Abstract
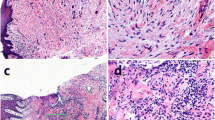
Periodontitis is a chronic inflammatory disease induced by Porphyromonas gingivalis (P. gingivalis) and other pathogens. P. gingivalis release various virulence factors including lipopolysaccharide (LPS). However, whether P. gingivalis–LPS inducing pyroptosis in human gingival fibroblasts (HGFs) remains unknown. In present study, P. gingivalis–LPS decreased the membrane integrity of HGFs, and pyroptosis-associated cytokines were upregulated at the mRNA level. In addition, pyroptosis proteins were highly expressed in gingival tissues of periodontitis. P. gingivalis–LPS induced gingivitis in the rat model, and the expression level of pyroptosis-associated proteins increased. Together, P. gingivalis–LPS can activate the pyroptosis reaction, which may be a pro-pyroptosis status in a relative low concentration.







Similar content being viewed by others
References
Hiranmayi, K.V., K. Sirisha, M.V. Ramoji Rao, and P. Sudhakar. 2017. Novel pathogens in periodontal microbiology. Journal of Pharmacy & Bioallied Sciences 9 (3): 155–163.
Genco, R.J. 1996. Current view of risk factors for periodontal diseases. Journal of Periodontology 67 (10s): 1041–1049.
Dye, B.A. 2011. Global periodontal disease epidemiology. Periodontology 2000 58 (1): 10–25.
Kolenbrander, P.E., R.N. Andersen, D.S. Blehert, P.G. Egland, J.S. Foster, and R.J. Palmer Jr. 2002. Communication among oral bacteria. Microbiology and Molecular Biology Reviews 66 (3): 486–505.
Silva, N., L. Abusleme, D. Bravo, N. Dutzan, J. Garcia-Sesnich, R. Vernal, et al. 2015. Host response mechanisms in periodontal diseases. Journal of Applied Oral Science 23 (3): 329–355.
Kroemer, G., P. Petit, N. Zamzami, J.L. Vayssière, and B. Mignotte. 1995. The biochemistry of programmed cell death. The FASEB Journal 9 (13): 1277–1287.
Elmore, S. 2007. Apoptosis: a review of programmed cell death. Toxicologic Pathology 35 (4): 495–516.
Sgorbissa, A., R. Benetti, S. Marzinotto, C. Schneider, and C. Brancolini. 1999. Caspase-3 and caspase-7 but not caspase-6 cleave Gas2 in vitro: implications for microfilament reorganization during apoptosis. Journal of Cell Science 112 (Pt 23): 4475–4482.
Song, B., T. Zhou, W.L. Yang, J. Liu, and L.Q. Shao. 2017. Programmed cell death in periodontitis: recent advances and future perspectives. Oral Diseases 23 (5): 609–619.
Nagata, S. 2018. Apoptosis and clearance of apoptotic cells. Annual Review of Immunology 36 (1): 489–517.
Vanden Berghe, T., A. Linkermann, S. Jouan-Lanhouet, H. Walczak, and P. Vandenabeele. 2014. Regulated necrosis: the expanding network of non-apoptotic cell death pathways. Nature Reviews. Molecular Cell Biology 15 (2): 135–147.
Someda, M., S. Kuroki, H. Miyachi, M. Tachibana, and S. Yonehara. 2020. Caspase-8, receptor-interacting protein kinase 1 (RIPK1), and RIPK3 regulate retinoic acid-induced cell differentiation and necroptosis. Cell Death and Differentiation 27 (5): 1539–1553.
Li, J., X.J. Ke, F. Yan, L. Lei, and H. Li. 2018. Necroptosis in the periodontal homeostasis: signals emanating from dying cells. Oral Diseases 24 (6): 900–907.
Ke, X., L. Lei, H. Li, H. Li, and F. Yan. 2016. Manipulation of necroptosis by porphyromonas gingivalis in periodontitis development. Molecular Immunology 77: 8–13.
Awad, F., E. Assrawi, C. Louvrier, et al. 2018. Inflammasome biology, molecular pathology and therapeutic implications. Pharmacology & Therapeutics 187: 133–149.
Brodsky, I.E., and D. Monack. 2009. NLR-mediated control of inflammasome assembly in the host response against bacterial pathogens. Seminars in Immunology 21 (4): 199–207.
De Vasconcelos, N.M., N. Van Opdenbosch, H. Van Gorp, E. Parthoens, and M. Lamkanfi. 2019. Single-cell analysis of pyroptosis dynamics reveals conserved GSDMD-mediated subcellular events that precede plasma membrane rupture. Cell Death and Differentiation 26 (1): 146–161.
Liu, X., Z. Zhang, J. Ruan, Y. Pan, V.G. Magupalli, H. Wu, and J. Lieberman. 2016. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature 535 (7610): 153–158.
Yang, J., Y. Zhao, and F. Shao. 2015. Non-canonical activation of inflammatory caspases by cytosolic LPS in innate immunity. Current Opinion in Immunology 32: 78–83.
Liu, J., J. Duan, Y. Wang, and X. Ouyang. 2014. Intracellular adhesion molecule-1 is regulated by Porphyromonas gingivalis through nucleotide binding oligomerization domain-containing proteins 1 and 2 molecules in periodontal fibroblasts. Journal of Periodontology 85 (2): 358–368.
Liu, W., J. Liu, W. Wang, Y. Wang, and X. Ouyang. 2018. NLRP6 induces pyroptosis by activation of caspase-1 in gingival fibroblasts. Journal of Dental Research 97 (12): 1391–1398.
Lamont, R.J., and H.F. Jenkinson. 1998. Life below the gum line: pathogenic mechanisms of Porphyromonas gingivalis. Microbiology and Molecular Biology Reviews 62 (4): 1244–1263.
Fitzsimmons, T.R., S. Ge, and P.M. Bartold. 2017. Compromised inflammatory cytokine response to P. gingivalis LPS by fibroblasts from inflamed human gingiva. Clinical Oral Investigations 22 (2): 919–927.
Li, Y., J. Li, J. Sun, Y. Liu, D. Liu, L. Du, et al. 2020. Expression of RAD51 and its clinical impact in oral squamous cell carcinoma. Analytical Cellular Pathology 2020: 1827676.
Li, Y., Z. Xu, J. Li, S. Ban, C. Duan, and W. Liu. 2018. Interleukin-18 expression in oral squamous cell carcinoma: its role in tumor cell migration and invasion, and growth of tumor cell xenografts. FEBS Open Bio 8 (12): 1953–1963.
Zenobia, C., and G. Hajishengallis. 2015. Porphyromonas gingivalis virulence factors involved in subversion of leukocytes and microbial dysbiosis. Virulence 6 (3): 236–243.
Makkawi, H., S. Hoch, E. Burns, K. Hosur, G. Hajishengallis, C.J. Kirschning, and G. Nussbaum. 2017. Porphyromonas gingivalis stimulates tlr2-pi3k signaling to escape immune clearance and induce bone resorption independently of myd88. Frontiers in Cellular and Infection Microbiology 7: 359.
Derradjia, A., H. Alanazi, H.J. Park, R. Djeribi, A. Semlali, and M. Rouabhia. 2015. α-Tocopherol decreases interleukin-1β and -6 and increases human β-defensin-1 and -2 secretion in human gingival fibroblasts stimulated with porphyromonas gingivalis lipopolysaccharide. Journal of Periodontal Research 51 (3): 295–303.
Márton, I.J., and C. Kiss. 2014. Overlap** protective and destructive regulatory pathways in apical periodontitis. Journal of Endodontia 40 (2): 155–163.
Novak, M.J., H.M. Albather, and J.M. Close. 2008. Redefining the biologic width in severe, generalized, chronic periodontitis: Implications for therapy. Journal of Periodontology 79 (10): 1864–1869.
Graham-Engeland, J.E., N.L. Sin, J.M. Smyth, D.R. Jones, E.L. Knight, M.J. Sliwinski, and C.G. Engeland. 2018. Negative and positive affect as predictors of inflammation: timing matters. Brain, Behavior, and Immunity 74: 222–230.
Hu, J., X. Liu, J. Zhao, et al. 2019. Identification of pyroptosis inhibitors that target a reactive cysteine in gasdermin D. Cancer Immunology Research 7 (2): A132.
Shi, J., W. Gao, and F. Shao. 2017. Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends in Biochemical Sciences 42 (4): 245–254.
Mulhall, H.J., A. Cardnell, K.F. Hoettges, F.H. Labeed, and M.P. Hughes. 2015. Apoptosis progression studied using parallel dielectrophoresis electrophysiological analysis and flow cytometry. Integrative Biology 7 (11): 1396–1401.
Brentnall, M., L. Rodriguez-Menocal, R.L. De Guevara, E. Cepero, and L.H. Boise. 2013. Caspase-9, caspase-3 and caspase-7 have distinct roles during intrinsic apoptosis. BMC Cell Biology 14 (1): 32.
**ang, H., F. Zhu, Z. Xu, and J. **ong. 2020. Role of inflammasomes in kidney diseases via both canonical and non-canonical pathways. Frontiers in Cell and Development Biology 27 (8): 106.
Vande, W.L., and M. Lamkanfi. 2016. Pyroptosis. Curr Biol, 2016 26 (13): R568–R572.
Sborgi, L., S. Rühl, E. Mulvihill, J. Pipercevic, R. Heilig, H. Stahlberg, and S. Hiller. 2016. GSDMD membrane pore formation constitutes the mechanism of pyroptotic cell death. The EMBO Journal 35 (16): 1766–1778.
He, W.T., H. Wan, L. Hu, P. Chen, X. Wang, Z. Huang, Z.H. Yang, C.Q. Zhong, and J. Han. 2015. Gasdermin D is an executor of pyroptosis and required for interleukin-1β secretion. Cell Research 25 (12): 1285–1298.
Kayagaki, N., I.B. Stowe, B.L. Lee, K. O’Rourke, K. Anderson, S. Warming, T. Cuellar, B. Haley, M. Roose-Girma, Q.T. Phung, P.S. Liu, J.R. Lill, H. Li, J. Wu, S. Kummerfeld, J. Zhang, W.P. Lee, S.J. Snipas, G.S. Salvesen, L.X. Morris, L. Fitzgerald, Y. Zhang, E.M. Bertram, C.C. Goodnow, and V.M. Dixit. 2015. Caspase-11 cleaves gasdermin D for non-canonical inflammasome signalling. Nature 526 (7575): 666–671.
Polito, L., M. Bortolotti, M. Pedrazzi, D. Mercatelli, M.G. Battelli, and A. Bolognesi. 2016. Apoptosis and necroptosis induced by stenodactylin in neuroblastoma cells can be completely prevented through caspase inhibition plus catalase or necrostatin-1. Phytomedicine 23 (1): 32–41.
Fritsch, M., and Saskia D Günther, Schwarzer R, et al. 2019. Caspase-8 is the molecular switch for apoptosis, necroptosis and pyroptosis. Nature 575 (7784): 1–5.
Chiquet, M., C. Katsaros, and D. Kletsas. 2015. Multiple functions of gingival and mucoperiosteal fibroblasts in oral wound healing and repair. Periodontology 2000 68 (1): 21–40.
Tipton, D.A., A.A. Hatten, J.P. Babu, and MKh Dabbous. 2015. Effect of glycated albumin and cranberry components on interleukin-6 and matrix metalloproteinase-3 production by human gingival fibroblasts. Journal of Periodontal Research 51 (2): 228–236.
Bozkurt, S.B., S.S. Hakki, E.E. Hakki, Y. Durak, and A. Kantarci. 2016. Porphyromonas gingivalis lipopolysaccharide induces a pro-inflammatory human gingival fibroblast phenotype. Inflammation 40 (1): 144–153.
Jian-Yu, Gu, Yu-Jie Liu, **ang-Qing Zhu, Jia-Ying Qiu, and Ying Sun. 2020. Effects of endotoxin tolerance induced by Porphyromonas gingivalis lipopolysaccharide on inflammatory responses in neutrophils. Inflammation 43 (5): 1692–1706.
Jung, Y.J., H.K. Jun, and B.K. Choi. 2015. Contradictory roles of Porphyromonas gingivalis gingipains in caspase-1 activation. Cellular Microbiology 17 (9): 1304–1319.
Fleetwood, A.J., M.K.S. Lee, W. Singleton, A. Achuthan, M.C. Lee, N.M. O'Brien-Simpson, et al. 2017. Metabolic remodeling, Inflammasome activation, and pyroptosis in macrophages stimulated by Porphyromonas gingivalis and its outer membrane vesicles. Frontiers in Cellular and Infection Microbiology 4 (7): 351.
Cheng, R., W. Liu, R. Zhang, Y. Feng, N.A. Bhowmick, and T. Hu. 2017. Porphyromonas gingivalis-derived lipopolysaccharide combines hypoxia to induce caspase-1 activation in periodontitis. Frontiers in Cellular and Infection Microbiology 14 (7): 474.
Li, Y.Y., B.S. Li, W.W. Liu, Q. Cai, H.Y. Wang, Y.Q. Liu, Y.J. Liu, and W.Y. Meng. 2020. Effects of D-arginine on Porphyromonas gingivalis biofilm. Journal of Oral Science 62 (1): 57–61.
Funding
The study was supported by the grant from the Finance Department of Jilin Province (JCSZ2019378-3; JCSZ2020304-24) and the grants from the Department of Science and Technology of Jilin Province (20180101121JC; 20200404108YY).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, YY., Cai, Q., Li, BS. et al. The Effect of Porphyromonas gingivalis Lipopolysaccharide on the Pyroptosis of Gingival Fibroblasts. Inflammation 44, 846–858 (2021). https://doi.org/10.1007/s10753-020-01379-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-020-01379-7