Abstract
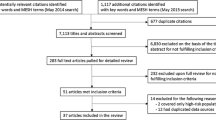
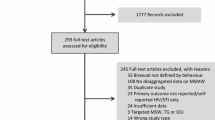
Men who have sex with men (MSM) often change sexual behaviors following HIV diagnosis. This systematic review examined such changes, including sero-adaptive behaviors (i.e., deliberate safer-sex practices to reduce transmission risk) to better understand the magnitude of their association with HIV diagnosis. We searched four databases (1996–2017) and reviewed references from other systematic reviews. We included studies conducted in the United States that compared sexual behavior among HIV-infected “aware” versus “unaware” MSM. We meta-analytically pooled RRs and associated 95% confidence intervals (CI) using random-effects models, and assessed risk of bias and evidence quality. Twenty studies reported k = 131 effect sizes on sexual practices outcomes, most of which reported changes in unprotected sex (k = 85), and on sex with at-risk partners (k = 76); 11 reported sero-adaptive behaviors. Unprotected anal intercourse with an HIV-uninfected/unknown-status partner was less likely among aware MSM (insertive position: k = 2, RR 0.26, 95% CI 0.17, 0.41; receptive position: k = 2, RR 0.53, 95% CI 0.37, 0.77). Risk of not always serosorting among aware MSM (k = 3) was RR = 0.92 (0.83, 1.02). Existing evidence, although low-quality, suggests that HIV-infected MSM tend to adopt safer sexual practices once aware of their diagnosis. Variation in reporting of outcomes limits their comparability. Sero-adaptive behavior data are sparse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who have sex with men (MSM) are the group at greatest risk for HIV infection in the United States (US), comprising more than half of known cases of HIV and an even greater majority (67%) of new HIV infections, according to current surveillance data [1]. Thus, effective HIV prevention strategies targeting MSM are critical to addressing the national burden of HIV. Advances in biomedical HIV prevention strategies stand to protect anyone at risk but in the absence of ideal adherence and efficacy, behavior change remains essential to successful prevention: while uptake of pre-exposure prophylaxis (PrEP) has increased [ Upon request. Not applicable. CDC. Diagnoses of HIV infection in the United States and dependent areas, 2017. Atlanta: Centers for Disease Control and Prevention; 2018. Finlayson T, Cha S, **a M, Trujillo L, Denson D, Prejean J, et al. Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men—20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68(27):597–603. Kanny D, Jeffries WLT, Chapin-Bardales J, Denning P, Cha S, Finlayson T, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(37):801–6. Rodger AJ, Cambiano V, Bruun T, Vernazza P, Collins S, Degen O, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. Lancet (London, England). 2019;393(10189):2428–38. CDC. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 23 US cities, 2017. Atlanta: Centers for Disease Control and Prevention; 2019. Li Z, Purcell DW, Sansom SL, Hayes D, Hall HI. Vital signs: HIV transmission along the continuum of care—United States, 2016. MMWR Morb Mortal Wkly Rep. 2019;68(11):267–72. Crepaz N, Dong X, Wang X, Hernandez AL, Hall HI. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons receiving HIV care—United States, 2014. MMWR Morb Mortal Wkly Rep. 2018;67(4):113–8. Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–53. Vallabhaneni S, Li X, Vittinghoff E, Donnell D, Pilcher CD, Buchbinder SP. Seroadaptive practices: association with HIV acquisition among HIV-negative men who have sex with men. PLoS ONE. 2012;7(10): e45718. Snowden JM, Raymond HF, McFarland W. Prevalence of seroadaptive behaviours of men who have sex with men, San Francisco, 2004. Sex Transm Infect. 2009;85(6):469–76. **a Q, Molitor F, Osmond DH, Tholandi M, Pollack LM, Ruiz JD, et al. Knowledge of sexual partner’s HIV serostatus and serosorting practices in a California population-based sample of men who have sex with men. AIDS. 2006;20(16):2081–9. Parsons JT, Severino J, Nanin J, Punzalan JC, von Sternberg K, Missildine W, et al. Positive, negative, unknown: assumptions of HIV status among HIV-positive men who have sex with men. AIDS Educ Prev. 2006;18(2):139–49. McFarland W, Chen Y-H, Nguyen B, Grasso M, Levine D, Stall R, et al. Behavior, intention or chance? A longitudinal study of HIV seroadaptive behaviors, abstinence and condom use. AIDS Behav. 2012;16(1):121–31. Kennedy CE, Bernard LJ, Muessig KE, Konda KA, Akl EA, Lo YR, et al. Serosorting and HIV/STI infection among HIV-Negative MSM and transgender people: a systematic review and meta-analysis to inform WHO guidelines. J Sex Transm Dis. 2013;2013: 583627. Purcell DW, Higa D, Mizuno Y, Lyles C. Quantifying the harms and benefits from serosorting among HIV-negative gay and bisexual men: a systematic review and meta-analysis. AIDS Behav. 2017;21(10):2835–43. Malekinejad M, Blodgett J, Horvath H, Parriott A, Hutchinson AB, Shrestha R, et al. Change in condom use in populations newly aware of HIV diagnosis in the United States and Canada: a systematic review and meta-analysis. AIDS Behav. 2021;25(6):1839–55. Zakher B, Blazina I, Chou R. Association between knowledge of HIV-positive status or use of antiretroviral therapy and high-risk transmission behaviors: systematic review. AIDS Care. 2014;26(4):514–21. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. The Cochrane Collaboration https://www.cochrane-handbook.org 2011. accessed 18 Sept 2015. Malekinejad M, Barker E, Horvath H, Kahn JG, Jimsheleishvili S. The impact of HIV infection diagnosis on sero-adaptive behaviors in men who have sex with men in the United States: protocol for a systematic review and meta-analysis [Protocol]. PROSPERO International Prospective Register of Systematic Reviews; 2018 https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=85282. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed). 2009;339: b2535. GRADE handbook for grading quality of evidence and strength of recommendations. GRADE Working Group http://www.guidelinedevelopment.org/handbook/ 2013. accessed 21 Jan 2018. EndNote v. X7. Thomson; 2013. Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1. Corp S. Stata Statistical Software: Release 14.2. College Station, TX: StataCorp LP.; 2015. Colfax GN, Buchbinder SP, Cornelisse PGA, Vittinghoff E, Mayer K, Celum C. Sexual risk behaviors and implications for secondary HIV transmission during and after HIV seroconversion. AIDS. 2002;16(11):1529–35. Darrow WW, Webster RD, Kurtz SP, Buckley AK, Patel KI, Stempel RR. Impact of HIV counseling and testing on HIV-infected men who have sex with men: the south beach health survey. AIDS Behav. 1998;2(2):115–26. Vallabhaneni S, McConnell JJ, Loeb L, Hartogensis W, Hecht FM, Grant RM, et al. Changes in seroadaptive practices from before to after diagnosis of recent HIV infection among men who have sex with men. PLoS ONE. 2013;8(2):1–8. Golden MR, Dombrowski JC, Kerani RP, Stekler JD. Failure of serosorting to protect African American men who have sex with men from HIV infection. Sex Transm Dis. 2012;39(9):659–64. McFarland W, Chen YH, Raymond HF, Nguyen B, Colfax G, Mehrtens J, et al. HIV seroadaptation among individuals, within sexual dyads, and by sexual episodes, men who have sex with men, San Francisco, 2008. AIDS Care. 2011;23(3):261–8. Khosropour CM, Dombrowksi JC, Hughes JP, Manhart LE, Golden MR. Evaluation of a computer-based recruitment system for enrolling men who have sex with men into an observational HIV behavioral risk study. Am J Epidemiol. 2016;184(6):477–83. Khosropour CM, Dombrowski JC, Kerani RP, Katz DA, Barbee LA, Golden MR. Changes in condomless sex and serosorting among men who have sex with men after HIV diagnosis. J Acquir Immune Defic Syndr. 2016;73(4):475–81. Steward WT, Remien RH, Higgins JA, Dubrow R, Pinkerton SD, Sikkema KJ, et al. Behavior change following diagnosis with acute/early HIV infection-a move to serosorting with other HIV-infected individuals. the NIMH multisite acute HIV infection study: III. AIDS Behav. 2009;13(6):1054–60. Marks G, Millett GA, Bingham T, Bond L, Lauby J, Liau A, et al. Understanding differences in HIV sexual transmission among Latino and Black men who have sex with men: the Brothers y Hermanos Study. AIDS Behav. 2009;13(4):682–90. Golden MR, Stekler J, Hughes JP, Wood RW. HIV serosorting in men who have sex with men: is it safe. J Acquir Immune Defic Syndr. 2008;49(2):212–8. Moore DM, Kanters S, Michelow W, Gustafson R, Hogg RS, Kwag M, et al. Implications for HIV prevention programs from a serobehavioural survey of men who have sex with men in Vancouver, British Columbia: the ManCount study. Can J Public Health Revue canadienne de santé publique. 2012;103(2):142–6. CDC. Adoption of protective behaviors among persons with recent HIV infection and diagnosis–Alabama, New Jersey, and Tennessee, 1997–1998. MMWR Morb Mortal Wkly Rep. 2000;49(23):512–5. CDC. HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men—United States. MMWR Morb Mortal Wkly Rep. 2013;62(47):958–62. CDC. HIV Infection Risk, Prevention, and Testing Behaviors among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 20 U.S. Cities, 2014. CDC; 2016. Drumright LN, Strathdee SA, Little SJ, Araneta MRG, Slymen DJ, Malcarne VL, et al. Unprotected anal intercourse and substance use before and after HIV diagnosis among recently HIV-infected men who have sex with men. Sex Transm Dis. 2007;34(6):401–7. German D, Sifakis F, Maulsby C, Towe VL, Flynn CP, Latkin CA, et al. Persistently high prevalence and unrecognized HIV infection among men who have sex with men in Baltimore: the Besure study. J Acquir Immune Defic Syndr. 2011;57(1):77–87. Gorbach PM, Weiss RE, Jeffries R, Javanbakht M, Drumright LN, Daar ES, et al. Behaviors of recently HIV-infected men who have sex with men in the year postdiagnosis: Effects of drug use and partner types. J Acquir Immune Defic Syndr. 2011;56(2):176–82. Gorbach PM, Javanbakht M, Bolan RK. Behavior change following HIV diagnosis: findings from a Cohort of Los Angeles MSM. AIDS Care. 2017;197:1–5. McGowan JP, Shah SS, Ganea CE, Blum S, Ernst JA, Irwin KL, et al. Risk behavior for transmission of human immunodeficiency virus (HIV) among HIV-seropositive individuals in an urban setting. Clin Infect Dis. 2004;38(1):122–7. Saah AJ, Hoover DR, Weng S, Carrington M, Mellors J, Rinaldo CR Jr, et al. Association of HLA profiles with early plasma viral load, CD4+ cell count and rate of progression to AIDS following acute HIV-1 infection. Multicenter AIDS Cohort Study AIDS. 1998;12(16):2107–13. Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, et al. HIV prevalence and associated risks in young men who have sex with men. Young Men’s Survey Study Group. JAMA. 2000;284(2):198–204. Whitham HK, Sansom SL, Wejnert C, Finlayson T, Huang YA, An Q, et al. Sex practices by HIV awareness and engagement in the continuum of care among MSM: a national HIV behavioral surveillance analysis in 21 U.S. cities. AIDS Behav. 2018;22(3):840–7. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. This project was funded by the U.S. CDC, National Center for HIV, Viral Hepatitis, STD, and TB Prevention Epidemiologic and Economic Modeling Agreement (NEEMA, # 5U38PS004649). MM was the lead author and supervisor. SJ and EKB conducted record/article screening and data extraction. MM adjudicated disagreements in screening decisions and conduced meta-analysis. ABH, RKS, PV, and JGK provided technical guidance throughout the research project. All authors contributed to manuscript development. The authors declare that they have no conflict of interest. Not required (review). Not required (review). Not applicable. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Below is the link to the electronic supplementary material. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Malekinejad, M., Jimsheleishvili, S., Barker, E.K. et al. Sexual Practice Changes Post-HIV Diagnosis Among Men Who Have Sex with Men in the United States: A Systematic Review and Meta-analysis.
AIDS Behav 27, 257–278 (2023). https://doi.org/10.1007/s10461-022-03761-y Accepted: Published: Issue Date: DOI: https://doi.org/10.1007/s10461-022-03761-yData Availability
Code Availability
References
Acknowledgements
Funding
Author information
Authors and Affiliations
Contributions
Corresponding author
Ethics declarations
Conflict of interest
Ethical Approval
Consent to Participate
Consent for Publication
Additional information
Publisher's Note
Supplementary Information
Rights and permissions
About this article
Cite this article
Keywords