Abstract
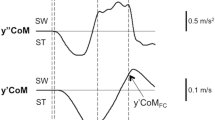
Anxiety and postural control deficits may be related in people with Parkinson’s disease (PwPD). However, the association between anxiety levels and weight-shifting control remains ambiguous. This study investigated whether 1) weight-shifting control differed between PwPD with and without anxiety, and 2) the learning effect of weight-shifting differed between the two populations. Additionally, we evaluated cortical activities to investigate neural mechanisms underlying weight-shifting control. Twenty-eight PwPD (14 anxiety, 14 nonanxiety) participated in a 5-day weight-shifting study by coupling the bearing weight of their more-affected leg to a sinusoidal target at 0.25 Hz. We tested the weight-shifting control on day 1 (pretest), day 3 (posttest), and day 5 (retention test) with a learning session on day 3. The error and jerk of weight-shifting trajectory and the theta and gamma powers of electroencephalography in prefrontal, frontal, sensorimotor and parietal-occipital areas were measured. At the pretest, the anxiety group showed larger error and smaller jerk of weight-shifting with greater prefrontal theta, frontal gamma, and sensorimotor gamma powers than the nonanxiety group. Anxiety intensity was correlated positively with weight-shifting error and theta power but negatively with weight-shifting jerk. Reduced weight-shifting error with increased theta power after weight-shifting learning was observed in the nonanxiety group. However, the anxiety group showed decreased gamma power after weight-shifting learning without behavior change. Our findings suggest differential weight-shifting control and associated cortical activation between PwPD with and without anxiety. In addition, anxiety would deteriorate weight-shifting control and hinder weight-shifting learning benefits in PwPD, leading to less weight-shifting accuracy and correction.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Martens Ehgoetz KA, Lefaivre SC, Beck EN, Chow R, Pieruccini-Faria F, Ellard CG, et al. Anxiety provokes balance deficits that are selectively dopa-responsive in Parkinson’s disease. Neuroscience. 2017;340:436–44. https://doi.org/10.1016/j.neuroscience.2016.11.011.
Wu M, Kim J, Wei F. Facilitating weight shifting during treadmill training improves walking function in humans with spinal cord injury: a randomized controlled pilot study. Am J Phys Med Rehabil. 2018;97(8):585–92. https://doi.org/10.1097/phm.0000000000000927.
Beckley D, Panzer V, Remler M, Ilog L, Bloem B. Clinical correlates of motor performance during paced postural tasks in Parkinson’s disease. J Neurol Sci. 1995;132(2):133–8. https://doi.org/10.1016/0022-510x(95)00130-t.
Rutten S, Vriend C, van der Werf YD, Berendse HW, Weintraub D, van den Heuvel OA. The bidirectional longitudinal relationship between insomnia, depression and anxiety in patients with early-stage, medication-naïve Parkinson’s disease. Parkinsonism Relat Disord. 2017;39:31–6. https://doi.org/10.1016/j.parkreldis.2017.01.015.
Papagno C, Trojano L. Cognitive and behavioral disorders in Parkinson’s disease: an update. I: cognitive impairments. Neurol Sci. 2018;39(2):215–23. https://doi.org/10.1007/s10072-017-3154-8.
Benke T, Bösch S, Andree B. A study of emotional processing in Parkinson’s disease. Brain Cogn. 1998;38(1):36–52. https://doi.org/10.1006/brcg.1998.1013.
Balaban CD, Thayer JF. Neurological bases for balance–anxiety links. J Anxiety Disord. 2001;15(1–2):53–79. https://doi.org/10.1016/s0887-6185(00)00042-6.
Jazaeri SZ, Azad A, Mehdizadeh H, Habibi SA, MandehgaryNajafabadi M, Saberi ZS, et al. The effects of anxiety and external attentional focus on postural control in patients with Parkinson’s disease. PLoS One. 2018;13(2):0192168. https://doi.org/10.1371/journal.pone.0192168.
Souza CdO, Voos MC, Barbosa AF, Chen J, Francato DCV, Milosevic M, et al. Relationship between posturography, clinical balance and executive function in Parkinson’s disease. J Mot Behav. 2019;51(2):212–21. https://doi.org/10.1080/00222895.2018.1458279.
Amir N, Bomyea J. Working memory capacity in generalized social phobia. J Abnorm Psychol. 2011;120(2):504. https://doi.org/10.1037/a0022849.
Foster PS, Drago V, Yung RC, Skidmore FM, Skoblar B, Shenal BV, et al. Anxiety affects working memory only in left hemibody onset Parkinson disease patients. Cogn Behav Neurol. 2010;23(1):14–8. https://doi.org/10.1097/WNN.0b013e3181cc8be9.
Chiviacowsky S, Wulf G, Lewthwaite R, Campos T. Motor learning benefits of self-controlled practice in persons with Parkinson’s disease. Gait Posture. 2012;35(4):601–5. https://doi.org/10.1016/j.gaitpost.2011.12.003.
Ramenzoni VC, Riley MA, Shockley K, Chiu C-YP. Postural responses to specific types of working memory tasks. Gait Posture. 2007;25(3):368–73. https://doi.org/10.1016/j.gaitpost.2006.04.014.
Jensen O, Tesche CD. Frontal theta activity in humans increases with memory load in a working memory task. Eur J Neurosci. 2002;15(8):1395–9. https://doi.org/10.1046/j.1460-9568.2002.01975.x.
Yang CY, Huang CK. Working-memory evaluation based on EEG signals during n-back tasks. J Integr Neurosci. 2018;17(3–4):695–707. https://doi.org/10.3233/**-180096.
Yu SH, Wu RM, Huang CY. Attentional resource associated with visual feedback on a postural dual task in Parkinson’s disease. Neurorehabil Neural Repair. 2020;34(10):891–903. https://doi.org/10.1177/1545968320948071.
Faria MH, Simieli L, Rietdyk S, Penedo T, Santinelli FB, Barbieri FA. (A)symmetry during gait initiation in people with Parkinson’s disease: A motor and cortical activity exploratory study. Front Aging Neurosci. 2023;15:1142540. https://doi.org/10.3389/fnagi.2023.1142540.
Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992;55(3):181–4. https://doi.org/10.1136/jnnp.55.3.181.
Dubois B, Burn D, Goetz C, Aarsland D, Brown RG, Broe GA, et al. Diagnostic procedures for Parkinson’s disease dementia: recommendations from the movement disorder society task force. Mov Disord. 2007;22(16):2314–24. https://doi.org/10.1002/mds.21844.
Post B, van den Heuvel L, van Prooije T, van Ruissen X, van de Warrenburg B, Nonnekes J. Young onset Parkinson’s Disease: a modern and tailored approach. J Parkinsons Dis. 2020;10(s1):S29–36. https://doi.org/10.3233/jpd-202135.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77. https://doi.org/10.1016/s0022-3999(01)00296-3.
Li X, Hamdy R, Sandborn W, Chi D, Dyer A. Long-term effects of antidepressants on balance, equilibrium, and postural reflexes. Psychiatry Res. 1996;63(2–3):191–6. https://doi.org/10.1016/0165-1781(96)02878-8.
Brown LA, Polych MA, Doan JB. The effect of anxiety on the regulation of upright standing among younger and older adults. Gait Posture. 2006;24(4):397–405. https://doi.org/10.1016/j.gaitpost.2005.04.013.
Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192–7. https://doi.org/10.1093/geronj/45.6.m192.
Brauer S, Burns Y, Galley P. Lateral reach: a clinical measure of medio-lateral postural stability. Physiother Res Int. 1999;4(2):81–8. https://doi.org/10.1002/pri.155.
Tantisuwat A, Chamonchant D, Boonyong S. Multi-directional Reach Test: An Investigation of the Limits of Stability of People Aged between 20–79 Years. J Phys Ther Sci. 2014;26(6):877–80. https://doi.org/10.1589/jpts.26.877.
Takahashi T, Ishida K, Yamamoto H, Takata J, Nishinaga M, Doi Y, et al. Modification of the functional reach test: analysis of lateral and anterior functional reach in community-dwelling older people. Arch Gerontol Geriatr. 2006;42(2):167–73. https://doi.org/10.1016/j.archger.2005.06.010.
Hogan N. An organizing principle for a class of voluntary movements. J Neurosci. 1984;4(11):2745–54. https://doi.org/10.1523/JNEUROSCI.04-11-02745.1984.
Maetzler W, Mancini M, Liepelt-Scarfone I, Müller K, Becker C, Van Lummel RC, et al. Impaired trunk stability in individuals at high risk for Parkinson’s disease. PLoS ONE. 2012;7(3):e32240. https://doi.org/10.1371/journal.pone.0032240.
Wang M, Wang J, Cui X, Wang T, Jiang T, Gao F, Cao J. Multidimensional feature optimization based eye blink detection under epileptiform discharges. IEEE Trans Neural Syst Rehabil Eng. 2022;30:905–14. https://doi.org/10.1109/tnsre.2022.3164126.
Mennes M, Wouters H, Vanrumste B, Lagae L, Stiers P. Validation of ICA as a tool to remove eye movement artifacts from EEG/ERP. Psychophysiology. 2010;47(6):1142–50. https://doi.org/10.1111/j.1469-8986.2010.01015.x.
Plöchl M, Ossandón JP, König P. Combining EEG and eye tracking: identification, characterization, and correction of eye movement artifacts in electroencephalographic data. Front Hum Neurosci. 2012;6:278. https://doi.org/10.3389/fnhum.2012.00278.
Takakusaki K. Functional neuroanatomy for posture and gait control. J Mov Disord. 2017;10(1):1–17. https://doi.org/10.14802/jmd.16062.
Jollife IT, Cadima J. Principal component analysis: A review and recent developments. Philos Trans R Soc A Math Phys Eng Sci. 2016;374(2065):20150202. https://doi.org/10.1098/rsta.2015.0202.
Dijkstra BW, Gilat M, Cofré Lizama LE, Mancini M, Bergmans B, Verschueren SMP, Nieuwboer A. Impaired weight-shift amplitude in people with Parkinson’s disease with freezing of gait. J Parkinsons Dis. 2021;11(3):1367–80. https://doi.org/10.3233/jpd-202370.
Yang YR, Lee YY, Cheng SJ, Lin PY, Wang RY. Relationships between gait and dynamic balance in early Parkinson’s disease. Gait Posture. 2008;27(4):611–5. https://doi.org/10.1016/j.gaitpost.2007.08.003.
Maki B, McIlroy W. Influence of arousal and attention on the control of postural sway. J Vestib Res. 1996;6(1):53–9.
Wada M, Sunaga N, Nagai M. Anxiety affects the postural sway of the antero-posterior axis in college students. Neurosci lett. 2001;302(2–3):157–9. https://doi.org/10.1016/s0304-3940(01)01662-7.
Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion. 2007;7(2):336. https://doi.org/10.1037/1528-3542.7.2.336.
Baker K, Rochester L, Nieuwboer A. The effect of cues on gait variability–reducing the attentional cost of walking in people with Parkinson’s disease. Parkinsonism Relat Disord. 2008;14(4):314–20. https://doi.org/10.1016/j.parkreldis.2007.09.008.
Blaauwendraat C, Levy Berg A, Gyllensten AL. One-year follow-up of basic body awareness therapy in patients with posttraumatic stress disorder. A small intervention study of effects on movement quality, PTSD symptoms, and movement experiences. Physiother Theory Pract. 2017;33(7):515–26. https://doi.org/10.1080/09593985.2017.1325957.
Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol. 1994;49(2):M72-84. https://doi.org/10.1093/geronj/49.2.m72.
Carpenter MG, Bloem BR. Postural control in Parkinson patients: a proprioceptive problem? Exp Neurol. 2011;227(1):26–30. https://doi.org/10.1016/j.expneurol.2010.11.007.
Boonstra TA, Schouten AC, van Vugt JP, Bloem BR, van der Kooij H. Parkinson’s disease patients compensate for balance control asymmetry. J Neurophysiol. 2014;112(12):3227–39. https://doi.org/10.1152/jn.00813.2013.
Sheikh M, Azarpazhooh MR, Hosseini HA. Randomized comparison trial of gait training with and without compelled weight-shift therapy in individuals with chronic stroke. Clin Rehabil. 2015;30(11):1088–96. https://doi.org/10.1177/0269215515611467.
Doyon J. Skill learning. Int Rev Neurobiol. 1997;41:273–94. https://doi.org/10.1016/s0074-7742(08)60356-6.
Morenilla L, Márquez G, Sánchez JA, Bello O, López-Alonso V, Fernández-Lago H, et al. Postural stability and cognitive performance of subjects with Parkinson’s disease during a dual-task in an upright stance. Front Psychol. 2020;11:1256. https://doi.org/10.3389/fpsyg.2020.01256.
Graydon MM, Linkenauger SA, Teachman BA, Proffitt DR. Scared stiff: the influence of anxiety on the perception of action capabilities. Cogn Emot. 2012;26(7):1301–15. https://doi.org/10.1080/02699931.2012.667391.
Wulf G, Chiviacowsky S, Lewthwaite R. Altering mindset can enhance motor learning in older adults. Psychol Aging. 2012;27(1):14–21. https://doi.org/10.1037/a0025718.
Raghavachari S, Lisman JE, Tully M, Madsen JR, Bromfield E, Kahana MJ. Theta oscillations in human cortex during a working-memory task: evidence for local generators. J Neurophysiol. 2006;95(3):1630–8. https://doi.org/10.1152/jn.00409.2005.
Klimesch W. EEG alpha and theta oscillations reflect cognitive and memory performance: a review and analysis. Brain Res Brain Res Rev. 1999;29(2–3):169–95. https://doi.org/10.1016/s0165-0173(98)00056-3.
Gebel A, Lehmann T, Granacher U. Balance task difficulty affects postural sway and cortical activity in healthy adolescents. Exp Brain Res. 2020;238(5):1323–33. https://doi.org/10.1007/s00221-020-05810-1.
Maurer U, Brem S, Liechti M, Maurizio S, Michels L, Brandeis D. Frontal midline theta reflects individual task performance in a working memory task. Brain Topogr. 2015;28:127–34. https://doi.org/10.1007/s10548-014-0361-y.
Schmidt B, Kanis H, Holroyd CB, Miltner WH, Hewig J. Anxious gambling: anxiety is associated with higher frontal midline theta predicting less risky decisions. Psychophysiology. 2018;55(10):e13210. https://doi.org/10.1111/psyp.13210.
Rozengurt R, Barnea A, Uchida S, Levy DA. Theta EEG neurofeedback benefits early consolidation of motor sequence learning. Psychophysiology. 2016;53(7):965–73. https://doi.org/10.1111/psyp.12656.
Van Der Cruijsen J, Manoochehri M, Jonker ZD, Andrinopoulou E-R, Frens MA, Ribbers GM, et al. Theta but not beta power is positively associated with better explicit motor task learning. Neuroimage. 2021;240:118373. https://doi.org/10.1016/j.neuroimage.2021.118373.
Tobias S. Test anxiety: Interference, defective skills, and cognitive capacity. Educ Psychol. 1985;20(3):135–42. https://doi.org/10.1207/s15326985ep2003_3.
Müller MM, Keil A, Gruber T, Elbert T. Processing of affective pictures modulates right-hemispheric gamma band EEG activity. Clin Neurophysiol. 1999;110(11):1913–20. https://doi.org/10.1016/s1388-2457(99)00151-0.
Slobounov S, Fukada K, Simon R, Rearick M, Ray W. Neurophysiological and behavioral indices of time pressure effects on visuomotor task performance. Brain Res Cogn Brain Res. 2000;9(3):287–98. https://doi.org/10.1016/s0926-6410(00)00009-4.
Assem M, Hart MG, Coelho P, Romero-Garcia R, McDonald A, Woodberry E, et al. High gamma activity distinguishes frontal cognitive control regions from adjacent cortical networks. Cortex. 2023;159:286–98. https://doi.org/10.1016/j.cortex.2022.12.007.
Crowell AL, Ryapolova-Webb ES, Ostrem JL, Galifianakis NB, Shimamoto S, Lim DA, et al. Oscillations in sensorimotor cortex in movement disorders: an electrocorticography study. Brain. 2012;135(2):615–30. https://doi.org/10.1093/brain/awr332.
Jenkinson N, Kühn AA, Brown P. γ oscillations in the human basal ganglia. Exp Neurol. 2013;245:72–6. https://doi.org/10.1016/j.expneurol.2012.07.005.
Heid C, Mouraux A, Treede R-D, Schuh-Hofer S, Rupp A, Baumgärtner U. Early gamma-oscillations as correlate of localized nociceptive processing in primary sensorimotor cortex. J Neurophysiol. 2020;123(5):1711–26. https://doi.org/10.1152/jn.00444.2019.
Spooner RK, Wiesman AI, Proskovec AL, Heinrichs-Graham E, Wilson TW. Prefrontal theta modulates sensorimotor gamma networks during the reorienting of attention. Hum Brain Mapp. 2020;41(2):520–9. https://doi.org/10.1002/hbm.24819.
Funding
This work was supported by a grant from the National Science and Technology Council, Taiwan (grant no. NSTC 112–2314-B-002–136-MY3).
Author information
Authors and Affiliations
Contributions
Conceptualization: R.M.W. and C.Y.H. Methodology: Y.T.H. and C.Y.H. Formal analysis: Y.T.H. and C.Y.H. Writing-original draft preparation: Y.T.H. and C.Y.H. Writing-review and editing: Y.T.H., R.M.W. and C.Y.H. Funding acquisition: C.Y.H.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in this study were in accordance with the ethical standards of the Helsinki declaration and approved by the National Taiwan University Hospital Research Ethics Committee.
Consent for publication
Not applicable.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Hung, YT., Wu, RM. & Huang, CY. Differentiation in theta and gamma activation in weight-shifting learning between people with parkinson’s disease of different anxiety severities. GeroScience (2024). https://doi.org/10.1007/s11357-024-01236-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-024-01236-7