Abstract
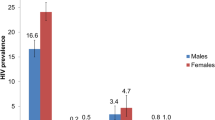
Droughts are associated with poor health outcomes and disruption of public health programming. Data on the association between drought and HIV testing and transmission risk behaviors are limited. We combined data from Demographic and Health Surveys from 10 high HIV prevalence sub-Saharan African countries with a high-resolution measure of drought. We estimated the association between drought and recent HIV testing, report of condomless sex, and number of sexual partners in the last year. Respondents exposed to drought were less likely to have an HIV test and more likely to have condomless sex, although effect sizes were small. We found evidence for effect modification by sex and age for the association between drought and HIV testing, such that the negative association between drought and HIV testing was strongest among men (marginal risk ratio [mRR] 0.92, 95% CI 0.89–0.95) and adolescents (mRR 0.90, 95% CI 0.86–0.93). Drought may hinder HIV testing programs in countries with high HIV prevalence.


Similar content being viewed by others
Data Availability
Demographic and Health Survey data are publicly available at https://dhsprogram.com. CHIRPS precipitation data are publicly available at https://chc.ucsb.edu/data/chirps.
Code Availability
Code is available upon request.
References
Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change. Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693–733.
Feria-Arroyo TP, Castro-Arellano I, Gordillo-Perez G, Cavazos AL, Vargas-Sandoval M, Grover A, et al. Implications of climate change on the distribution of the tick vector Ixodes scapularis and risk for Lyme disease in the Texas-Mexico transboundary region. Parasites and Vectors. 2014;7:1–16.
Erickson RA, Hayhoe K, Presley SM, Allen LJS, Long KR, Cox SB. Potential impacts of climate change on the ecology of dengue and its mosquito vector the Asian tiger mosquito (Aedes albopictus). Environ Res Lett. 2012;7:034003.
Epstein A, Benmarhnia T, Weiser SD. Drought and illness among young children in Uganda, 2009–2012. Am J Trop Med Hyg. 2020;102:644–8.
Tong DQ, Wang JXL, Gill TE, Lei H, Wang B. Intensified dust storm activity and Valley fever infection in the southwestern United States. Geophys Res Lett. 2017;44:4304–12.
Burke M, Gong E, Jones K. Income Shocks and HIV in Africa. Econ J. 2015;125:1157–89.
Armstrong A, Nagata JM, Vicari M, Irvine C, Cluver L, Sohn AH, et al. A Global Research Agenda for Adolescents Living With HIV. J Acquir Immune Defic Syndr. 2018;78(Suppl 1):16–21.
Low AJ, Frederix K, McCracken S, Manyau S, Gummerson E, Radin E, et al. Association between severe drought and HIV prevention and care behaviors in Lesotho: A population-based survey 2016–2017. PLoS Med 2019; 16. doi:https://doi.org/10.1371/journal.pmed.1002727.
Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Heal. 2018;2:223–8.
Hlongwa M, Mashamba-Thompson T, Makhunga S, Hlongwana K. Barriers to HIV testing uptake among men in sub-Saharan Africa: a sco** review. Afr J AIDS Res. 2020;19:13–23.
Camlin CS, Ssemmondo E, Chamie G, El Ayadi AM, Kwarisiima D, Sang N, et al. Men “missing” from population-based HIV testing: insights from qualitative research. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2016;28:67–73.
Wheeler T, Von Braun J. Climate change impacts on global food security. Sci (80- ). 2013;341:508–13.
Stain HJ, Kelly B, Lewin TJ, Higginbotham N, Beard JR, Hourihan F. Social networks and mental health among a farming population. Soc Psychiatry Psychiatr Epidemiol. 2008;43:843–9.
Staniford AK, Dollard MF, Guerin B. Stress and help-seeking for drought-stricken citrus growers in the Riverland of South Australia. Aust J Rural Health. 2009;17:147–54.
Carnie TL, Berry HL, Blinkhorn SA, Hart CR. In their own words: Young people’s mental health in drought-affected rural and remote NSW. Aust J Rural Health. 2011;19:244–8.
Epstein A, Bendavid E, Nash D, Charlebois ED, Weiser SD. Drought and intimate partner violence towards women in 19 countries in sub-saharan Africa during 2011–2018: A population-based study. PLoS Med 2020; 17. doi:https://doi.org/10.1371/JOURNAL.PMED.1003064.
ICF International. Demographic and Health Survey Sampling and Household Listing Manual. 2012.https://dhsprogram.com/pubs/pdf/DHSM4/DHS6_Sampling_Manual_Sept2012_DHSM4.pdf (accessed 19 Apr2021).
UNAIDS. Seizing the moment: Tackling entrenched inequalities to end epidemics. Geneva: ; 2020.
UNAIDS. UNAIDS Report on the Global AIDS Epidemic. Geneva: World Health Organization; 2010. https://www.unaids.org/globalreport/Global_report.htm.
Funk C, Peterson P, Landsfeld M, Pedreros D, Verdin J, Shukla S, et al. The climate hazards infrared precipitation with stations - A new environmental record for monitoring extremes. Sci Data 2015; 2. doi:https://doi.org/10.1038/sdata.2015.66.
Stalter R, Chen M, Uwizeye G, Mutunge E, Ahayo A, Mugwaneza P, et al. Association of sexual risk behaviour with previous HIV testing among voluntary HIV counselling and testing clients in Kigali, Rwanda. Int J STD AIDS. 2016;27:1317–25.
George G, Beckett S, Cawood C, Khanyile D, Govender K, Kharsany ABM. Impact of HIV testing and treatment services on risky sexual behaviour in the uMgungundlovu District, KwaZulu-Natal, South Africa: A cross-sectional study. AIDS Res Ther 2019; 16. doi:https://doi.org/10.1186/s12981-019-0237-z.
Rutstein SO, Johnson K. The DHS wealth index. DHS Comp. Reports No. 6. 2004.http://dhsprogram.com/pubs/pdf/CR6/CR6.pdf (accessed 25 May2021).
Norton EC, Miller MM, Kleinman LC. Computing Adjusted Risk Ratios and Risk Differences in Stata. Stata J Promot Commun Stat Stata. 2013;13:492–509.
StataCorp. Stata Statistical Software: Release 14. 2015.
R Core Team. R: A language and environment for statistical computing. 2017.http://www.r-project.org/.
Food and Agriculture Organization. The impact of disasters on agriculture and food security: FAO in Emergencies. Rome, Italy: ; 2015.
Smirnov O, Zhang M, **ao T, Orbell J, Lobben A, Gordon J. The relative importance of climate change and population growth for exposure to future extreme droughts. Clim Change. 2016;138:41–53.
Chikwari CD, Dringus S, Ferrand RA. Barriers to, and emerging strategies for, HIV testing among adolescents in sub-Saharan Africa. Curr Opin HIV AIDS. 2018;13:257–64.
Awopegba OE, Kalu A, Ahinkorah BO, Seidu AA, Ajayi AI. Prenatal care coverage and correlates of HIV testing in sub-Saharan Africa: Insight from demographic and health surveys of 16 countries. PLoS ONE 2020; 15. doi:https://doi.org/10.1371/journal.pone.0242001.
Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkungu J, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS. 2012;26:67–75.
Young S, Wheeler AC, McCoy SI, Weiser SD. A Review of the Role of Food Insecurity in Adherence to Care and Treatment Among Adult and Pediatric Populations Living with HIV and AIDS. AIDS Behav. 2014;18:505–15.
Leddy AM, Roque A, Sheira LA, Frongillo EA, Landay AL, Adedimeji AA, et al. Food Insecurity Is Associated With Inflammation Among Women Living With HIV. J Infect Dis. 2019;219:429–36.
Weiser SD, Yuan C, Guzman D, Frongillo EA, Riley ED, Bangsberg DR, et al. Food insecurity and HIV clinical outcomes in a longitudinal study of urban homeless and marginally housed HIV-infected individuals. AIDS. 2013;27:2953–8.
Weiser SD, Palar K, Frongillo EA, Tsai AC, Kumbakumba E, dePee S, et al. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS. 2014;28:115–20.
Kalichman SC, Cherry C, Amaral C, White D, Kalichman MO, Pope H, et al. Health and Treatment Implications of Food Insufficiency among People Living with HIV/AIDS, Atlanta, Georgia. J Urban Heal Bull New York Acad Med; 87. doi:https://doi.org/10.1007/s11524-010-9446-4.
Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52:342–9.
Wutich A, Brewis A, Tsai A. Water and mental health. WIREs Water. 2020;7:e1461.
Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ. Food insufficiency, depression, and the modifying role of social support: Evidence from a population-based, prospective cohort of pregnant women in peri-urban South Africa. Soc Sci Med. 2016;151:69–77.
Peltz A, Garg A. Food insecurity and health care use. Pediatrics 2019; 144. doi:https://doi.org/10.1542/peds.2019-0347.
Melo A, Matias MA, Dias SS, Gregório MJ, Rodrigues AM, De Sousa RD, et al. Is food insecurity related to health-care use, access and absenteeism? Public Health Nutr. 2019;22:3211–9.
Thomas MMC, Miller DP, Morrissey TW. Food insecurity and child health. Pediatrics 2019; 144. doi:https://doi.org/10.1542/peds.2019-0397.
Mahmood A, Kim H, Kabir U, Kedia S, Ray M. Food Insecurity and Influenza and Pneumonia Vaccines Uptake Among Community-Dwelling Older Adults in the United States. J Community Health. 2020;45:943–53.
Lankowski AJ, Siedner MJ, Bangsberg DR, Tsai AC. Impact of geographic and transportation-related barriers on HIV outcomes in sub-saharan Africa: A systematic review. AIDS Behav. 2014;18:1199–223.
Stanke C, Kerac M, Prudhomme C, Medlock J, Murray V. Health effects of drought: a systematic review of the evidence. PLoS Curr 2013; 5. doi:https://doi.org/10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b004.
Kloos H. Health aspects of resettlement in Ethiopia. Soc Sci Med. 1990;30:643–56.
Lindvall K, Kinsman J, Abraha A, Dalmar A, Abdullahi MF, Godefay H, et al. Health status and health care needs of drought-related migrants in the horn of africa—a qualitative investigation. Int J Environ Res Public Health. 2020;17:1–18.
Finlay SE, Moffat A, Gazzard R, Baker D, Murray V. Health impacts of wildfires. PLoS Curr 2012; 4. doi:https://doi.org/10.1371/4f959951cce2c.
Mechtenberg A, McLaughlin B, DiGaetano M, Awodele A, Omeeboh L, Etwalu E, et al. Health care during electricity failure: The hidden costs. PLoS ONE. 2020;15:e0235760.
Funding
JMN is supported by the American Heart Association (CDA34760281). AE is supported by the National Institute of Allergy and Infectious Diseases (F31AI150029). SDW is supported by the National Institute of Allergy and Infectious Diseases (K24AI134326).
Author information
Authors and Affiliations
Contributions
AE, JMN, and SDW conceived of the study. AE conducted the data analysis, with input from JMN, EDC and SDW. AE and JMN drafted the manuscript, with support from SDW. All authors contributed to the interpretation of results. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest/Competing Interests
The authors have declared that no competing interests exist.
Ethics Approval
Demographic and Health Surveys obtain informed consent from survey participants and permission to use DHS data was obtained from the DHS program. Specific approval for this de-identified data analysis was not required.
Consent to Participate
N/A.
Consent for Publication
N/A.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Adrienne Epstein and Jason M. Nagata contributed equally to this work.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Epstein, A., Nagata, J.M., Ganson, K.T. et al. Drought, HIV Testing, and HIV Transmission Risk Behaviors: A Population-Based Study in 10 High HIV Prevalence Countries in Sub-Saharan Africa. AIDS Behav 27, 855–863 (2023). https://doi.org/10.1007/s10461-022-03820-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03820-4