Abstract
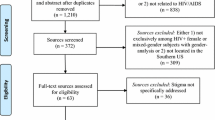
Men living with HIV (MLWH) in sub-Saharan Africa experience poor health outcomes and increased AIDS-related deaths due to stigma influencing testing and treatment uptake and adherence. PRISMA 2020 was used to report a meta-synthesis of the stigma experiences of MLWH in SSA. With the help of an expert librarian, a search of six databases was formulated and performed to examine the available qualitative and mixed method studies with qualitative results relevant to the research question. Studies focused on adult men living with HIV, with five studies specifically examining the HIV experience of men who have sex with men. Study themes were synthesized to describe MLWH’s perceived, internalized, anticipated, enacted, and intersectional stigma experiences. Most studies included masculinity as a key theme that affected both testing and treatment adherence upon diagnosis. Future research is needed to better understand subpopulations, such as men who have sex with men living with HIV, and what interventions may be beneficial to mitigate the disparities among MLWH in SSA.

Similar content being viewed by others
References
Kaiser Family Foundation. The global HIV/AIDS epidemic. KFF. 2022. https://www.kff.org/global-health-policy/fact-sheet/the-global-hivaids-epidemic/. Accessed 13 Nov 2022.
UNAIDS. Fact sheet—latest global and regional statistics on the status of the AIDS epidemic. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2022. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf. Accessed 23 Oct 2022.
West CA, Chang GC, Currie DW, Bray R, Kinchen S, Behel S, McCullough-Sanden R, Low A, Bissek A, Shang JD, Ndongmo CB, Dokubo EK, Balachandra S, Lobognon LR, Dube L, Nuwagaba-Biribonwoha H, Li M, Pasipamire M, Getaneh Y, Lulseged S, Eshetu F, Kingwara L, Zielinski-Gutierrez E, Tlhomola M, Ramphalla P, Kalua T, Auld AF, Williams DB, Remera E, Rwibasira GN, Mugisha V, Malamba SS, Mushi J, Jalloh MF, Mgomella GS, Kirungi WL, Biraro S, Awor AC, Barradas DT, Mugurungi O, Rogers JH, Bronson M, Bodika SM, Ajiboye A, Gaffga N, Moore C, Patel HK, Voetsch AC. Unawareness of HIV infection among men aged 15–59 years in 13 sub-Saharan African countries: findings from the population-based HIV impact assessments, 2015–2019. JAIDS. 2021;87:S97.
UNAIDS. Executive summary—in danger: UNAIDS global AIDS update 2022 [Internet]. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2022. https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update-summary_en.pdf. Accessed 23 Oct 2022.
UNAIDS. Addressing a blind spot in the response to HIV—reaching out to men and boys. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2017. https://www.unaids.org/sites/default/files/media_asset/blind_spot_en.pdf. Accessed 23 Oct 2022.
Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103:813–21. https://doi.org/10.2105/AJPH.2012.301069.
Relf MV, Holzemer WL, Holt L, Nyblade L, Caiola CE. A review of the state of the science of HIV and stigma: context, conceptualization, measurement, interventions, gaps, and future priorities. J Assoc Nurses AIDS Care. 2021;32:392–407. https://doi.org/10.1097/JNC.0000000000000237.
Herek GM. AIDS and stigma. Am Behav Sci. 1999;42:1106–16. https://doi.org/10.1177/00027649921954787.
Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17:1785–95. https://doi.org/10.1007/s10461-013-0437-9.
Derlega VJ, Winstead BA, Greene K, Serovich J, Elwood WN. Perceived HIV-related stigma and HIV disclosure to relationship partners after finding out about the seropositive diagnosis. J Health Psychol. 2002;7:415–32. https://doi.org/10.1177/1359105302007004330.
Arinaitwe I, Amutuhaire H, Atwongyeire D, Tusingwire E, Kawungezi PC, Rukundo GZ, Ashaba S. Social support, food insecurity, and HIV stigma among men living with HIV in rural southwestern Uganda: a cross-sectional analysis. HIV AIDS (Auckl). 2021;13:657–66. https://doi.org/10.2147/HIV.S316174.
Mburu G, Ram M, Siu G, Bitira D, Skovdal M, Holland P. Intersectionality of HIV stigma and masculinity in eastern Uganda: implications for involving men in HIV programmes. BMC Public Health. 2014;14:1061. https://doi.org/10.1186/1471-2458-14-1061.
Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. A sco** review on the role of masculine norms in men’s engagement in the HIV care continuum in sub-Saharan Africa. AIDS Care. 2019;31:1435–46. https://doi.org/10.1080/09540121.2019.1595509.
Abara WE, Garba I. HIV epidemic and human rights among men who have sex with men in sub-Saharan Africa: implications for HIV prevention, care, and surveillance. Glob Public Health. 2017;12:469–82. https://doi.org/10.1080/17441692.2015.1094107.
Joshi K, Lessler J, Olawore O, Loevinsohn G, Bushey S, Tobian AAR, Grabowski MK. Declining HIV incidence in sub-Saharan Africa: a systematic review and meta-analysis of empiric data. J Int AIDS Soc. 2021. https://doi.org/10.1002/jia2.25818.
Nyato D, Kuringe E, Drake M, Casalini C, Nnko S, Shao A, Komba A, Baral SD, Wambura M, Changalucha J. Participants’ accrual and delivery of HIV prevention interventions among men who have sex with men in sub-Saharan Africa: a systematic review. BMC Public Health. 2018. https://doi.org/10.1186/s12889-018-5303-2.
Hamilton A, Thompson N, Choko AT, Hlongwa M, Jolly P, Korte JE, Conserve DF. HIV self-testing uptake and intervention strategies among men in sub-Saharan Africa: a systematic review. Front Public Health. 2021. https://doi.org/10.3389/fpubh.2021.594298.
Hlongwa M, Hlongwana K, Makhunga S, Choko AT, Dzinamarira T, Conserve D, Tsai AC. Linkage to HIV care following HIV self-testing among men: systematic review of quantitative and qualitative studies from six countries in sub-Saharan Africa. AIDS Behav. 2022. https://doi.org/10.1007/s10461-022-03800-8.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021. https://doi.org/10.1136/bmj.n71.
Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. 2017;107:863–9. https://doi.org/10.2105/AJPH.2017.303744.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021.
UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2014. https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf. Accessed 10 June 2023.
UNAIDS. AIDS by the numbers: AIDS is not over, but it can be. Joint United Nations Programme on HIV/AIDS (UNAIDS). 2016. https://www.unaids.org/sites/default/files/media_asset/AIDS-by-the-numbers-2016_en.pdf. Accessed 10 June 2023.
Covidence systematic review software. Veritas Health Innovation. 2022. https://www.covidence.org/. Accessed 8 Mar 2022.
Kmet LM, Lee RC, Cook LS. HTA initiative #13: standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Heritage Foundation for Medical Research. 2004. https://www.ihe.ca/download/standard_quality_assessment_criteria_for_evaluating_primary_research_papers_from_a_variety_of_fields.pdf. Accessed 24 Oct 2022.
Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. New York: Springer Publishing Company; 2007.
Belay YA, Yitayal M, Atnafu A, Taye FA. Patient experiences and preferences for antiretroviral therapy service provision: implications for differentiated service delivery in Northwest Ethiopia. AIDS Res Ther. 2022;19:1–16. https://doi.org/10.1186/s12981-022-00452-5.
Hlongwa M, Jama NA, Mehlomakulu V, Pass D, Basera W, Nicol E. Barriers and facilitating factors to HIV treatment among men in a high-HIV-burdened district in KwaZulu-Natal, South Africa: a qualitative study. Am J Mens Health. 2022. https://doi.org/10.1177/15579883221120987.
Lofgren SM, Tsui S, Atuyambe L, Ankunda L, Komuhendo R, Wamala N, Sadiq A, Kirumira P, Srishyla D, Flynn A, Pastick KA, Meya DB, Nakasujja N, Porta C. Barriers to HIV care in Uganda and implications for universal test-and-treat: a qualitative study. AIDS Care. 2022;34:597–605. https://doi.org/10.1080/09540121.2021.1946000.
Mandawa MB, Mahiti GR. Factors contributing to loss to follow-up from HIV care among men living with HIV/AIDS in Kibaha District, Tanzania. HIV AIDS (Auckl). 2022;14:503–16. https://doi.org/10.2147/hiv.S381204.
Mange T, Henderson N, Lukelelo N. ‘After 25 years of democracy we are still stigmatised and discriminated against’ healthcare experiences of HIV-positive older black gay men in a township in South Africa. J Pract Teach Learn. 2022;9:87–100. https://doi.org/10.1921/jpts.v19i1-2.1674.
Mathenjwa M, Khidir H, Milford C, Mosery N, Rambally Greener L, Pratt MC, O’Neil K, Harrison A, Bangsberg DR, Safren SA, Smit JA, Psaros C, Matthews LT. Acceptability of an intervention to promote viral suppression and serostatus disclosure for men living with HIV in South Africa: qualitative findings. AIDS Behav. 2022;26:1–12. https://doi.org/10.1007/s10461-021-03278-w.
Muwanguzi PA, Nelson LE, Ngabirano TD, Kiwanuka N, Osingada CP, Sewankambo NK. Linkage to care and treatment among men with reactive HIV self-tests after workplace-based testing in Uganda: a qualitative study. Front Public Health. 2022. https://doi.org/10.3389/fpubh.2022.650719.
Nabikande S, Namutundu J, Nangendo J, Okello T, Agwang W, Tusabe J, Kabwama SN, Katahoire AR. Men’s late presentation for HIV care in Eastern Uganda: the role of masculinity norms. PLoS ONE. 2022. https://doi.org/10.1371/journal.pone.0277534.
Ndione AG, Procureur F, Senne JN, Cornaglia F, Gueye K, Ndour CT, Lépine A. Sexuality-based stigma and access to care: intersecting perspectives between health care providers and men who have sex with men in HIV care centres in Senegal. Health Policy Plan. 2022;37:587–96. https://doi.org/10.1093/heapol/czac010.
Rich C, Mavhu W, France NF, Munatsi V, Byrne E, Willis N, Nolan A. Exploring the beliefs, experiences and impacts of HIV-related self-stigma amongst adolescents and young adults living with HIV in Harare, Zimbabwe: a qualitative study. PLoS ONE. 2022. https://doi.org/10.1371/journal.pone.0268498.
Hendrickson ZM, Naugle DA, Tibbels N, Dosso A, Van Lith LM, Mallalieu EC, Kamara D, Dailly-Ajavon P, Cisse A, Ahanda KS, Thaddeus S, Babalola S, Hoffman CJ. “You take medications, you live normally”: the role of antiretroviral therapy in mitigating men’s perceived threats of HIV in Côte d’Ivoire. AIDS Behav. 2019;23:2600–9. https://doi.org/10.1007/s10461-019-02614-5.
Naugle DA, Tibbels NJ, Hendrickson ZM, Dosso A, Van Lith LM, Mallalieu EC, Kouadio AM, Kra W, Kamara D, Dailly-Ajavon P, Cissé A, Seifert-Ahanda K, Thaddeus S, Babalola S, Hoffman CJ. Bringing fear into focus: the intersections of HIV and masculine gender norms in Côte d’Ivoire. PLoS ONE. 2019. https://doi.org/10.1371/journal.pone.0223414.
Tibbels NJ, Hendrickson ZM, Naugle DA, Dosso A, Van Lith LM, Mallalieu EC, Kouadio AM, Kra W, Kamara D, Dailly-Ajavon P, Cisse A, Seifert-Ahanda K, Thaddeus S, Babalola S, Hoffmann CJ. Men’s perceptions of HIV care engagement at the facility- and provider-levels: experiences in Cote d’Ivoire. PLoS ONE. 2019. https://doi.org/10.1371/journal.pone.0211385.
Balogun A, Bissell P, Saddiq M. Negotiating access to the Nigerian healthcare system: the experiences of HIV-positive men who have sex with men. Cult Health Sex. 2020;22:233–46. https://doi.org/10.1080/13691058.2019.1582802.
Mukumbang FC. Leaving no man behind: how differentiated service delivery models increase men’s engagement in HIV care. Int J Health Policy Manag. 2021;10:129–40. https://doi.org/10.34172/ijhpm.2020.32.
Ogunbajo A, Kershaw T, Kushwaha S, Boakye F, Wallace-Atiapah N-D, Nelson LE. Barriers, motivators, and facilitators to engagement in HIV care among HIV-infected Ghanaian men who have sex with men (MSM). AIDS Behav. 2018;22:829–39. https://doi.org/10.1007/s10461-017-1806-6.
Okal J, Lango D, Matheka J, Obare F, Ngunu-Gituathi C, Mugambi M, Avina S. “It is always better for a man to know his HIV status”—a qualitative study exploring the context, barriers and facilitators of HIV testing among men in Nairobi, Kenya. PLoS ONE. 2020. https://doi.org/10.1371/journal.pone.0231645.
Okoror TA, Falade CO, Walker EM, Olorunlana A, Anaele A. Social context surrounding HIV diagnosis and construction of masculinity: a qualitative study of stigma experiences of heterosexual HIV positive men in southwest Nigeria. BMC Public Health. 2016;16:507. https://doi.org/10.1186/s12889-016-3165-z.
Sileo KM, Reed E, Kizito W, Wagman JA, Stockman JK, Wanyenze RK, Chemusto H, Musoke W, Mukasa B, Kiene SM. Masculinity and engagement in HIV care among male fisherfolk on HIV treatment in Uganda. Cult Health Sex. 2019;21:774–88. https://doi.org/10.1080/13691058.2018.1516299.
Zissette S, Watt MH, Prose NS, Mntambo N, Moshabela M. “If you don’t take a stand for your life, who will help you?”: men’s engagement in HIV care in KwaZulu-Natal, South Africa. Psychol Men Masc. 2016;17:265–73. https://doi.org/10.1037/men0000025.
Berner-Rodoreda A, Ngwira E, Alhassan Y, Chione B, Dambe R, Bärnighausen T, Phiri S, Taegtmeyer M, Neuhann F. “Deadly”, “fierce”, “shameful”: notions of antiretroviral therapy, stigma and masculinities intersecting men’s life-course in Blantyre, Malawi. BMC Public Health. 2021. https://doi.org/10.1186/s12889-021-12314-2.
Mantell JE, Masvawure TB, Ma**ure M, Apollo T, Gwanzura C, Block L, Bennett E, Preko P, Musuka G, Rabkin M. Engaging men in HIV programmes: a qualitative study of male engagement in community-based antiretroviral refill groups in Zimbabwe. J Int AIDS Soc. 2019. https://doi.org/10.1002/jia2.25403.
Misra S, Mehta HT, Eschliman EL, Rampa S, Poku OB, Wang W-Q, Ho-Foster AR, Mosepele M, Becker TD, Entaile P, Arscott-Mills T, Opondo PR, Blank MB, Yang LH. Identifying “what matters most” to men in Botswana to promote resistance to HIV-related stigma. Qual Health Res. 2021;31:1680–96. https://doi.org/10.1177/10497323211001361.
Mooney AC, Gottert A, Khoza N, Rebombo D, Hove J, Suárez AJ, Twine R, MacPhail C, Treves-Kagan S, Kahn K, Pettifor A, Lippman SA. Men’s perceptions of treatment as prevention in South Africa: implications for engagement in HIV care and treatment. AIDS Educ Prev. 2017;29:274–87. https://doi.org/10.1521/aeap.2017.29.3.274.
Moyo I, Macherera M, Mavhandu-Mudzusi AH. The lived experiences of men who have sex with men when accessing HIV care services in Zimbabwe. Health SA. 2021. https://doi.org/10.4102/hsag.v26i0.1462.
Meskele M, Khuzwayo N, Taylor M. Map** the evidence of intimate partner violence among women living with HIV/AIDS in sub-Saharan Africa: a sco** review. BMJ Open. 2021. https://doi.org/10.1136/bmjopen-2020-041326.
Tenkorang EY, Asamoah-Boaheng M, Owusu AY. Intimate partner violence (IPV) against HIV-positive women in sub-Saharan Africa: a mixed-method systematic review and meta-analysis. Trauma Violence Abuse. 2021;22:1104–28. https://doi.org/10.1177/1524838020906560.
Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. What role do masculine norms play in men’s HIV testing in sub-Saharan Africa?: a sco** review. AIDS Behav. 2018;22:2468–79. https://doi.org/10.1007/s10461-018-2160-z.
Naanyu V, Ruff J, Goodrich S, Spira T, Bateganya M, Toroitich-Ruto C, Otieno-Nyunya B, Siika AM, Wools-Kaloustian K. Qualitative exploration of perceived benefits of care and barriers influencing HIV care in trans Nzoia, Kenya. BMC Health Serv Res. 2020. https://doi.org/10.1186/s12913-020-05236-z.
Makoae LN, Seboni NM, Molosiwa K, Moleko M, Human S, Sukati NA, Holzemer WL. The symptom experience of people living with HIV/AIDS in southern Africa. J Assoc Nurses AIDS Care. 2005;16:22–32. https://doi.org/10.1016/j.jana.2005.03.005.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2020. https://doi.org/10.1002/jrsm.1411.
Acknowledgements
The manuscript was supported by the Fogarty International Center/National Institutes of Health through Award Number R21TW011247 (M. Relf, Contact MPI/L. Nyblade, MPI) and the Duke University Center for AIDS Research (CFAR), an NIH funded program (5P30AI064518). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
Research reported in this publication was supported by the Fogarty International Center of the National Institutes for Health under award R21TW012007 and by the Duke Center for AIDS Research, a National Institutes of Health funded program under award number 5P30AI064518. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors on this paper meet the four criteria for authorship as identified by the International Committee of Medical Journal Editors; all authors have contributed to the drafting or been involved in revising it, reviewed the final version of this manuscript before submission, and agree to be accountable for all aspects of the work. Specifically, using the CRediT taxonomy, the specific contribution of each author is as follows: Conceptualization & Methodology: S. Janek, L. Ledbetter, M. Relf. Formal Analysis: S. Hatoum, S. Janek, M. Relf. Funding Acquisition: M. Relf. Investigation: S. Hatoum, S. Janek, L. Ledbetter, M. Relf. Methodology: S. Janek, L. Ledbetter, M. Relf. Project administration: M. Relf. Supervision: M. Relf. Verification: S. Hatoum, S. Janek, M. Relf. Writing—manuscript draft: S. Janek. Writing—review & editing: S. Hatoum, S. Janek, L. Ledbetter, M. Relf.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no real or perceived vested interests related to this article that could be construed as a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Registration The protocol that guided this meta-synthesis was prospectively registered with Prospero (registration ID: CRD42022315871).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Janek, S.E., Hatoum, S., Ledbetter, L. et al. Understanding the Stigma Experience of Men Living with HIV in Sub-Saharan Africa: A Qualitative Meta-synthesis. AIDS Behav (2024). https://doi.org/10.1007/s10461-024-04329-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s10461-024-04329-8