 2020;26:290–8.
Yang P, Chen B, **ang S, Lin X-F, Luo F, Li W. Long-term outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for morbid obesity: results from a meta-analysis of randomized controlled trials. Surg Obes Relat Dis. Elsevier Inc.; 2019;15:546–55.
O’Brien PE, Hindle A, Brennan L, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg Obesity Surgery. 2019;29:3–14.
Gu L, Huang X, Li S, et al. A meta-analysis of the medium- and long-term effects of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass. BMC Surg BMC Surgery. 2020;30
Sharples AJ, Mahawar K. Systematic review and meta-analysis of randomised controlled trials comparing long-term outcomes of Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg Obesity Surgery. 2020;30:664–72.
Guraya SY, Strate T. Effectiveness of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity in achieving weight loss outcomes. Int J Surg [Internet]. Elsevier; 2019;70:35–43. Available from. https://doi.org/10.1016/j.ijsu.2019.08.010.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 18.7 kb)
Rights and permissions
About this article
Cite this article
van Rijswijk, AS., van Olst, N., Schats, W. et al. What Is Weight Loss After Bariatric Surgery Expressed in Percentage Total Weight Loss (%TWL)? A Systematic Review. OBES SURG 31, 3833–3847 (2021). https://doi.org/10.1007/s11695-021-05394-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05394-x