Abstract
Background
Idiopathic intracranial hypertension (IIH) is a serious condition that is frequently associated with irreversibly vision loss, having a higher incidence among obese women. Our aims were to screen subclinical IIH in obese patients scheduled to bariatric surgery using peripapillary retinal nerve fiber layer (RNFL) thickness and to evaluate if the findings demand the possible need of a preoperative evaluation in this population.
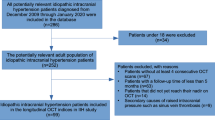
Methods
This study included 111 eyes from 36 obese patients (86% female, body mass index > 35 kg/m2) scheduled to bariatric surgery and 20 non-obese (body mass index < 25 kg/m2) age-matched controls. We measured sectorial and mean RNFL thickness in a 3.5-mm-diameter circular scan centered on the optic nerve head, using optical coherence tomography (Heidelberg Spectralis SD-OCT) in all participants. Multivariate linear regression was used for adjustments.
Results
No patient had subclinical IIH corresponding to increased RNFL thickness. However, in obese individuals, global peripapillary RNFL was thinner than in controls (104 ± 6 μm versus 99 ± 12 μm, p = 0.005). Overall, RNFL thickness was superior in the control group for all sectors. The differences reached significance for the nasal, temporal, superior temporal, and inferior temporal sectors. These differences remained even after adjusting for possible confounders (hypertension, dyslipidemia, diabetes, age, sleep apnea syndrome, and sex).
Conclusions
Routine screening asymptomatic obese patients undergoing bariatric surgery for IIH using RNFL thickness was not clinically relevant in our study. However, we found that severe obesity is associated with neurodegeneration independently of the other components of the metabolic syndrome, what may justify future investigation on the need of monitoring these patients.


Similar content being viewed by others
References
World Health Organization (WHO). Global status report on noncommunicable diseases 2014. 2014.
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet (London, England). 2014;384:766–81.
Oliveira A, Araújo J, Severo M, et al. Prevalence of general and abdominal obesity in Portugal: comprehensive results from the National Food, nutrition and physical activity survey 2015-2016. BMC Public Health. 2018;18:614.
Cefalu WT, Bray GA, Home PD, et al. Advances in the science, treatment, and prevention of the disease of obesity: reflections from a diabetes care editors’ expert forum. Diabetes Care. 2015;38:1567–82.
Cheung N, Wong TY. Obesity and eye diseases. Surv Ophthalmol. 2007;52:180–95.
Andrews LE, Liu GT, Ko MW. Idiopathic intracranial hypertension and obesity. Horm Res Paediatr. 2014;81:217–25.
Bruce BB, Biousse V, Newman NJ. Update on idiopathic intracranial hypertension. Am J Ophthalmol. 2011;152:163–9.
Kilgore KP, Lee MS, Leavitt JA, et al. Re-evaluating the incidence of idiopathic intracranial hypertension in an era of increasing obesity. Ophthalmology. 2017;124:697–700.
Hruby A, Hu FB. The epidemiology of obesity: abig picture Adela. Pharmacoeconomics. 2016;33:673–89.
Ibrahim AM, Ghaferi AA, Thumma JR, et al. Variation in outcomes at bariatric surgery centers of excellence. JAMA Surg. 2017;152:629–36.
Galvin JA, Van Stavern GP. Clinical characterization of idiopathic intracranial hypertension at the Detroit Medical Center. J Neurol Sci. 2004;223:157–60.
Frau J, Fenu G, Signori A, et al. A cross-sectional and longitudinal study evaluating brain volumes, RNFL, and cognitive functions in MS patients and healthy controls. BMC Neurol. 2018;18:67.
Eren Y, Kabatas N, Guven H, Comoglu S, Gurdal C. Evaluation of optic nerve head changes with optic coherence tomography in patients with idiopathic intracranial hypertension. Acta Neurol Belg 2018. https://doi.org/10.1007/s13760-018-1000-2
OCT Sub-Study Committee for NORDIC Idiopathic Intracranial Hypertension Study Group OS-SC for the NIIHS, Auinger P, Durbin M, et al. Baseline OCT measurements in the idiopathic intracranial hypertension treatment trial, part I: quality control, comparisons, and variability. Invest Ophthalmol Vis Sci. 2014;55:8180–8.
Radhakrishnan K, Ahlskog JE, Cross SA, et al. Idiopathic intracranial hypertension (pseudotumor cerebri). Insight. 1993;50:78–80.
Bonomi L, Marchini G, Marraffa M, et al. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology. 2000;107:1287–93.
Vijaya L, Rashima A, Panday M, et al. Predictors for incidence of primary open-angle glaucoma in a south Indian population: the Chennai eye disease incidence study. Ophthalmology. 2014;121:1370–6.
Yamamoto S, Sawaguchi S, Iwase A, et al. Primary open-angle glaucoma in a population associated with high prevalence of primary angle-closure glaucoma: the kumejima study. Ophthalmology. 2014;121:1558–65.
Nangia V, Jonas JB, Matin A, et al. Prevalence and associated factors of glaucoma in rural central India. The Central India Eye and Medical Study. PLoS One. 2013;8:e76434.
Ramdas WD, Wolfs RCW, Hofman A, et al. Lifestyle and risk of develo** open-angle glaucoma. Arch Ophthalmol. 2011;129:767.
Khawaja AP, Chan MPY, Garway-Heath DF, et al. Associations with retinal nerve fiber layer measures in the EPIC-Norfolk Eye Study. Invest Ophthalmol Vis Sci. 2013;54:5028–34.
Zarei R, Anvari P, Eslami Y, et al. Retinal nerve fibre layer thickness is reduced in metabolic syndrome. Diabet Med. 2017;34:1061–6.
Tham Y-C, Cheng C-Y. Associations between chronic systemic diseases and primary open angle glaucoma: an epidemiological perspective. Clin Exp Ophthalmol. 2017;45:24–32.
Shi R, Guo Z, Wang F, et al. Alterations in retinal nerve fiber layer thickness in early stages of diabetic retinopathy and potential risk factors. Curr Eye Res. 2018;43:244–53.
Dogan B, Kazim Erol M, Dogan U, et al. The retinal nerve fiber layer, choroidal thickness, and central macular thickness in morbid obesity: an evaluation using spectral-domain optical coherence tomography. Eur Rev Med Pharmacol Sci. 2016;20:886–91.
Budenz DL, Anderson DR, Varma R, et al. Determinants of normal retinal nerve fiber layer thickness measured by Stratus OCT. Ophthalmology. 2007;114:1046–52.
Ren J, Sowers JR, Zhang Y. Metabolic stress, autophagy, and cardiovascular aging: from pathophysiology to therapeutics. Trends Endocrinol Metab. 2018;29:699–711.
Tsubota K, Kawashima M, Inaba T, et al. The era of antiaging ophthalmology comes of age: antiaging approach for dry eye treatment. Ophthalmic Res. 2010;44:146–54.
Shiba C, Shiba T, Takahashi M, et al. Relationships among serum lipoprotein lipase mass, visceral fat, and retinal nerve fiber layer thickness. Graefes Arch Clin Exp Ophthalmol. 2015;253:1883–8.
Spielman LJ, Little JP, Klegeris A. Inflammation and insulin/IGF-1 resistance as the possible link between obesity and neurodegeneration. J Neuroimmunol. 2014;273:8–21.
Weisberg SP, McCann D, Desai M, et al. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–808.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Laiginhas, R., Guimarães, M., Cardoso, P. et al. Retinal Nerve Fiber Layer Thickness Decrease in Obesity as a Marker of Neurodegeneration. OBES SURG 29, 2174–2179 (2019). https://doi.org/10.1007/s11695-019-03806-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03806-7