Abstract
Background
Laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG) have shown different weight loss results. These differences might be partly due to dum** after LRYGB, forcing sweet eaters to switch to a healthy diet. The Dutch Sweet Eating Questionnaire (DSEQ) is validated to measure sweet eating. This study aims to investigate if sweet eating measured with the DSEQ influences weight loss.
Methods
In this multicenter randomized controlled trial, patients were included between 2013 and 2017 in two Dutch high-volume hospitals, and randomized with a 1:1 ratio between LRYGB and LSG. Primary outcome measure was weight loss. Secondary outcome measure was sweet eating behavior, measured with the DSEQ. Data was collected at baseline, 1 year and 2 years postoperatively.
Results
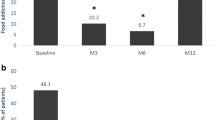
Data was analyzed of 623 patients who underwent LRYGB (n = 308; 49.4%) or LSG (n = 315; 50.6%). Follow-up rates at 2 years postoperative were 67.1% for weight and 35.3% for DSEQ. At 2 years postoperative, mean BMI was significantly higher after LSG than LRYGB (respectively 30.88 versus 28.87 kg/m2, p < 0.001), and the percentage of sweet eaters was significantly higher after LSG than LRYGB (respectively 8.6% versus 2.6%, p = 0.049). None of the preoperative sweet eaters were sweet eaters 2 years after LRYGB (0.0%), versus 11.8% 2 years after LSG. No correlation was found between postoperative sweet eating behavior and %EBMIL.
Conclusion
No significant correlation was found between preoperative or postoperative sweet eating measured with the DSEQ and weight loss. The decision-making for the procedure type is more complex than weight loss and dietary habits, and should also involve quality of life and presence of comorbidities. These factors should be addressed in future research along with longer term results.
Trial Registration
Dutch Trial Register NTR-4741




Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- DSEQ:
-
Dutch sweet eating questionnaire
- EBMIL:
-
Excess body mass index loss
- ERABS:
-
Enhanced recovery after bariatric surgery
- GERD:
-
Gastroesophageal reflux disease
- IFSO:
-
International Federation for the Surgery of Obesity and Metabolic Disorders
- LMWH:
-
Low molecular weight heparin
- LRYGB:
-
Laparoscopic Roux-en-Y gastric bypass
- LSG:
-
Laparoscopic sleeve gastrectomy
- NSE:
-
Non-sweet eaters
- SE:
-
Sweet eaters
- T2D:
-
Type 2 diabetes
- TWL:
-
Total weight loss
- TWOR:
-
Toetsingscommissie wetenschappelijk onderzoek Rotterdam
- VTE:
-
Venous thromboembolic events
References
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Colquitt JL et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;(8):Cd003641.
Zellmer JD et al. Is laparoscopic sleeve gastrectomy a lower risk bariatric procedure compared with laparoscopic Roux-en-Y gastric bypass? A meta-analysis. Am J Surg. 2014;208(6):903–10. discussion 909-10
Gadiot RP, Biter LU, Zengerink HJ, et al. Laparoscopic sleeve gastrectomy with an extensive posterior mobilization: technique and preliminary results. Obes Surg. 2012;22(2):320–9.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. Jama. 2018;319(3):255–65.
Poelemeijer YQM et al. Gastric bypass versus sleeve gastrectomy: patient selection and short-term outcome of 47,101 primary operations from the Swedish, Norwegian, and Dutch National Quality Registries. Ann Surg. 2019;
Fried M et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55.
Sugerman HJ, Starkey JV, Birkenhauer R. A randomized prospective trial of gastric bypass versus vertical banded gastroplasty for morbid obesity and their effects on sweets versus non-sweets eaters. Ann Surg. 1987;205(6):613–24.
Wilson-Perez HE et al. The effect of vertical sleeve gastrectomy on food choice in rats. Int J Obes. 2013;37(2):288–95.
Wijma RB, Emous M, van den Broek M, et al. Prevalence and pathophysiology of early dum** in patients after primary Roux-en-Y gastric bypass during a mixed-meal tolerance test. Surg Obes Relat Dis. 2019;15(1):73–81.
Ahmad A et al. Prevalence of dum** syndrome after laparoscopic sleeve gastrectomy and comparison with laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2019;29(5):1506–13.
Kafri N, Valfer R, Nativ O, et al. Health behavior, food tolerance, and satisfaction after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2011;7(1):82–8.
van den Heuvel M, Hörchner R, Wijtsma A, et al. Sweet eating: a definition and the development of the Dutch Sweet Eating Questionnaire. Obes Surg. 2011;21(6):714–21.
Biter LU et al. The sleeve bypass trial: a multicentre randomized controlled trial comparing the long term outcome of laparoscopic sleeve gastrectomy and gastric bypass for morbid obesity in terms of excess BMI loss percentage and quality of life. BMC Obes. 2015;2:30.
Mannaerts GH, van Mil S, Stepaniak PS, et al. Results of implementing an enhanced recovery after bariatric surgery (ERABS) protocol. Obes Surg. 2016;26(2):303–12.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Angrisani L, di Lorenzo N, Favretti F, et al. The Italian group for LAP-BAND: predictive value of initial body mass index for weight loss after 5 years of follow-up. Surg Endosc. 2004;18(10):1524–7.
Busetto L, Segato G, de Marchi F, et al. Outcome predictors in morbidly obese recipients of an adjustable gastric band. Obes Surg. 2002;12(1):83–92.
Hudson SM, Dixon JB, O’Brien PE. Sweet eating is not a predictor of outcome after lap-band placement. Can we finally bury the myth? Obes Surg. 2002;12(6):789–94.
Korenkov M, Kneist W, Heintz A, et al. Laparoscopic gastric banding as a universal method for the treatment of patients with morbid obesity. Obes Surg. 2004;14(8):1123–7.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319–24.
Sioka E, Tzovaras G, Oikonomou K, et al. Influence of eating profile on the outcome of laparoscopic sleeve gastrectomy. Obes Surg. 2013;23(4):501–8.
Ammon BS, Bellanger DE, Geiselman PJ, et al. Short-term pilot study of the effect of sleeve gastrectomy on food preference. Obes Surg. 2015;25(6):1094–7.
Emous M, Wolffenbuttel BHR, Totté E, et al. The short- to mid-term symptom prevalence of dum** syndrome after primary gastric-bypass surgery and its impact on health-related quality of life. Surg Obes Relat Dis. 2017;13(9):1489–500.
Laurenius A, Engstrom M. Early dum** syndrome is not a complication but a desirable feature of Roux-en-Y gastric bypass surgery. Clin Obes. 2016;6(5):332–40.
Varma S, Clark JM, Schweitzer M, et al. Weight regain in patients with symptoms of post-bariatric surgery hypoglycemia. Surg Obes Relat Dis. 2017;13(10):1728–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the institutional review board (IRB) and the regional Medical Research Ethics Committee TWOR, Rotterdam, the Netherlands (protocol number 2011-48).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Biter, L.U., Leeman, M., Friskes, I. et al. The Prognostic Value of the Dutch Sweet Eating Questionnaire on Weight Loss After Metabolic Surgery: a Randomized Controlled Trial. OBES SURG 30, 2497–2504 (2020). https://doi.org/10.1007/s11695-020-04527-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04527-y