Abstract
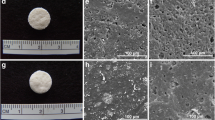
Composites of gatifloxacin (GFLX)-loaded poly (lactic-co-glycolic) acid (PLGA) and β-tricalcium phosphate (βTCP) containing 0, 1, and 10 wt % GFLX (0, 1, and 10 wt % GFLX composites), and GFLX-loaded PLGA containing 1, 5, and 10 wt % GFLX (1, 5, and 10wt % GFLX-PLGA) as controls were fabricated and characterized in vitro and in vivo. On in vitro evaluation, the 10 wt % GFLX composite released GFLX over at least 28 days in Hanks’ balanced solution and exhibited clinically sufficient bactericidal activities against Streptococcus milleri and Bacteroides fragilis from 1 h to 10 days. The 0, 1, and 10 wt % GFLX composites and 10 wt % GFLX-PLGA were implanted in bone defects created by debridement of osteomyelitis lesions induced by S. milleri and B. fragilis in the mandible of rabbits (n = 5). Four weeks after implantation of the 10 wt % GFLX composite, inflammation in the debrided area disappeared in all the rabbits, while inflammation remained in all the rabbits after implantation of the 0 wt % GFLX composite and 10 wt % GFLX-PLGA, and in three rabbits after implantation of the 1 wt % GFLX composite. Bone formation appears to be less intense for the 10 wt % GFLX composite than for the 1 wt % GFLX composite probably owing to the rapid degradation of the 10 wt % GFLX composite. These findings show that the GFLX composite is effective for the local treatment of osteomyelitis.









Similar content being viewed by others
References
Yoshii T, Nishimura H, Yoshikawa T, Furudoi S, Yoshioka A, Takenono I, et al. Therapeutic possibilities of long-term roxithromycin treatment for chronic diffuse sclerosing osteomyelitis of the mandible. J Antimicrobial Chemother. 2001;47:631–7.
Marx RE, Sawatari Y, Fortin M, et al. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63:1567–75.
Migliorati CA, Schubert MM, Peterson DE, Seneda LM. Bisphosphonate-associated osteonecrosis of mandibular and maxillary bone: an emerging oral complication of supportive cancer therapy. Cancer. 2005;104:83–93.
Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527–34.
Wannfors K, Gazelius B. Blood flow in jaw bones affected by chronic osteomyelitis. Br J Oral Maxillofac Surg. 1991;29:147–53.
Coviello V, Stevens MR. Contemporary concepts in the treatment of chronic osteomyelitis. Oral Maxillofac surg Clin North Am. 2007;19(vi):523–34.
Lazzarini L, Mader JT, Calhoun JH. Osteomyelitis in long bones. J Bone Joint surg Am. 2004;86-A:2305–18.
Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364:369–79.
Kluin OS, van der Mei HC, Busscher HJ, Neut D. Biodegradable vs non-biodegradable antibiotic delivery devices in the treatment of osteomyelitis. Expert Opin Drug Deliv. 2013;10:341–51.
Popat KC, Eltgroth M, Latempa TJ, Grimes CA, Desai TA. Decreased Staphylococcus epidermis adhesion and increased osteoblast functionality on antibiotic-loaded titania nanotubes. Biomaterials. 2007;28:4880–8.
Panagopoulos P, Tsaganos T, Plachouras D, Carrer DP, Papadopoulos A, Giamarellou H, et al. In vitro elution of moxifloxacin and fusidic acid by a synthetic crystallic semihydrate form of calcium sulphate (Stimulan). Int J Antimicrob Agents. 2008;32:485–7.
Webb ND, McCanless JD, Courtney HS, Bumgardner JD, Haggard WO. Daptomycin eluted from calcium sulfate appears effective against Staphylococcus. Clin Orthop Relat Res. 2008;466:1383–7.
Gogia JS, Meehan JP, Di Cesare PE, Jamali AA. Local antibiotic therapy in osteomyelitis. Semin Plast Surg. 2009;23:100–7.
Laurencin CT, Gerhart T, Witschger P, Satcher R, Domb A, Rosenberg AE, et al. Bioerodible polyanhydrides for antibiotic drug delivery: in vivo osteomyelitis treatment in a rat model system. J Orthop Res. 1993;11:256–62.
Sinha VR, Bansal K, Kaushik R, Kumria R, Trehan A. Poly-epsilon-caprolactone microspheres and nanospheres: an overview. Int J Pharm. 2004;278:1–23.
Turesin F, Gursel I, Hasirci V. Biodegradable polyhydroxyalkanoate implants for osteomyelitis therapy: in vitro antibiotic release. J Biomater Sci Polym Ed. 2001;12:195–207.
Yenice I, Calis S, Atilla B, Kas HS, Ozalp M, Ekizoglu M, et al. In vitro/in vivo evaluation of the efficiency of teicoplanin-loaded biodegradable microparticles formulated for implantation to infected bone defects. J Microencapsul. 2003;20:705–17.
Abazinge M, Jackson T, Yang Q, Owusu-Ababio G. Comparison of in vitro and in vivo release characteristics of sustained release ofloxacin microspheres. Drug Deliv. 2000;7:77–81.
Koort JK, Makinen TJ, Suokas E, Veiranto M, Jalava J, Knuuti J, et al. Efficacy of ciprofloxacin-releasing bioabsorbable osteoconductive bone defect filler for treatment of experimental osteomyelitis due to Staphylococcus aureus. Antimicrob Agents Chemother. 2005;49:1502–8.
Makinen TJ, Veiranto M, Lankinen P, Moritz N, Jalava J, Tormala P, et al. In vitro and in vivo release of ciprofloxacin from osteoconductive bone defect filler. J Antimicrob Chemother. 2005;56:1063–8.
Zhou J, Fang T, Wang Y, Dong J. The controlled release of vancomycin in gelatin/beta-TCP composite scaffolds. J Biomed Mater Res A. 2012;100:2295–301.
Nelson CL, McLaren SG, Skinner RA, Smeltzer MS, Thomas JR, Olsen KM. The treatment of experimental osteomyelitis by surgical debridement and the implantation of calcium sulfate tobramycin pellets. J Orthopaed Res. 2002;20:643–7.
Miyai T, Ito A, Tamazawa G, Matsuno T, Sogo Y, Nakamura C, et al. Antibiotic-loaded poly-epsilon-caprolactone and porous beta-tricalcium phosphate composite for treating osteomyelitis. Biomaterials. 2008;29:350–8.
Tamazawa G, Ito A, Miyai T, Matsuno T, Kitahara K, Sogo Y, et al. Gatifloxacine-loaded PLGA and beta-tricalcium phosphate composite for treating osteomyelitis. Dent Mater J. 2011;30:264–73.
Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;45:493–6.
Satoh T, Heimdahl A. Study on the formation of experimental infected rabbit. Shigaku. 1989;76:1520–6 (in Japanese with abstract in English).
Satoh TYM, Abe A, Ishigaki Y, Miyasaka T, Adachi M. Transfer of a new quinolone, fleroxacin, to the oral tissues of experimentally infected rabbits. Chemotherapy. 1995;43:903–6.
Hosaka M, Yasue T, Fukuda H, Tomizawa H, Aoyama H, Hirai K. Invitro and invivo antibacterial Activities of Am-1155, a new 6-fluoro-8-methoxy quinolone. Antimicrob Agents chemothe. 1992;36:2108–17.
Kanellakopoulou K, Giamarellos-Bourboulis EJ. Carrier systems for the local delivery of antibiotics in bone infections. Drugs. 2000;59:1223–32.
Mori H, Takahashi T, Sagawa T, Matsunaga H, Matsumura M, Niimura K, et al. Chemical structure and physico-chemical properties of gatifloxacin hydrate. Iyakuhin Kenkyu. 1998;29:885–94.
Cai Q, Shi G, Bei J, Wang S. Enzymatic degradation behavior and mechanism of poly(lactide-co-glycolide) foams by trypsin. Biomaterials. 2003;24:629–38.
Makadia HK, Siegel SJ. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polym-Basel. 2011;3:1377–97.
Perry CM, Balfour JAB, Lamb HM. Gatifloxacin. Drugs. 1999;58:683–96.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Kimishima, K., Matsuno, T., Makiishi, J. et al. Effects of gatifloxaine content in gatifloxacine-loaded PLGA and β-tricalcium phosphate composites on efficacy in treating osteomyelitis. Odontology 104, 105–113 (2016). https://doi.org/10.1007/s10266-014-0187-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-014-0187-9