Abstract
Purpose
This study examines the hepatic extracellular volume fraction (ECV) disparity between the left and right lobes (ECV_left and ECV_right) in patients with chronic thromboembolic pulmonary hypertension (CTEPH), its association with right heart catheterization (RHC) metrics, and with intolerance to increased pulmonary hypertension (PH)-targeted medication dosages.
Methods
We retrospectively analyzed 72 CTEPH-diagnosed patients who underwent equilibrium-phase abdominal dual-energy CT (DECT) and RHC. Hepatic ECVs, derived from DECT’s iodine maps using circular regions of interest in the liver and aorta, were correlated with RHC parameters via Spearman’s rank correlation and lobe differences through the Wilcoxon signed-rank test. Logistic regression assessed cases with ECV_left exceeding ECV_right by > 0.05, while receiver operating characteristic curve analysis gauged ECVs’ predictive power for medication intolerance.
Results
Of the 72 patients (57 females; median age 69), ECV_total (0.24, IQR 0.20–0.27) moderately correlated with RHC parameters (rs = 0.28, −0.24, 0.3 for mean pulmonary arterial pressure, cardiac index [CI], and pulmonary vascular resistance index, respectively). ECV_left significantly surpassed ECV_right (0.25 vs. 0.22, p < 0.001), with a greater ECV_left by > 0.05 indicating notably lower CI (p < 0.001). In 27 patients on PH medication, ECV_left effectively predicted medication intolerance (AUC = 0.84).
Conclusion
In CTEPH patients, hepatic ECV correlated with RHC metrics, where elevated left lobe ECV suggested reduced CI and potential medication intolerance.
Graphical Abstract
The hepatic extracellular volume fraction (ECV), measured via dual-energy CT, was notably higher in the left lobe compared to the right in patients with chronic thromboembolic pulmonary hypertension, with elevated ECV in the left lobe correlating with reduced cardiac index and intolerance to medication.






Similar content being viewed by others
Abbreviations
- CTEPH:
-
Chronic thromboembolic pulmonary hypertension
- CI:
-
Cardiac index
- ECV:
-
Extracellular volume fraction
- DECT:
-
Dual-energy computed tomography
- PH:
-
Pulmonary hypertension
- RHC:
-
Right heart catheterization
- LR:
-
Left-right
- IQR:
-
Interquartile range
- ROC:
-
Receiver operating characteristic curve
- AUC:
-
Areas under the ROC
References
Møller S, Bernardi M (2013) Interactions of the heart and the liver. Eur Heart J 34:2804–2811. https://doi.org/10.1093/eurheartj/eht246
Xanthopoulos A, Starling RC, Kitai T, Triposkiadis F (2019) Heart failure and liver disease: cardiohepatic interactions. JACC Heart Fail 7:87–97. https://doi.org/10.1016/j.jchf.2018.10.007
Rosenkranz S, Howard LS, Gomberg-Maitland M, Hoeper MM (2020) Systemic consequences of pulmonary hypertension and right-sided heart failure. Circulation 141:678–693. https://doi.org/10.1161/CIRCULATIONAHA.116.022362
Dai DF, Swanson PE, Krieger EV et al (2014) Congestive hepatic fibrosis score: a novel histologic assessment of clinical severity. Mod Pathol 27:1552–1558. https://doi.org/10.1038/modpathol.2014.79
Louie CY, Pham MX, Daugherty TJ et al (2015) The liver in heart failure: a biopsy and explant series of the histopathologic and laboratory findings with a particular focus on pre-cardiac transplant evaluation. Mod Pathol 28:932–943. https://doi.org/10.1038/modpathol.2015.40
Nickel NP, Galura GM, Zuckerman MJ et al (2021) Liver abnormalities in pulmonary arterial hypertension. Pulm Circ 11:1–12. https://doi.org/10.1177/20458940211054304
Dolan RS, Stillman AE, Davarpanah AH (2022) Feasibility of hepatic T1-map** and extracellular volume quantification on routine cardiac magnetic resonance imaging in patients with infiltrative and systemic disorders. Acad Radiol 29:S100–S109. https://doi.org/10.1016/j.acra.2021.09.018
Guo J, Wang L, Wang J et al (2022) Prognostic value of hepatic native T1 and extracellular volume fraction in patients with pulmonary arterial hypertension. J Am Heart Assoc 11:e026254. https://doi.org/10.1161/JAHA.122.026254
Bogaert J, Claessen G, Dresselaers T et al (2022) Magnetic resonance relaxometry of the liver – a new imaging biomarker to assess right heart failure in pulmonary hypertension. J Heart Lung Transplant 41:86–94. https://doi.org/10.1016/j.healun.2021.09.005
Ramachandran P, Serai SD, Veldtman GR et al (2019) Assessment of liver T1 map** in fontan patients and its correlation with magnetic resonance elastography-derived liver stiffness. Abdom Radiol (NY) 44:2403–2408. https://doi.org/10.1007/s00261-019-01990-9
Sofue K, Tsurusaki M, Mileto A et al (2018) Dual-energy computed tomography for non-invasive staging of liver fibrosis: accuracy of iodine density measurements from contrast-enhanced data. Hepatol Res 48:1008–1019. https://doi.org/10.1111/hepr.13205
Marri UK, DasShalimar P et al (2021) Noninvasive staging of liver fibrosis using 5-minute delayed dual-energy CT: comparison with US elastography and correlation with histologic findings. Radiology 298:600–608. https://doi.org/10.1148/radiol.2021202232
Yoon JH, Lee JM, Kim JH et al (2021) Hepatic fibrosis grading with extracellular volume fraction from iodine map** in spectral liver CT. Eur J Radiol 137:109604. https://doi.org/10.1016/j.ejrad.2021.109604
Ozaki K, Ishida T, Ohtani T et al (2021) Assessing the progression of segmental fibrosis in chronic liver disease using extracellular volume fractions. Eur J Radiol 145:110033. https://doi.org/10.1016/j.ejrad.2021.110033
Swietlik EM, Ruggiero A, Fletcher AJ et al (2019) Limitations of resting haemodynamics in chronic thromboembolic disease without pulmonary hypertension. Eur Respir J 53:1801787. https://doi.org/10.1183/13993003.01787-2018
Humbert M, Kovacs G, Hoeper MM et al (2022) 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 43:3618–3731. https://doi.org/10.1093/eurheartj/ehac237
Ghofrani H-A, D’Armini AM, Grimminger F et al (2013) Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med 369:319–329. https://doi.org/10.1056/nejmoa1209657
van Thor MCJ, ten Klooster L, Snijder RJ et al (2019) Long-term clinical value and outcome of riociguat in chronic thromboembolic pulmonary hypertension. IJC Heart Vasc 22:163–168. https://doi.org/10.1016/j.ijcha.2019.02.004
Hill NS, Rahaghi FF, Sood N et al (2017) Individual dose adjustment of riociguat in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Respir Med 129:124–129. https://doi.org/10.1016/j.rmed.2017.05.005
Higuchi S, Horinouchi H, Aoki T et al (2022) Balloon pulmonary angioplasty in the management of chronic thromboembolic pulmonary hypertension. Radiographics 42:1881–1896. https://doi.org/10.1148/rg.210102
Higuchi S, Ota H, Yaoita N et al (2023) Update on the roles of imaging in the management of chronic thromboembolic pulmonary hypertension. J Cardiol 81:297–306. https://doi.org/10.1016/j.jjcc.2022.03.001
Fukuda K, Date H, Doi S et al (2019) Guidelines for the treatment of pulmonary hypertension (JCS 2017/JPCPHS 2017). Circ J 83:842–945. https://doi.org/10.1253/circj.CJ-66-0158
Ghofrani HA, Hoeper MM, Halank M et al (2010) Riociguat for chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension: a phase II study. Eur Respir J 36:792–799. https://doi.org/10.1183/09031936.00182909
Frey R, Becker C, Unger S et al (2016) Assessment of the effects of hepatic impairment and smoking on the pharmacokinetics of a single oral dose of the soluble guanylate cyclase stimulator riociguat (BAY 63–2521). Pulm Circ 6:S5–S14. https://doi.org/10.1086/685015
Callan P, Clark AL (2016) Right heart catheterisation: indications and interpretation. Heart 102:147–157. https://doi.org/10.1136/heartjnl-2015-307786
Johnson PJ, Berhane S, Kagebayashi C et al (2015) Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 33:550–558. https://doi.org/10.1200/JCO.2014.57.9151
Yoshihisa A, Kimishima Y, Kiko T et al (2018) Liver fibrosis marker, 7S domain of collagen type IV, in patients with pre-capillary pulmonary hypertension. Int J Cardiol 258:269–274. https://doi.org/10.1016/j.ijcard.2018.01.138
Taniguchi T, Ohtani T, Kioka H et al (2019) Liver stiffness reflecting right-sided filling pressure can predict adverse outcomes in patients with heart failure. JACC Cardiovasc Imaging 12:955–964. https://doi.org/10.1016/j.jcmg.2017.10.022
Dick BM (1928) “Stream-Lines” in the portal vein: their influence on the selective distribution of blood in the liver. Edinb Med J 35:533–539
Ozaki K, Kozaka K, Kosaka Y et al (2020) Morphometric changes and imaging findings of diffuse liver disease in relation to intrahepatic hemodynamics. Jpn J Radiol 38:833–852. https://doi.org/10.1007/s11604-020-00978-6
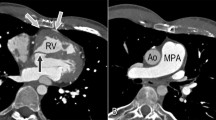
Yamasaki Y, Abe K, Kamitani T et al (2021) Right ventricular extracellular volume with dual-layer spectral detector CT: value in chronic thromboembolic pulmonary hypertension. Radiology 298:589–596. https://doi.org/10.1148/radiol.2020203719
Broncano J, Bhalla S, Gutierrez FR et al (2020) Cardiac MRI in pulmonary hyper-tension: from magnet to bedside. Radiographics 40:982–1002. https://doi.org/10.1148/rg.2020190179
Obmann VC, Berzigotti A, Catucci D et al (2021) T1 map** of the liver and the spleen in patients with liver fibrosis-does normalization to the blood pool increase the predictive value? Eur Radiol 31:4308–4318. https://doi.org/10.1007/s00330-020-07447-8
Acknowledgements
The authors thank CT technologists Yuji Matsuzaki, Shun Okuyama, and Masaki Sakurai for their support in image acquisition and processing, and Editage (https://www.editage.jp/) for English language editing.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Tatsuya Nishii, Hiroki Horinouchi and Takara Namboku. The first draft of the manuscript was written by Tatsuya Nishii and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This retrospective study was approved by the our Institutional Review Board (approval number: R19039-3).
Consent to participate
The requirement for obtaining written informed consent was waived due to the retrospective design of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nishii, T., Horinouchi, H., Namboku, T. et al. Laterality of CT-measured hepatic extracellular volume fraction in patients with chronic thromboembolic pulmonary hypertension. Int J Cardiovasc Imaging (2024). https://doi.org/10.1007/s10554-024-03119-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10554-024-03119-6