Abstract
Purpose
Outpatients with hematologic disease often receive red cell transfusion to treat anemia and fatigue. The effect of transfusion on fatigue-related quality of life and how well this effect is sustained has not been quantified. The study aim was to describe the early and sustained impact over 4 weeks of red cells on patient-reported fatigue in outpatients age ≥ 50 receiving transfusion as routine clinical care.
Methods
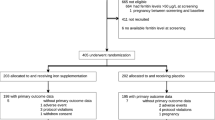
FACIT-Fatigue scale scores were measured pre-transfusion and at visits targeting 3, 7, and 28 days post-transfusion. Group-based trajectory modeling of patient fatigue scores by study day was used to identify the number of distinct trajectories (Groups), then longitudinal mixed effects modeling of fatigue scores was used to estimate group-specific mean improvements early after transfusion and between days 3 and 28 post-transfusion.
Results
Four distinct fatigue score trajectory groups were identified and were found to be correlated with baseline fatigue scores (means 12, 26, 34, and 47 points). In the three groups with the lowest fatigue trajectories (indicating greater fatigue), improvements in fatigue early after transfusion achieved the established minimum clinically important difference (≥ 3 points, Group p = 0.0039). In all trajectory groups, mean fatigue levels did not change significantly between 3 and 28 days (± 1 point, Group p = 0.60).
Conclusion
Patient-reported fatigue varies widely among older adult outpatients with hematologic disorders. Nonetheless, trajectory modeling suggests that most anemic patients can expect a noticeable improvement in fatigue in the first few days after transfusion that generally is sustained up to 4 weeks.



Similar content being viewed by others
References
Cella, D., Lai, J. S., Chang, C. H., Peterman, A., & Slavin, M. (2002). Fatigue in cancer patients compared with fatigue in the general United States population. Cancer, 94(2), 528–538. https://doi.org/10.1002/cncr.10245.
Prochaska, M. T., Newcomb, R., Block, G., Park, B., & Meltzer, D. O. (2017). Association between anemia and fatigue in hospitalized patients: Does the measure of anemia matter? Journal of Hospital Medicine, 12(11), 898–904. https://doi.org/10.12788/jhm.2832.
Cella, D., Kallich, J., McDermott, A., & Xu, X. (2004). The longitudinal relationship of hemoglobin, fatigue and quality of life in anemic cancer patients: Results from five randomized clinical trials. Annals of Oncology, 15(6), 979–986.
Chan, K. L. L., Mak, W. M. V., Tam, Y. H., & Lee, K. K. H. (2018). Factors affecting patient-reported outcomes after red blood cell transfusion in medical patients. Transfusion, 58(1), 158–167. https://doi.org/10.1111/trf.14397.
Prochaska, M. T., Newcomb, R., Jiang, D., & Meltzer, D. O. (2018). The effect of red-blood-cell transfusion on fatigue in hospitalized patients with anaemia. Vox Sanguinis, 113(7), 669–677. https://doi.org/10.1111/vox.12704.
Carson, J. L., Terrin, M. L., Noveck, H., Sanders, D. W., Chaitman, B. R., Rhoads, G. G., et al. (2011). Liberal or restrictive transfusion in high-risk patients after hip surgery. New England Journal of Medicine, 365(26), 2453–2462. https://doi.org/10.1056/NEJMoa1012452.
Prick, B. W., Jansen, A. J., Steegers, E. A., Hop, W. C., Essink-Bot, M. L., Uyl-de Groot, C. A., et al. (2014). Transfusion policy after severe postpartum haemorrhage: A randomised non-inferiority trial. [Multicenter Study Randomized Controlled Trial Research Support, Non-U.S. Gov't]. An International Journal of Obstetrics & Gynaecology, 121(8), 1005–1014.
Brown, E., Hurlow, A., Rahman, A., Closs, S. J., & Bennett, M. I. (2010). Assessment of fatigue after blood transfusion in palliative care patients: A feasibility study. [Validation Studies]. Journal of Palliative Medicine, 13(11), 1327–1330.
St Lezin, E., Karafin, M. S., Bruhn, R., Chowdhury, D., Qu, L., Bialkowski, W., et al. (2019). Therapeutic impact of red blood cell transfusion on anemic outpatients: The RETRO study. Transfusion, 59(6), 1934–1943. https://doi.org/10.1111/trf.15249.
Stanworth, S. J., Killick, S., McQuilten, Z. K., Karakantza, M., Weinkove, R., Smethurst, H., et al. (2020). Red cell transfusion in outpatients with myelodysplastic syndromes: A feasibility and exploratory randomised trial. British Journal of Haematology. https://doi.org/10.1111/bjh.16347.
Cserti-Gazdewich, C. (2018). Shifting ground and gaps in transfusion support of patients with hematological malignancies. Hematology-American Society of Hematology Education Program, 2018(1), 553–560. https://doi.org/10.1182/asheducation-2018.1.553.
Carson, J. L., Grossman, B. J., Kleinman, S., Tinmouth, A. T., Marques, M. B., Fung, M. K., et al. (2012). Red blood cell transfusion: A clinical practice guideline from the AABB*. Annals of Internal Medicine, 157(1), 49–58. https://doi.org/10.7326/0003-4819-157-1-201206190-00429.
Lin, Y., & Buckstein, R. (2019). Outpatient transfusions: Time to study what matters to patients. Transfusion, 59(6), 1887–1890. https://doi.org/10.1111/trf.15382.
Cella, D., Zagari, M. J., Vandoros, C., Gagnon, D. D., Hurtz, H. J., & Nortier, J. W. (2003). Epoetin alfa treatment results in clinically significant improvements in quality of life in anemic cancer patients when referenced to the general population. Journal of Clinical Oncology, 21(2), 366–373. https://doi.org/10.1200/jco.2003.02.136.
Crawford, J., Cella, D., Cleeland, C. S., Cremieux, P. Y., Demetri, G. D., Sarokhan, B. J., et al. (2002). Relationship between changes in hemoglobin level and quality of life during chemotherapy in anemic cancer patients receiving epoetin alfa therapy. Cancer, 95(4), 888–895. https://doi.org/10.1002/cncr.10763.
Nilsson-Ehle, H., Birgegard, G., Samuelsson, J., Antunovic, P., Astermark, J., Garelius, H., et al. (2011). Quality of life, physical function and MRI T2* in elderly low-risk MDS patients treated to a haemoglobin level of %3e/=120 g/L with darbepoetin alfa +/- filgrastim or erythrocyte transfusions. European Journal of Haematology, 87(3), 244–252. https://doi.org/10.1111/j.1600-0609.2011.01654.x.
Bian, J., Chen, B., Hershman, D. L., Marks, N., Norris, L., Schulz, R., et al. (2017). Effects of the US food and drug administration boxed warning of erythropoietin-stimulating agents on utilization and adverse outcome. Journal of Clinical Oncology, 35(17), 1945–1951. https://doi.org/10.1200/jco.2017.72.6273.
Kleinman, S., Busch, M. P., Murphy, E. L., Shan, H., Ness, P., & Glynn, S. A. (2014). The National heart, lung, and blood institute recipient epidemiology and donor evaluation study (REDS-III): A research program striving to improve blood donor and transfusion recipient outcomes. Transfusion, 54(3 Pt 2), 942–955. https://doi.org/10.1111/trf.12468.
Yellen, S. B., Cella, D. F., Webster, K., Blendowski, C., & Kaplan, E. (1997). Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. Journal of Pain and Symptom Management, 13(2), 63–74.
Cella, D., Eton, D. T., Lai, J. S., Peterman, A. H., & Merkel, D. E. (2002). Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. Journal of Pain and Symptom Management, 24(6), 547–561.
Mor, V., Laliberte, L., Morris, J. N., & Wiemann, M. (1984). The karnofsky performance status scale. An examination of its reliability and validity in a research setting. Cancer, 53(9), 2002–2007.
ATS. (2002). ATS statement: Guidelines for the six-minute walk test. American Journal of Respiratory and Critical Care Medicine, 166, 6. https://doi.org/10.1164/rccm.166/1/111.
Nagin, D. S., Jones, B. L., Passos, V. L., & Tremblay, R. E. (2018). Group-based multi-trajectory modeling. Statistical Methods in Medical Research, 27(7), 2015–2023. https://doi.org/10.1177/0962280216673085.
Shi, Q., Mendoza, T. R., Gunn, G. B., Wang, X. S., Rosenthal, D. I., & Cleeland, C. S. (2013). Using group-based trajectory modeling to examine heterogeneity of symptom burden in patients with head and neck cancer undergoing aggressive non-surgical therapy. Quality of Life Research, 22(9), 2331–2339. https://doi.org/10.1007/s11136-013-0380-2.
Hsu, H. C., & Chang, W. C. (2015). Trajectories of frailty and related factors of the older people in Taiwan. Experimental Aging Research, 41(1), 104–114. https://doi.org/10.1080/0361073x.2015.978219.
Druce, K. L., Jones, G. T., Macfarlane, G. J., Verstappen, S. M., & Basu, N. (2015). The longitudinal course of fatigue in rheumatoid arthritis: Results from the Norfolk arthritis register. Journal of Rheumatology, 42(11), 2059–2065. https://doi.org/10.3899/jrheum.141498.
Steensma, D. P., Heptinstall, K. V., Johnson, V. M., Novotny, P. J., Sloan, J. A., Camoriano, J. K., et al. (2008). Common troublesome symptoms and their impact on quality of life in patients with myelodysplastic syndromes (MDS): Results of a large internet-based survey. Leukemia Research, 32(5), 691–698. https://doi.org/10.1016/j.leukres.2007.10.015.
Efficace, F., Gaidano, G., Breccia, M., Criscuolo, M., Cottone, F., Caocci, G., et al. (2015). Prevalence, severity and correlates of fatigue in newly diagnosed patients with myelodysplastic syndromes. British Journal of Haematology, 168(3), 361–370. https://doi.org/10.1111/bjh.13138.
Lacourt, T. E., Kavelaars, A., Ohanian, M., Shah, N. D., Shelburne, S. A., Futreal, A., et al. (2018). Patient-reported fatigue prior to treatment is prognostic of survival in patients with acute myeloid leukemia. Oncotarget, 9(58), 31244–31252. https://doi.org/10.18632/oncotarget.25787.
Roubinian, N. H., & Carson, J. L. (2016). Red blood cell transfusion strategies in adult and pediatric patients with malignancy. Hematology/Oncology Clinics of North America, 30(3), 11. https://doi.org/10.1016/j.hoc.2016.01.001.
Stanworth, S., Killick, S., McQuilten, Z., Karakantza, M., Smethurst, H., Pankhurst, L., et al. (2018). A feasibility randomized trial of red cell transfusion thresholds in myelodysplasia. Blood, 132(Suppl 1), 527–527. https://doi.org/10.1182/blood-2018-99-112949.
Shreay, S., Desrosiers, M. P., Corey-Lisle, P., & Payne, K. (2013). A retrospective study to evaluate the time burden associated with outpatient red blood transfusions indicated for anemia due to concomitantly administered chemotherapy in cancer patients. Supportive Care in Cancer, 21(5), 1335–1340. https://doi.org/10.1007/s00520-012-1671-9.
Acknowledgements
The NHLBI Recipient Epidemiology Donor Evaluation Study-III (REDS-III), domestic component, is the responsibility of the following persons: Hubs: A.E. Mast and J.L. Gottschall, BloodCenter of Wisconsin (BCW), Milwaukee, WI; D.J. Triulzi and J.E. Kiss, The Institute for Transfusion Medicine (ITXM), Pittsburgh, PA; E.L. Murphy and E.M. St. Lezin, University of California, San Francisco (UCSF), and Laboratory Medicine, Department of Veterans Affairs Medical Center, San Francisco, CA; E.L. Snyder, Yale University School of Medicine, New Haven, CT; R.G. Cable, American Red Cross Blood Services, Farmington, CT; Data coordinating center: D.J. Brambilla and M.T. Sullivan, Research Triangle International, Rockville, MD; Central laboratory: M.P. Busch and P.J. Norris, Blood Systems Research Institute, San Francisco, CA; Publication committee chair: R.Y. Dodd, American Red Cross, Holland Laboratory, Rockville, MD; Steering committee chair: S.H. Kleinman, University of British Columbia, Victoria, BC, Canada; National Heart, Lung, and Blood Institute, National Institutes of Health: S.A. Glynn and K.B. Malkin, Bethesda, MD.
Funding
This project is part of the NHLBI Recipient Epidemiology and Donor Evaluation Study-III (REDS-III), which was funded by NHLBI contracts NHLBI HHSN2682011-00001I, -00002I, -00003I, -00004I, -00005I, -00006I, -00007I, -00008I, and -00009I.
Author information
Authors and Affiliations
Consortia
Contributions
RB and ESL drafted the manuscript; ZK and JH performed statistical analyses. All other authors contributed significantly to the study design, data acquisition, or critical interpretation of the analyses. All authors reviewed the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
No authors declare a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bruhn, R., Karafin, M.S., Hilton, J.F. et al. Early and sustained improvement in fatigue-related quality of life following red blood cell transfusion in outpatients. Qual Life Res 29, 2737–2744 (2020). https://doi.org/10.1007/s11136-020-02517-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02517-2