Abstract
Purpose
Non-contact continuous respiratory rate monitoring is preferred for early detection of patient deterioration. However, this technique is under development; a gold standard respiratory monitor has not been established. Therefore, this prospective observational method comparison study aimed to compare the measurement accuracy of a non-contact continuous respiratory rate monitor, a microwave Doppler sensor positioned beneath the mattress, with that of other monitors.
Methods
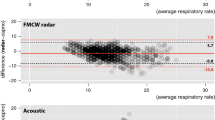
The respiratory rate of intensive care unit patients was simultaneously measured using a microwave Doppler sensor, capnography, thoracic impedance pneumography, and a piezoelectric sensor beneath the mattress. Bias and 95% limits of agreement between the respiratory rate measured using capnography (standard reference) and that measured using the other three methods were calculated using Bland–Altman analysis for repeated measures. Clarke error grid (CEG) analysis evaluated the sensor’s ability to assist in correct clinical decision-making.
Results
Eighteen participants were included, and 2,307 data points were analyzed. The bias values (95% limits of agreement) of the microwave Doppler sensor, thoracic impedance pneumography, and piezoelectric sensor were 0.2 (− 4.8 to 5.2), 1.5 (− 4.4 to 7.4), and 0.4 (− 4.0 to 4.8) breaths per minute, respectively. Clinical decisions evaluated using CEG analyses were correct 98.1% of the time for the microwave Doppler sensor, which was similar to the performance of the other devices.
Conclusion
The microwave Doppler sensor had a small bias but relatively low precision, similar to other devices. In CEG analyses, the risk of each monitor leading to inadequate clinical decision-making was low.
Trial registration number
: UMIN000038900, February 1, 2020.




Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Malycha J, Bonnici T, Clifton DA, Ludbrook G, Young JD, Watkinson PJ. Patient centred variables with univariate associations with unplanned ICU admission: a systematic review. BMC Med Inform Decis Mak. 2019;19:98. https://doi.org/10.1186/s12911-019-0820-1.
Andersen LW, Kim WY, Chase M, Berg KM, Mortensen SJ, Moskowitz A, Novack V, Cocchi MN, Donnino MW. ; American Heart Association’s Get With the Guidelines(®) – Resuscitation Investigators (2016) The prevalence and significance of abnormal vital signs prior to in-hospital cardiac arrest. Resuscitation 98:112–7. https://doi.org/10.1016/j.resuscitation.2015.08.016.
Buist M, Bernard S, Nguyen TV, Moore G, Anderson J. Association between clinically abnormal observations and subsequent in-hospital mortality: a prospective study. Resuscitation. 2004;62:137–41. https://doi.org/10.1016/j.resuscitation.2004.03.005.
Cuthbertson BH, Boroujerdi M, McKie L, Aucott L, Prescott G. Can physiological variables and early warning scoring systems allow early recognition of the deteriorating surgical patient? Crit Care Med. 2007;35:402–9. https://doi.org/10.1097/01.CCM.0000254826.10520.875.
Hillman KM, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, Bishop GF, Simmons G. Antecedents to hospital deaths. Intern Med J. 2001;31:343–8. https://doi.org/10.1046/j.1445-5994.2001.00077.x.
Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified early warning score in medical admissions. QJM. 2001;94:521–6. https://doi.org/10.1093/qjmed/94.10.521.
Jones DA, DeVita MA, Bellomo R. Rapid-Response Teams. N Engl J Med. 2011;365:139–46. https://doi.org/10.1056/NEJMra0910926.
Gao H, McDonnell A, Harrison DA, Moore T, Adam S, Daly K, Esmonde L, Goldhill D, Parry G, Rashidian A, Subbe C, Harvey S. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med. 2007;33:667–79. https://doi.org/10.1007/s00134-007-0532-3.
De Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17:216–23. https://doi.org/10.1136/qshc.2007.023622.
Perman SM, Stanton E, Soar J, Berg RA, Donnino MW, Mikkelsen ME, Edelson DP, Churpek MM, Yang L, Merchant RM, American Heart Association’s Get With the Guidelines®—Resuscitation (formerly the National Registry of Cardiopulmonary Resuscitation) Investigators. Location of in-hospital cardiac arrest in the united states-variability in event rate and outcomes. J Am Heart Assoc. 2016;5:e003638. https://doi.org/10.1161/JAHA.116.003638.
Andersen LW, Berg KM, Chase M, Cocchi MN, Massaro J, Donnino MW. Acute respiratory compromise on inpatient wards in the United States: incidence, outcomes, and factors associated with in-hospital mortality. Resuscitation. 2016;105:123–9. https://doi.org/10.1016/j.resuscitation.2016.05.014.
Leuvan CHV, Mitchell I. Missed opportunities? An observational study of vital sign measurements. Crit Care Resusc. 2008;10:111–5.
Sun L, Joshi M, Khan SN, Ashrafian H, Darzi A. Clinical impact of multi-parameter continuous non-invasive monitoring in hospital wards: a systematic review and meta-analysis. J R Soc Med. 2020;113:217–24. https://doi.org/10.1177/0141076820925436.
Brown H, Terrence J, Vasquez P, Bates DW, Zimlichman E. Continuous monitoring in an inpatient medical-surgical unit: a controlled clinical trial. Am J Med. 2014;127:226–32. https://doi.org/10.1016/j.amjmed.2013.12.004.
Stites M, Surprise J, McNiel J, Northrop D, De Ruyter M. Continuous capnography reduces the incidence of opioid-induced respiratory rescue by hospital rapid resuscitation team. J Patient Saf. 2021;17:e557–61. https://doi.org/10.1097/PTS.0000000000000408.
Brabrand M, Hallas P, Folkestad L, Lautrup-Larsen CH, Brodersen JB. Measurement of respiratory rate by multiple raters in a clinical setting is unreliable: a cross-sectional simulation study. J Crit Care. 2018;44:404–6. https://doi.org/10.1016/j.jcrc.2017.12.020.
Wilkinson JN, Thanawala VU. Thoracic impedance monitoring of respiratory rate during sedation - is it safe? Anaesthesia. 2009;64:455–6. https://doi.org/10.1111/j.1365-2044.2009.05908.x.
Drummond GB, Nimmo AF, Elton RA. Thoracic impedance used for measuring chest wall movement in postoperative patients. Br J Anaesth. 1996;77:327–32. https://doi.org/10.1093/bja/77.3.327.
Mimoz O, Benard T, Gaucher A, Frasca D, Debaene B. Accuracy of respiratory rate monitoring using a non-invasive acoustic method after general anaesthesia. Br J Anaesth. 2012;108:872–5. https://doi.org/10.1093/bja/aer510.
Greenland KB. A potential method for obtaining wave-form capnography during high flow nasal oxygen. Anaesth Intensive Care. 2019;47:204–6. https://doi.org/10.1177/0310057X19836430.
Macknet M, Kimball-Jones P, Applegate R, Martin R, Allard M. Accuracy of a novel bioacoustic sensor for monitoring respiratory rate. Eur J Anaesthesiol. 2007;24:34. https://doi.org/10.1097/00003643-200706001-00124.
Poncette AS, Mosch L, Spies C, Schmieding M, Schiefenhövel F, Krampe H, Balzer F. Improvements in patient monitoring in the intensive care unit: survey study. J Med Internet Res. 2020;22:e19091. https://doi.org/10.2196/19091.
Addison PS, Jacquel D, Foo DMH, Antunes A, Borg UR. Video-based physiologic monitoring during an acute hypoxic challenge: heart rate, respiratory rate, and oxygen saturation. Anesth Analg. 2017;125:860–73. https://doi.org/10.1213/ANE.0000000000001989.
Breteler MJM, KleinJan EJ, Dohmen DAJ, Leenen LPH, van Hillegersberg R, Ruurda JP, van Loon K, Blokhuis TJ, Kalkman CJ. Vital signs monitoring with wearable sensors in high-risk surgical patients a clinical validation study. Anesthesiology. 2020;132:424–39. https://doi.org/10.1097/ALN.0000000000003029.
Tanaka H, Yokose M, Takaki S, Mihara T, Saigusa Y, Goto T. Evaluation of respiratory rate monitoring using a microwave doppler sensor mounted on the ceiling of an intensive care unit: a prospective observational study. J Clin Monit Comput. 2022;36:71–9. https://doi.org/10.1007/s10877-021-00733-w.
Granholm A, Pedersen NE, Lippert A, Petersen LF, Rasmussen LS. Respiratory rates measured by a standardised clinical approach, ward staff, and a wireless device. Acta Anaesthesiol Scand. 2016;60:1444–52. https://doi.org/10.1111/aas.12784.
Bergese SD, Mestek ML, Kelley SD, McIntyre R Jr, Uribe AA, Sethi R, Watson JN, Addison PS. Multicenter study validating accuracy of a continuous respiratory rate measurement derived from pulse oximetry: a comparison with capnography. Anesth Analg. 2017;124:1153–9. https://doi.org/10.1213/ANE.0000000000001852.
Montenij LJ, Buhre WF, Jansen JR, Kruitwagen CL, De Waal EE. Methodology of method comparison studies evaluating the validity of cardiac output monitors: a stepwise approach and checklist. Br J Anaesth. 2016;116:750–8. https://doi.org/10.1093/bja/aew094.
Clarke WL, Cox D, Gonder-Frederick LA, Carter W, Pohl SL. Evaluating clinical accuracy of systems for self-monitoring of blood glucose. Diabetes Care. 1987;10:622–8. https://doi.org/10.2337/diacare.10.5.622.
Parker RA, Weir CJ, Rubio N, Rabinovich R, Pinnock H, Hanley J, McCloughan L, Drost EM, Mantoani LC, MacNee W, McKinstry B. Application of mixed effects limits of agreement in the presence of multiple sources of variability: exemplar from the comparison of several devices to measure respiratory rate in COPD patients. PLoS ONE. 2016;11:e0168321. https://doi.org/10.1371/journal.pone.0168321.
Zimlichman E, Szyper-Kravitz M, Shinar Z, Klap T, Levkovich S, Unterman A, Rozenblum R, Rothschild JM, Amital H, Shoenfeld Y. Early recognition of acutely deteriorating patients in non-intensive care units: Assessment of an innovative monitoring technology. J Hosp Med. 2012;7:628–33. https://doi.org/10.1002/jhm.1963.
Breteler MJM, Huizinga E, van Loon K, Leenen LPH, Dohmen DAJ, Kalkman CJ, Blokhuis TJ. Reliability of wireless monitoring using a wearable patch sensor in high-risk surgical patients at a step-down unit in the Netherlands: a clinical validation study. BMJ Open. 2018;8:e020162. https://doi.org/10.1136/bmjopen-2017-020162.
Clifton L, Clifton DA, Pimentel MAF, Watkinson PJ, Tarassenko L. Predictive monitoring of mobile patients by combining clinical observations with data from wearable sensors. IEEE J Biomed Heal Inform. 2014;18:722–30. https://doi.org/10.1109/JBHI.2013.2293059.
Acknowledgements
None.
Funding
This work was supported by Konica Minolta, Inc. (Tokyo, Japan). The microwave Doppler sensor and piezoelectric sensor used in this study were provided by Konica Minolta, Inc. The company was not involved in the study design, collection, analysis, and interpretation of data, writing of the manuscript, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Hiroyuki Tanaka: Literature search, data collection, analysis of data, manuscript preparation, and manuscript review. Masashi Yokose: Literature search, data collection, study design, analysis of data, manuscript preparation, and review of manuscript.Shunsuke Takaki: Data collection, study design, and review of manuscript.Takahiro Mihara: Study design and review of manuscript.Yusuke Saigusa: Study design, analysis of data, and review of manuscript.Takahisa Goto: Review of manuscript.
Corresponding author
Ethics declarations
Competing interests
Shunsuke Takaki received funding for this study from Konica Minolta, Inc. The other authors have no competing interests to declare.
Ethical approval
This prospective observational study was conducted in accordance with the World Medical Association’s 1964 Declaration of Helsinki and approved by the Institutional Review Board of Yokohama City University Hospital (approval no. B190700013; July 17, 2019).
Consent to participate
Written informed consent was obtained from all participants or their proxies.
Consent to publish
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tanaka, H., Yokose, M., Takaki, S. et al. Measurement accuracy of a microwave doppler sensor beneath the mattress as a continuous respiratory rate monitor: a method comparison study. J Clin Monit Comput 38, 77–88 (2024). https://doi.org/10.1007/s10877-023-01081-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-023-01081-7