Abstract
Background
Hospital admissions due to fall-related fractures are a major problem in the aging population. Several risk factors have been identified, including drug use. Most studies often retrieved prescription-only drugs from national databases. These are associated with some limitations as they do not always reliably reproduce the complete patient’s active drug list.
Objective
To evaluate the association between the number of FRIDs intake identified by a standardised medication reconciliation process and a fall-related fracture leading to a hospital admission in older adults.
Setting
The first cohort has been recruited from one traumatology ward of a tertiary teaching hospital in Belgium and the second cohort has been recruited from 11 community pharmacies in Belgium.
Method
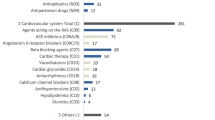
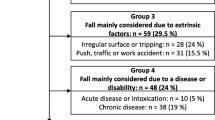
A prospective study with two individually matched cohorts was performed. Adult patients (≥75 years) admitted with an injury due to a fall were included in the first cohort (faller group). The second cohort consisted of patients who did not suffer from a fall within the last 6 months (non-faller group). Matching was performed for age, gender, place of residence and use of a walking aid. In both groups, clinical pharmacists and undergraduate pharmacy students obtained the medication history, using a standardised approach. A list of drugs considered to increase the risk of falling was created. It included cardiovascular drugs and drugs acting on the nervous system. A linear mixed model was used to compare the number of fall risk-increasing drugs between fallers and non-fallers.
Main outcome measure
The number of fall risk-increasing drugs in a faller versus a non-faller group.
Results
Sixty-one patients were matched with 121 non-fallers. Patients received on average 3.1 ± 2.1 and 3.2 ± 1.8 fall risk-increasing drugs in the faller and in the non-faller group, respectively. The mean number of fall risk-increasing drugs was comparable in both groups (p = 0.844), even after adjusting for alcohol consumption, fear of falling, vision and foot problems (p = 0.721).
Conclusion
In a sample of hospitalised patients admitted for a fall-related injury, no significant difference in the number of fall risk-increasing drugs versus that of an outpatient group of non-fallers was found.
Similar content being viewed by others
References
Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am. 2006;90:807–24.
Pohl P, Nordin E, Lundquist A, Bergström U, Lundin-Olsson L. Community-dwelling older people with an injurious fall are likely to sustain new injurious falls within 5 years—a prospective long-term follow-up study. BMC Geriatr. 2014;14:120. doi:10.1186/1471-2318-14-120.
Karlsson MK, Vonschewelov T, Karlsson C, Cöster M, Rosengen BE. Prevention of falls in the elderly: a review. Scand J Public Health. 2013;41:442–54.
Huang AR, Mallet L, Rochefort CM, Eguale T, Buckeridge DL, Tamblyn R. Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging. 2012;29:359–76.
Campbell AJ. Drug treatment as a cause of falls in old age. A review of the offending agents. Drugs Aging. 1991;1:289–302.
Bulat T, Castle SC, Rutledge M, Quigley P. Clinical practice algorithms: medication management to reduce fall risk in the elderly—part 3, benzodiazepines, cardiovascular agents, and antidepressants. J Am Acad Nurse Pract. 2008;20:55–62.
Tannenbaum C, Martin P, Tamblyn R, Benedetti A, Ahmed S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med. 2014;174:890–8.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi:10.1002/14651858.CD007146.pub3.
Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12:CD005465. doi:10.1002/14651858.CD005465.pub3.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47:30–9.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc. 1999;47:40–50.
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–60.
Gribbin J, Hubbard R, Gladman JR, Smith C, Lewis S. Risk of falls associated with antihypertensive medication: population-based case-control study. Age Ageing. 2010;39:592–7.
Gribbin J, Hubbard R, Gladman J, Smith C, Lewis S. Risk of falls associated with antihypertensive medication: self-controlled case series. Pharmacoepidemiol Drug Saf. 2011;20:879–84.
Aung K, Htay T. Thiazide diuretics and the risk of hip fracture. Cochrane Database Syst Rev. 2011;10:CD005185. doi:10.1002/14651858.CD005185.pub2.
Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172:1739–44.
Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of falls on initiation of antihypertensive drugs in the elderly. Osteoporos Int. 2013;24:2649–57.
Lapane KL, Yang S, Brown MJ, Jawahar R, Pagliasotti C, Rajpathak S. Sulfonylureas and risk of falls and fractures: a systematic review. Drugs Aging. 2013;30:527–47.
Bloch F, Thibaud M, Tournoux-Facon C, Brèque C, Rigaud AS, Dugué B, et al. Estimation of the risk factors for falls in the elderly: can meta-analysis provide a valid answer? Geriatr Gerontol Int. 2013;13:250–63.
Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588–95.
Milos V, Bondesson A, Magnusson M, Jakobsson U, Westerlund T, Midlöv P. Fall risk-increasing drugs and falls: a cross-sectional study among elderly patients in primary care. BMC Geriatr. 2014;14:40. doi:10.1186/1471-2318-14-40.
Wiens M, Etminan M, Gill SS, Takkouche B. Effects of antihypertensive drug treatments on fracture outcomes: a meta-analysis of observational studies. J Intern Med. 2006;260:350–62.
Rejnmark L, Vestergaard P, Mosekilde L. Treatment with beta-blockers, ACE inhibitors, and calcium-channel blockers is associated with a reduced fracture risk: a nationwide case-control study. J Hypertens. 2006;24:581–9.
Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173:510–5.
De Winter S, Spriet I, Indevuyst C, Vanbrabant P, Desruelles D, Sabbe M, et al. Pharmacist- versus physician-acquired medication history: a prospective study at the emergency department. Qual Saf Health Care. 2010;19:371–5.
Etchells E, Koo M, Daneman N, McDonald A, Baker M, Matlow A, et al. Comparative economic analyses of patient safety improvement strategies in acute care: a systematic review. BMJ Qual Saf. 2012;21:448–56.
van den Bemt PM, van der Schrieck-de Loos EM, van der Linden C, Theeuwes AM, Pol AG, Dutch CBO WHO High 5 s Study Group. Effect of medication reconciliation on unintentional medication discrepancies in acute hospital admissions of elderly adults: a multicenter study. J Am Geriatr Soc. 2013;61:1262–8.
World Health Organisation (WHO) (2013) Guidelines for ATC classification and DDD assignment (document on the internet). Oslo: WHO collaborating Centre for Drug Statistics Methodology. http://www.whocc.no/filearchive/publications/1_2013guidelines.pdf.
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45.
Qaseem A, Snow V, Shekelle P, Hopkins R Jr, Forciea MA, Owens DK, et al. Pharmacologic treatment of low bone density or osteoporosis to prevent fractures: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;149:404–15.
(2011) Expertisecentrum Val-en fractuurpreventie Vlaanderen. Draaiboek zorgpad valpreventie (document on the internet). Expertisecentrum Val-en fractuurpreventie Vlaanderen. http://www.valpreventie.be/Portals/Valpreventie/Documenten/thuis/EVV_Draaiboek_zorgpad_valpreventie.pdf.
Lindquist LA, Gleason KM, McDaniel MR, Doeksen A, Liss D. Teaching medication reconciliation through simulation: a patient safety initiative for second year medical students. J Gen Intern Med. 2008;23:998–1001.
French DD, Campbell R, Spehar A, Cunningham F, Bulat T, Luther SL. Drugs and falls in community-dwelling older people: a national veterans study. Clin Ther. 2006;28:619–30.
Lamis RL, Kramer JS, Hale LS, Zackula RE, Berg GM. Fall risk associated with inpatient medications. Am J Health Syst Pharm. 2012;69:1888–94.
Kelsey J, Berry SD, Procter-Gray E, Quach L, Nguyen US, Li W, et al. Indoor and outdoor falls in older adults are different: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston Study. J Am Geriatr Soc. 2010;58:2135–41.
Giladi AM, Shauver MJ, Ho A, Zhong L, Kim HM, Chung KC. Variation in the incidence of distal radius fractures in the U.S. elderly as related to slippery weather conditions. Plast Reconstr Surg. 2014;133:321–32.
Echt MA, Samelson EJ, Hannan MT, Dufour AB, Berry SD. Psychotropic drug initiation or increased dosage and the acute risk of falls: a prospective cohort study of nursing home residents. BMC Geriatr. 2013;13:19. doi:10.1186/1471-2318-13-9.
Berry SD, Lee Y, Cai S, Dore DD. Nonbenzodiazepine sleep medication use and hip fractures in nursing home residents. JAMA Intern Med. 2013;173:754–61.
Acknowledgments
We would like to express our special thanks to Prof. Dr. Apr. Gert Laekeman, Clinical Pharmacology and Pharmacotherapy, Dpt Pharmaceutical and Pharmacological Sciences, KU Leuven, for his contribution to this study, to keep this project on track in the community pharmacies and for carefully reading this manuscript. We would like to thank all the collaborating undergraduate pharmacy students and the community pharmacies. Finally, we also want to thank Annouschka Laenen, Leuven Biostatistics and Statistical Bioinformatics Centre, Dpt of Public Health and Primary Care, KU Leuven for the statistical assistance.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Winter, S., Vanwynsberghe, S., Foulon, V. et al. Exploring the relationship between fall risk-increasing drugs and fall-related fractures. Int J Clin Pharm 38, 243–251 (2016). https://doi.org/10.1007/s11096-015-0230-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-015-0230-0