Abstract
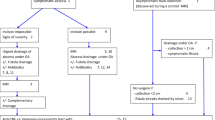
The French National Society of Coloproctology established national recommendations for the treatment of anoperineal lesions associated with Crohn’s disease. Treatment strategies for anal ulcerations and anorectal stenosis are suggested. Recommendations have been graded following international recommendations, and when absent professional agreement was established. For each situation, practical algorithms have been drawn.


Similar content being viewed by others
Abbreviations
- AUC:
-
Anal ulceration of Crohn’s disease
- APL:
-
Ano-perineal lesion
- CD:
-
Crohn’s disease
- PA:
-
Professional agreement
- EA:
-
Expert agreement
- MRI:
-
Nuclear magnetic resonance imaging
- IS:
-
Immunosuppressant
References
Bouchard D, Abramowitz L, Bouguen G, Brochard C, Dabadie A, de Parades V, Eleuet-Kaplan M, Fathallah N, Faucheron J-L, Maggiori L, Panis Y, Pigot F, Roume P, Roumeguere P, Sénéjoux A, Siproudhis L, Staumont G, Suduca J-M, Vinson-Bonnet B, Zeitoun J-D (2017) Anoperineal lesions in Crohn’s disease: French recommendations for clinical practice. Tech Coloproctol 21:683–691
Hughes LE (1992) Clinical classification of perianal Crohn’s disease. Dis Colon Rectum 35:928–932
Schwartz DA, Loftus EV Jr, Tremaine WJ, Panaccione R, Harmsen WS, Zinsmeister AR, Sandborn WJ (2002) The natural history of fistulizing Crohn’s disease in Olmsted County, Minnesota. Gastroenterology 122:875–880
Eglinton TW, Roberts R, Pearson J et al (2012) Clinical and genetic risk factors for perianal Crohn’s disease in a population-based cohort. Am J Gastroenterol 107:589–596
Siproudhis L, Mortaji A, Mary JY, Juguet F, Bretagne JF, Gosselin M (1997) Anal lesions: any significant prognosis in Crohn’s disease ? Eur J Gastroenterol Hepatol 9:239–243
Horaist C, de Parades V, Abramowitz L et al (2017) Elaboration and validation of Crohn’s disease anoperineal lesions consensual definitions. World J Gastroenterol 23:5371–5378
Travis S, Van Assche G, Dignass A, Cabré E, Gassull MA (2010) On the second ECCO Consensus on Crohn’s disease. J Crohns Colitis 4:1–6
Vernier-Massouille G, Balde M, Salleron J, Turck D, Dupas JL, Mouterde O, Merle V, Salomez JL, Branche J, Marti R, Lerebours E, Cortot A, Gower-Rousseau C, Colombel JF (2008) Natural history of pediatric Crohn’s disease: a population-based cohort study. Gastroenterology 135:1106–1113
Fleshner PR, Schoetz DJ Jr, Roberts PL, Murray JJ, Coller JA, Veidenheimer MC (1995) Anal fissure in Crohn’s disease: a plea for aggressive management. Dis Colon Rectum 38:1137–1143
D’Ugo S, Franceschilli L, Cadeddu F, Leccesi L, Blanco Gdel V, Calabrese E, Milito G, Di Lorenzo N, Gaspari AL, Sileri P (2013) Medical and surgical treatment of haemorrhoids and anal fissure in Crohn’s disease: a critical appraisal. BMC Gastroenterol 13:11 47.
Wolkomir AF, Luchtefeld MA (1993) Surgery for symptomatic hemorrhoids and anal fissures in Crohn’s disease. Dis Colon Rectum 36:545–547
Ouraghi A, Nieuviarts S, Mougenel JL et al (2001) Infliximab therapy for Crohn’s disease anoperineal lesions. Gastroenterol Clin Biol 25:949–956
Bouguen G, Trouilloud I, Siproudhis L et al (2009) Long-term outcome of non-fistulizing (ulcers, stricture) perianal Crohn’s disease in patients treated with infliximab. Aliment Pharmacol Ther 30:749–756
Colombel JF, Sandborn WJ, Reinisch W et al (2010) SONIC Study Group. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med 362:1383–1395
Bouguen G, Siproudhis L, Gizard E et al (2013) Long-term outcome of perianal fistulizing Crohn’s disease treated with infliximab. Clin Gastroenterol Hepatol 11:975–81.e1-4
Cosnes J, Bourrier A, Laharie D et al (2013) Groupe d’Etude Thérapeutique des Affections Inflammatoires du Tube Digestif (GETAID). Early administration of azathioprine vs conventional management of Crohn’s Disease: a randomized controlled trial. Gastroenterology 145:758–765
Palder SB, Shandling B, Bilik R, Griffiths AM, Sherman P (1991) Perianal complications of pediatric Crohn’s disease. J Pediatr Surg 26:513–515
Ruemmele FM, Veres G, Kolho KL, European Crohn’s and Colitis Organisation, European Society of Pediatric Gastroenterology, Hepatology and Nutrition et al (2014) Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohns Colitis 8:1179–1207
Yamamoto T, Allan RN, Keighley MR (2000) Effect of fecal diversion alone on perianal Crohn’s disease. World J Surg 24:1258–1262
Regimbeau JM, Panis Y, Pocard M et al (2001) Long-term results of ileal pouch-anal anastomosis for colorectal Crohn’s disease. Dis Colon Rectum 44:769–778
Gu J, Valente MA, Remzi FH, Stocchi L (2015) Factors affecting the fate of faecal diversion in patients with perianal Crohn’s disease. Colorectal Dis 17:66–72
Bafford AC, Latushko A, Hansraj N, Jambaulikar G, Ghazi LJ (2017) The use of temporary fecal diversion in colonic and perianal crohn’s disease does not improve outcomes. Dig Dis Sci 62:2079–2086
Hong MK, Craig Lynch A et al (2011) Faecal diversion in the management of perianal Crohn’s disease. Colorectal Dis 13:171–176
Singh S, Ding NS, Mathis KL, Dulai PS, Farrell AM, Pemberton JH, Hart AL, Sandborn WJ, Loftus EV Jr (2015) Systematic review with meta-analysis: faecal diversion for management of perianal Crohn’s disease. Aliment Pharmacol Ther 42:783–792
Li W, Stocchi L, Elagili F, Kiran RP, Strong SA (2017) Healing of the perineal wound after proctectomy in Crohn’s disease patients: only preoperative perineal sepsis predicts poor outcome. Tech Coloproctol 21:715–720
Adam S (2000 May) Perineal wound morbidity following proctectomy for inflammatory bowel disease (IBD). Colorectal Dis 2(3):165–169
Irvine EJ (1995) Usual therapy improves perianal Crohn’s disease as measured by a new disease activity index. McMaster IBD Study Group. J Clin Gastroenterol 20:27–321
Panes J, Bouhnik Y, Reisnish W et al, Imaging techniques for assessment of inflammatory bowel diseases: joint ECCO and ESGAR evidence based consensus guidelines. J Crohns Colitis 7:556–585
Linares L, Moreira LF, Andrews H, Allan RN, Alexander-Williams J, Keighley MR (1988) Natural history and treatment of anorectal strictures complicating Crohn’s disease. Br J Surg 75(7):653–655
Funding
This work was supported by the French National Society of Coloproctology (SNFCP) and the Groupe d’Etudes Thérapeutique des Affections Inflammatoires du Tube Digestif (GETAID).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Bouchard D: Abbvie, Takeda (consultant and lecture fees), Pigot F : Abbvie (lecture fees), Abramowitz L : Abbvie, Takeda (research fees), Faucheron JL : AMI, Medtronic (consultant, research fees), Laharie D : Abbvie, Janssen, MSD, Takeda (board, lectures fees), Siproudhis L : Abbvie, Ferring, MSD, Takeda (teaching sessions, consultant, research fees). The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bouchard, D., Brochard, C., Vinson-Bonnet, B. et al. How to manage anal ulcerations and anorectal stenosis in Crohn’s disease: algorithm-based decision making. Tech Coloproctol 23, 353–360 (2019). https://doi.org/10.1007/s10151-019-01971-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-01971-6