Abstract
Background
Current guidelines recommend indefinite imatinib treatment for advanced gastrointestinal stromal tumor (GIST) patients. Imatinib-refractory progression-free survival (PFS) and overall survival were previously reported not to differ between GIST patients who interrupted imatinib and those who did not.
Methods
Clinical outcomes of 77 consecutive patients with recurrent or metastatic GIST who interrupted imatinib treatment after maintaining years of imatinib treatment in the absence of gross tumor lesions were retrospectively analyzed. Associations between clinical factors and progression-free survival (PFS) following imatinib interruption were analyzed.
Results
The median time from the absence of gross tumor lesions to imatinib interruption was 61.5 months. Since imatinib interruption, the median PFS was 19.6 months, and 4 patients (26.3%) remained progression-free for longer than 5 years. Among the patients who had progressive disease following the interruption, imatinib re-introduction led to an 88.6% objective response rate and a 100% disease control rate. Complete removal of the initial gross tumor lesion(s) and complete removal of the residual gross tumor lesion(s) by local treatment (vs. no local treatment or residual lesions after local treatment) were independently associated with favorable PFS.
Conclusion
Interruption of imatinib following prolonged maintenance in the absence of gross tumor lesions led to disease progression in the majority of cases. However, re-introduction of imatinib resulted in effective tumor control. Unmaintained remission seems to be possible in some patients with metastatic or recurrent GIST after a prolonged remission with imatinib if there is complete removal of any gross tumor lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors arising in the gastrointestinal tract. Based on the results of the multicenter phase 2 B2222 [1, 2] and the phase 3 SWOG [3] and EORTC studies [4], imatinib is the robust standard first-line agent for patients with metastatic GIST. Thereafter, as multimodal approaches such as surgical resection and appropriate management of adverse events were increasingly applied, treatment outcomes with imatinib were further improved in clinical practice. In a previous report from a large volume center, median PFS and OS with palliative 1st line imatinib were 5.4 and 8.8 years, respectively [5].
International guidelines state that imatinib treatment should be continued [6,7,8] based on the results of the BFR14 study showing that interruption of imatinib led to relatively rapid tumor progression [9,10,11]. However, while imatinib treatment is generally tolerable, a majority of patients experience adverse events [1,2,3,4], which poses a challenge for the chronic administration of imatinib, especially for those with a prolonged response or disease control. In real-world practice, GIST patients who prefer to temporarily interrupt imatinib treatment are often encountered, because of recurrent adverse events, financial issues (especially before the reimbursement of imatinib), medical co-morbidities, or the desire to have a drug holiday [12]. In the mid-2000s, it was shown that imatinib interruption in patients with chronic myeloid leukemia (CML) following a complete molecular remission after certain periods of imatinib maintenance led to unmaintained remission in half of the patients, and most patients with a relapse re-achieved a molecular response following imatinib re-introduction [13]. Given the potent efficacy of imatinib for GIST, the clinical feasibility and unmaintained remission in a proportion of patients from the CML study raised the possibility of interrupting imatinib in selected GIST patients. Moreover, in the BRF14 study [9], along with our retrospective analysis [12], re-introduction of imatinib following disease progression after imatinib interruption achieved tumor control in most cases, and imatinib-refractory PFS and OS were not different between those who interrupted or continued imatinib treatment. These results indicate that imatinib interruption, and re-introduction when disease progresses, may not necessarily have a detrimental impact on the overall treatment course with imatinib.
In the BFR14 study, a proportion of patients interrupted imatinib in the presence of residual gross tumor lesions (i.e., those with a partial response [PR] and stable disease [SD]) [9,10,11]. However, residual gross tumor lesions after imatinib treatment usually contain viable tumor cells on pathological evaluation [14] that could always serve as a source for progressive disease (PD), and surgical resection of residual tumor lesions following imatinib was reportedly associated with a favorable PFS [15]. In this regard, imatinib interruption can be preferentially considered in a clinical situation that recapitulates a high probability of complete eradication of tumor cells, such as a prolonged absence of gross residual lesions with imatinib treatment.
In our previous retrospective analysis of the clinical outcomes of GIST patients who interrupted imatinib or not, patients who interrupted imatinib had worse PFS but similar imatinib-refractory PFS and OS. In that study, the median imatinib treatment duration before interruption was 11.9 months, and imatinib was interrupted despite the presence of gross residual lesions in most cases. Therefore, the prognostic value of interrupting imatinib following long-term administration of imatinib in the absence of gross tumor lesions remained unanswered. Subsequently, a series of patients with recurrent/metastatic GIST who maintained imatinib treatment for a certain period of time (in principle 5 years) in the absence of gross tumor lesions interrupted imatinib treatment after a discussion about the potential outcomes. In this study, we aimed to investigate the clinical outcomes of these patients and provide evidence for selecting candidates who may be considered to interrupt imatinib treatment. In particular, we focused on delineating factors associated with the occurrence of PD following interruption of imatinib, and the clinical outcomes of re-introduction of imatinib after the occurrence of PD during imatinib interruption.
Patients and methods
Study patients
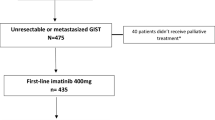
We identified 89 consecutive patients with recurrent/metastatic GIST treated at Asan Medical Center (Seoul, Korea) who initiated palliative 1st line imatinib treatment, achieved a radiological absence of gross tumor lesions with imatinib as assessed by dynamic computed tomography (CT) with or without local treatment, maintained imatinib continuously for, in principle, 5 years in the absence of gross tumor lesions, and interrupted imatinib after a thorough discussion about their disease status between July 2009 and September 2020.
To ensure the absence of gross tumor lesion(s) at the time of imatinib interruption, additional radiological review was performed for all patients by an experienced abdominal radiologist (HJK, a board-certified abdominal radiologist with more than 10 years of experience in abdominal imaging). As a result, 5 patients with gross tumor lesion(s) (≥ 5 mm, which is the CT slice thickness of our institution) identified on the additional radiological review were excluded. In addition, 7 patients with local recurrence at the previous surgical resection site without invasion to any adjacent structure were excluded. Finally, a total of 77 patients were included as the study participants (Supplementary Fig. 1). The protocol of this study was approved by the Institutional Review Board of Asan Medical Center, and the study was conducted according to the principles of the Helsinki declaration. The requirement for informed consent was waived by the Institutional Review Board.
Treatment and evaluation
Patients were initially treated with imatinib at 400 mg once daily. The imatinib dose was carefully modified based on adverse events combined with the imatinib plasma concentration to maintain sufficient imatinib treatment. During imatinib treatment, dynamic abdominopelvic CT scans, with or without chest CT scans, were performed 1 month after the start of imatinib and every 3 months thereafter. The response was assessed according to mRECIST v1.1, which was modified from RECIST v1.1 specifically for GIST [16]. An 18‐fluorodeoxyglucose‐positron emission tomography scan was not routinely performed but was indicated for lesions not definitively evaluable for response by CT scan alone and required further characterization to determine their viability.
According to the timing of local treatment and the completeness of removal of the gross primary and/or metastatic tumor lesions by local treatment, the patients were classified into 3 groups: group 1, complete removal of initial gross lesions before imatinib treatment; group 2, complete removal of residual gross lesions during imatinib treatment; and group 3, no surgery/local treatment or incomplete local treatments.
The tumor genotype was determined by Sanger sequencing as previously described [17]. In summary, genomic DNA was extracted from three tumor sections using a DEXPAT kit (TaKaRa, Kyoto, Japan) and analyzed for mutations in exons 9, 11, 13 and 17 of KIT and exons 12 and 18 of PDGFRA using polymerase chain reaction and Sanger sequencing. For determination of the primary mutation, most patients (n = 74, 93.7%) utilized tumor tissue samples at the time of diagnosis of GIST, while 3 (3.8%) used surgical specimens of resected residual lesions and genomic analysis was not performed for 2 (2.5%) patients.
Interruption and re-introduction of imatinib
In the absence of gross tumor lesions as assessed by CT scans after imatinib treatment for years, imatinib was interrupted after a thorough discussion of the potential outcomes between the attending physicians and patients. After imatinib interruption, the patients underwent cautious surveillance for disease status with radiological evaluation by CT scans performed every 3 months for the first 2 years and every 6 months thereafter.
Upon confirmation of PD during imatinib interruption, imatinib was re-introduced at the previously administered dose. The objective response to the re-introduction of imatinib was analyzed. If the disease progressed following the re-introduction of imatinib, the patients were treated with escalated doses of imatinib or sunitinib as a subsequent treatment.
Mitotic index following imatinib treatment
Among patients who had complete removal of residual tumor during imatinib treatment (group 2), 33 patients received surgical resection for the tumor lesions with or without local treatment for liver metastasis such as radiofrequency ablation or percutaneous ethanol injection, and 9 received local treatment without surgical resection. Among those who received surgery, 30 patients had information on the mitotic count following imatinib treatment, and the mitotic index per 50 high power fields (HPFs) was examined by an experienced gastrointestinal pathologist (YSP, a board-certified gastrointestinal pathologist with more than 10 years of experience in gastrointestinal pathology). Analysis of the mitotic index was not possible in 3 patients whose archived tumor tissue was unavailable.
Statistical analysis
Survival outcomes were estimated based on the Kaplan–Meier method. PFS was defined as the interval from interruption of imatinib to PD or death. Imatinib-refractory PFS was estimated based on the interval from the initiation of 1st line imatinib to the date of imatinib-refractory PD, which refers to disease progression due to the development of resistance to imatinib, or death. Imatinib-refractory PFS since re-introduction of imatinib was estimated based on the interval from the re-introduction of imatinib following PD after interruption to the date of imatinib-refractory PD or death.
PFS was analyzed regarding factors including the primary tumor site (gastric vs. non-gastric), clinical setting (initially metastatic disease vs. recurrent disease), metastatic site, genotype and local treatments. A Cox proportional hazard model was used to analyze the associations between the examined factors and PFS. A P value of < 0.05 was considered statistically significant. Statistical analyses were performed using R software version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Clinical characteristics
The baseline patient characteristics are summarized in Table 1. The median age at the time of initiation of palliative 1st line imatinib treatment was 50 years, and that at the time of imatinib interruption was 57 years, respectively. About two-thirds of patients (n = 52, 67.5%) had liver metastasis, 29 patients (37.7%) had peritoneal metastasis, and 4 had both liver and peritoneal metastases. The median time from the initiation of palliative 1st line imatinib treatment to interruption of imatinib was 72.1 months (range 50.6–155.9 months). The median time from the absence of gross tumor lesions to imatinib interruption was 61.5 months (range 41.4–122.7 months).
There were 19 patients (24.7%) who had complete removal of their initial gross tumor lesions by surgical resection and/or local ablative treatment at the time of initial diagnosis of recurrent/metastatic disease before imatinib treatment (group 1), while 42 (54.5%) had complete removal of their residual gross tumor lesions by local treatments during imatinib treatment (group 2). About 20% of patients (n = 16) achieved the radiological absence of gross tumor lesions by imatinib treatment with or without incomplete local treatment (group 3). Among the samples resected for residual lesions that were tested for genoty** (n = 3), there was no patient who had a KIT secondary resistance mutation.
Overall survival outcomes
Imatinib-resistant PFS estimated from the initiation of palliative 1st line imatinib treatment during a median follow-up of 121.5 months is shown in Fig. 1A. During a median follow-up of 30.4 months, PD was noted in 47 patients (61.0%), resulting in a median PFS of 19.6 months. Among the patients who did not show disease progression after imatinib interruption, 4 patients were followed for 5 years and remained progression-free with a 5-year PFS rate of 26.3% (Fig. 1B).
Clinical outcomes after re-introduction of imatinib
All 47 patients whose disease progressed during imatinib interruption resumed imatinib treatment. The median imatinib-refractory PFS since re-introduction of imatinib was 112.4 months with a 5-year PFS rate of 77.4% (Fig. 1C).
Excluding the 3 patients who received surgical resection for their progressing lesions, 44 patients were available for analysis of their response to imatinib re-introduction. Nine (20.5%), 30 (68.2%) and 5 (11.4%) patients had a complete response (CR), PR and SD, respectively, with an ORR of 88.6% and a disease control rate of 100%. Among those who resumed imatinib, there was no case that had PD as their best response.
Factors associated with progression-free survival since imatinib interruption
Next, PFS since imatinib interruption was examined regarding various clinical factors. PFS was not different according to the primary tumor site (gastric vs. non-gastric), clinical setting (initially metastatic disease vs. recurrent disease) or the genotype. Patients with liver metastasis showed a trend toward a more favorable PFS than those without liver metastasis (P = 0.055) (Supplementary Fig. 2A), whereas those with peritoneal metastasis tended to be associated with poor PFS (P = 0.081) (Supplementary Fig. 2B).
When PFS was analyzed for groups subjected to local treatments, those who had complete removal of their initial gross tumor lesion(s) before imatinib treatment (group 1) and complete removal of their residual gross tumor lesion(s) during imatinib treatment (group 2) by local treatments exhibited more favorable PFS than those who achieved the radiological absence of gross tumor lesions by imatinib treatment with or without incomplete local treatment (group 3) (P = 0.003) (Fig. 2).
In multivariate Cox proportional analysis, complete removal of initial gross tumor lesion(s) (hazard ratio [HR] 0.32, 95% CI 0.12–0.81, P = 0.016) and complete removal of residual gross tumor lesion(s) (HR 0.45, 95% CI 0.21–0.94, P = 0.033) by local treatments (vs. no local treatment or residual lesions after local treatment) were independently associated with favorable PFS since interruption of imatinib (Table 2). In addition, the absence of peritoneal metastasis tended to be associated with a favorable PFS with marginal statistical significance (HR 0.52, 95% CI 0.26–1.05, P = 0.070).
Mitotic Index Following Imatinib Treatment and Progression-free Survival
Among patients who had information on their mitotic index (n = 30) from the surgery following imatinib treatment, those who had a low mitotic count (≤ 5/50 HPFs) had more favorable PFS since interruption of imatinib compared to those with a high mitotic count (> 5/50 HPFs) (P = 0.026) (Supplementary Fig. 3A), especially those with a mitotic count of 0/50 HPFs (Supplementary Fig. 3B).
When patients with different mitotic indices were analyzed together with groups 1 and 3, those with a mitotic index of ≤ 5/50 HPFs showed the most favorable PFS, whereas those with a mitotic index > 5/50 HPFs showed poor PFS, which was comparable to group 3 (Supplementary Fig. 4).
Profiles of patients remaining progression-free following imatinib interruption
Table 3 summarizes the profiles of the 4 patients who remain progression-free after 5 years of imatinib interruption. These patients had liver metastasis but not peritoneal metastasis. All of these patients achieved complete removal of their initial gross tumor lesion(s) or complete removal of their residual gross tumor lesion(s) by local treatments. For the 2 patients with surgical resection following imatinib treatment, their mitotic index was 0/50 HPFs and < 2/50 HPFs, respectively.
Discussion
In this study, we investigated the clinical outcomes of patients with recurrent/metastatic GIST who interrupted imatinib following years of its use for maintenance in the absence of gross tumor lesions. The median PFS with imatinib interruption was 19.6 months, and a proportion of patients remained progression-free, with a 5-year PFS rate of 26.3%, which indicates that unmaintained remission, which is defined as a complete remission (no radiological residual lesion) maintained without imatinib, is possible in at least some patients with metastatic disease. Following PD after imatinib interruption, re-introduction of imatinib achieved a response in most cases with a median imatinib-refractory PFS of 112.4 months, which suggests that interruption of imatinib does not promote the development of resistance to imatinib. The complete removal of gross tumor lesion(s) by local treatment either at the time of diagnosis of metastatic disease or during imatinib treatment was an independent factor associated with a favorable PFS. To our knowledge, this is the first study to report clinical outcomes of imatinib interruption following a long-term absence of gross tumor lesions, and to delineate factors associated with disease progression in this clinical setting. These findings may provide practical insights for recurrent/metastatic GIST patients who may be considering an imatinib interruption.
One of the most important aspects of our study is that the complete removal of gross tumor lesions by local treatment was associated with favorable PFS following imatinib interruption. This suggests that even if the gross tumor lesions become invisible by imatinib treatment only, the lesions are likely to still have microscopic viable tumor cells, whereas local treatment could achieve complete eradication of the viable tumor cells. In the BFR14 study that randomized patients after 1 year of imatinib, patients who interrupted imatinib in a CR achieved only by imatinib treatment had a short PFS, which was comparable to that of those with gross residual disease [9]. Also, in the pooled analysis of the BFR study, which included those who interrupted imatinib after 1, 3 and 5 years, although the PFS tended to be longer in patients achieving a CR, followed by PR and SD, those with a CR still had a short PFS (median 10.4 months) [18]. Therefore, given that about two-thirds of patients achieved complete removal of gross tumor lesions by local treatment in the current study, complete local treatment appears to be one of the main factors explaining the different PFS following imatinib interruption between the BFR14 (median PFS 6.1–10.8 months) [9,10,11] study and our (median PFS 19.6 months) study. In particular, it is noteworthy that all 4 patients who achieved an unmaintained remission over 5 years of imatinib interruption had their gross tumor lesions removed by local treatments. A recently reported phase 2 study of 12 metastatic GIST patients who were treated with imatinib for ≥ 5 years and had their metastatic lesions grossly removed by local treatment found that 40% remained progression-free following imatinib interruption during a median follow-up of 42 months in this setting [19]. These results are in line with our findings. Therefore, imatinib interruption might preferentially be considered in those achieving complete removal of gross tumor lesions by local treatment than in those achieving a CR by imatinib treatment only. Nevertheless, our results need to be cautiously interpreted in consideration of the possibility that patients who received surgery may be associated with favorable factors such as an initially low tumor burden, good performance status, or less severe complications with imatinib.
Unlike peritoneal metastases, which could easily be missed by imaging studies or during surgical exploration, metastatic lesions in the liver are generally quite visible against the normal liver parenchyma with contrast enhancement and they are more likely to be removed by local treatments, including surgery or local ablation. This concept is supported by our findings showing that liver metastasis was associated with a trend toward favorable PFS, whereas the presence of peritoneal metastasis showed a trend toward poor PFS.
Consistent with previous reports [15, 20], local treatment for residual gross tumor lesions following imatinib treatments was associated with favorable PFS. Importantly, those who had a low mitotic index (≤ 5/50 HPFs) had a prominently favorable PFS. While mitosis has been classically considered an important factor representing the aggressive biological feature of GIST [21, 22], there has been limited information as to its value following imatinib treatment. A low mitotic index can be observed in tumors with a low baseline mitotic index, suggestive of less aggressive tumor biology, and also in tumors that achieved a pronounced reduction of mitosis with imatinib, which is indicative of a favorable responsiveness to imatinib. Therefore, interruption of imatinib may be preferentially considered in patients with tumors that have a low mitotic index following imatinib treatment when metastatic lesions have been completely removed by local treatments and imatinib was maintained for a sufficient duration of time.
Another aspect to note in our study is that imatinib was interrupted following its long-term maintenance with ‘the absence of gross GIST lesion(s)’ achieved either with or without local treatments (median 61.5 months). Prolonged administration of imatinib per se may allow for the selection of patients with favorable prognostic factors and/or a favorable clinical response to imatinib without develo** therapeutic resistance. The results of the BFR 14 study showing that a longer duration of imatinib administration prior to interruption was associated with longer PFS after imatinib interruption [9,10,11, 18] is also in line with this concept. Based on our results, imatinib interruption may be considered among those who maintained imatinib for a long-term period after achieving the disappearance of their gross GIST lesion(s). Nevertheless, it should also be noted that the time elapsed from the absence of a gross GIST lesion to imatinib interruption was not a factor associated with PFS, which indicates that the clinical relevance of a prolonged duration of imatinib may be somewhat limited to a certain period of imatinib treatment.
Since this study was not a prospective randomized study, interpretation of our study may be limited. A randomized study is currently ongoing to address the feasibility of interrupting imatinib treatment following 10 years of imatinib treatment (GIST-TEN, NCT05009927), which is expected to provide evidence to guide imatinib interruption. Nevertheless, it should be considered that inclusion in the GIST-TEN study did not require the complete removal of gross tumor lesions by local treatment, which was shown to be linked to favorable PFS in our study. Moreover, performing prospective studies dealing with the issue of imatinib interruption following years of imatinib treatment would be practically difficult. A recently reported phase 2 study of imatinib interruption was prematurely closed due to slow patient accrual (12 recruited out of 31 planned) [19], and a similar study of patients who received imatinib for more than 5 years and who had complete removal of gross metastatic lesions by surgical resection or radiofrequency ablation was also suspended due to slow accrual (NCT02924714). Therefore, our study, based on a decent number of patients and with a relatively long follow-up duration, may provide important and detailed practical insights for considering imatinib interruption in GIST.
Regarding the definition of having no gross lesions by radiological assessment, we employed a ≥ 5 mm criterion to essentially include patients having no radiological residual gross tumor lesion(s). However, while dynamic CT is the mainstay of radiological evaluation for GIST, our results should be interpreted in consideration of the fact that the current CT platform is still technically limited for characterizing small nodules. To minimize the impact of this issue, a full radiological review of all of the serial CT scans to track indeterminate lesions was performed by an abdominal radiology specialist to assess whether such lesions were small gross residual tumors or benign lesions. As a result, 5 patients who met the criterion of residual tumor lesions ≥ 5 mm in size were excluded from the current study based on CT scans taken at the time of interruption or at subsequent follow-ups.
Recently, circulating tumor DNA (ctDNA) is increasingly being used to guide treatment decisions by providing information on specific mutations or minimal residual disease (MRD). In a recent study of stage II colon cancer, ctDNA-guided treatment decisions were shown to reduce the use of adjuvant chemotherapy without compromising recurrence-free survival relative to the standard treatment decision based on clinicopathological features [23]. Although recent GIST studies have evaluated the utility of ctDNA analysis to detect primary and secondary mutations that correlate with clinical outcomes in response to various agents [24,25,26], there has been no study, to our knowledge, reporting on the clinical utility of ctDNA-based MRD evaluations to guide treatment decisions in GIST patients. This may be because the limited array of mutations other than KIT and PDGFRA [27] may pose a challenge for evaluating MRD in GIST. As for CML, in which blood is a major dwelling site for tumor cells and MRD is systematically defined, imatinib discontinuation was shown to be safe when undetectable MRD was achieved for at least 2 years [28, 29]. In GIST, where the accurate assessment of viable tumor cells is currently challenging with both radiological and ctDNA evaluation, further efforts are needed to develop a platform that can sensitively evaluate MRD with a specific focus on KIT and PDGFRA mutations and to employ MRD to guide treatment decisions, such as interrupting imatinib.
In conclusion, interruption of imatinib following prolonged maintenance in the absence of gross tumor lesions led to disease progression in a majority of cases. However, re-introduction of imatinib resulted in effective tumor control. Unmaintained remission seems to be possible for some patients with metastatic or recurrent GIST after a prolonged remission with imatinib if there is complete removal of any gross tumor lesions. Interruption of imatinib may be considered with close surveillance, especially for those with complete removal of gross tumor lesions by local treatment.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author (YKK) on reasonable request.
Abbreviations
- GISTs:
-
Gastrointestinal stromal tumors
- ORR:
-
Objective response rate
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- CML:
-
Chronic myeloid leukemia
- PR:
-
Partial response
- SD:
-
Stable disease
- PD:
-
Progressive disease
- CT:
-
Computed tomography
- HPFs:
-
High power fields
- CR:
-
Complete response
- ctDNA:
-
Circulating tumor DNA
- MRD:
-
Minimal residual disease
References
Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347:472–80. https://doi.org/10.1056/NEJMoa020461.
Blanke CD, Demetri GD, von Mehren M, et al. Long-term results from a randomized phase II trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol. 2008;26:620–5. https://doi.org/10.1200/jco.2007.13.4403.
Blanke CD, Rankin C, Demetri GD, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008;26:626–32. https://doi.org/10.1200/jco.2007.13.4452.
Casali PG, Zalcberg J, Le Cesne A, et al. Ten-year progression-free and overall survival in patients with unresectable or metastatic GI stromal tumors: long-term analysis of the european organisation for research and treatment of cancer, Italian sarcoma group, and australasian gastrointestinal trials group intergroup phase III randomized trial on imatinib at two dose levels. J Clin Oncol. 2017;35:1713–20. https://doi.org/10.1200/jco.2016.71.0228.
Kim JH, Ryu MH, Yoo C, et al. Long-term survival outcome with tyrosine kinase inhibitors and surgical intervention in patients with metastatic or recurrent gastrointestinal stromal tumors: A 14-year, single-center experience. Cancer Med. 2019;8:1034–43. https://doi.org/10.1002/cam4.1994.
Casali PG, Blay JY, Abecassis N, et al. Gastrointestinal stromal tumours: ESMO-EURACAN-GENTURIS clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2022;33:20–33. https://doi.org/10.1016/j.annonc.2021.09.005.
Koo DH, Ryu MH, Kim KM, et al. Asian consensus guidelines for the diagnosis and management of gastrointestinal stromal tumor. Cancer Res Treat. 2016;48:1155–66. https://doi.org/10.4143/crt.2016.187.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Blay JY, Le Cesne A, Ray-Coquard I, et al. Prospective multicentric randomized phase III study of imatinib in patients with advanced gastrointestinal stromal tumors comparing interruption versus continuation of treatment beyond 1 year: the French Sarcoma Group. J Clin Oncol. 2007;25:1107–13. https://doi.org/10.1200/jco.2006.09.0183.
Le Cesne A, Ray-Coquard I, Bui BN, et al. Discontinuation of imatinib in patients with advanced gastrointestinal stromal tumours after 3 years of treatment: an open-label multicentre randomised phase 3 trial. Lancet Oncol. 2010;11:942–9. https://doi.org/10.1016/s1470-2045(10)70222-9.
Ray-Coquard I, Bin Bui N, Adenis A, et al. Risk of relapse with imatinib (IM) discontinuation at 5 years in advanced GIST patients: results of the prospective BFR14 randomized phase III study comparing interruption versus continuation of IM at 5 years of treatment: a French Sarcoma Group Study. J Clin Oncol. 2010;28:10032.
Lee JL, Ryu MH, Chang HM, et al. Clinical outcome in gastrointestinal stromal tumor patients who interrupted imatinib after achieving stable disease or better response. Jpn J Clin Oncol. 2006;36:704–11. https://doi.org/10.1093/jjco/hyl088.
Rousselot P, Huguet F, Rea D, et al. Imatinib mesylate discontinuation in patients with chronic myelogenous leukemia in complete molecular remission for more than 2 years. Blood. 2007;109:58–60. https://doi.org/10.1182/blood-2006-03-011239.
Kurokawa Y, Yang HK, Cho H, et al. Phase II study of neoadjuvant imatinib in large gastrointestinal stromal tumours of the stomach. Br J Cancer. 2017;117:25–32. https://doi.org/10.1038/bjc.2017.144.
Park SJ, Ryu MH, Ryoo BY, et al. The role of surgical resection following imatinib treatment in patients with recurrent or metastatic gastrointestinal stromal tumors: results of propensity score analyses. Ann Surg Oncol. 2014;21:4211–7. https://doi.org/10.1245/s10434-014-3866-4.
Demetri GD, Reichardt P, Kang YK, et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295–302. https://doi.org/10.1016/s0140-6736(12)61857-1.
Bang YH, Ryu MH, Kim HD, et al. Clinical outcomes and prognostic factors for patients with high-risk gastrointestinal stromal tumors treated with 3-year adjuvant imatinib. Int J Cancer. 2022;151:1770–7. https://doi.org/10.1002/ijc.34157.
Patrikidou A, Chabaud S, Ray-Coquard I, et al. Influence of imatinib interruption and rechallenge on the residual disease in patients with advanced GIST: results of the BFR14 prospective French Sarcoma Group randomised, phase III trial. Ann Oncol. 2013;24:1087–93. https://doi.org/10.1093/annonc/mds587.
Hompland I, Boye K, Papakonstantinou A, et al. Discontinuation of imatinib in patients with oligo-metastatic gastrointestinal stromal tumor who are in complete radiological remission: a prospective multicenter phase II study. J Clin Oncol. 2022; 40(16_suppl). https://doi.org/10.1200/JCO.2022.40.16_suppl.11535.
Bauer S, Rutkowski P, Hohenberger P, et al. Long-term follow-up of patients with GIST undergoing metastasectomy in the era of imatinib – analysis of prognostic factors (EORTC-STBSG collaborative study). Eur J Surg Oncol. 2014;40:412–9. https://doi.org/10.1016/j.ejso.2013.12.020.
Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Seminars in diagnostic pathology. Amsterdam: Elsevier; 2006. p. 70–83.
Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008;39:1411–9.
Tie J, Cohen JD, Lahouel K, et al. Circulating tumor DNA analysis guiding adjuvant therapy in stage II colon cancer. N Engl J Med. 2022;386:2261–72. https://doi.org/10.1056/NEJMoa2200075.
Bauer S, Heinrich MC, George S, et al. Clinical Activity of Ripretinib in Patients with Advanced Gastrointestinal Stromal Tumor Harboring Heterogeneous KIT/PDGFRA Mutations in the Phase III INVICTUS Study. Clin Cancer Res. 2021;27:6333–42. https://doi.org/10.1158/1078-0432.Ccr-21-1864.
Bialick S, Rose BE, Espejo-Freire AP, et al. KIT resistance mutations identified by circulating tumor DNA and treatment outcomes in advanced gastrointestinal stromal tumor. J Clin Oncol. 2022;40(16_suppl):11514. https://doi.org/10.1200/JCO.2022.40.16_suppl.11514.
Serrano C, Bauer S, Gómez-Peregrina D, et al. Circulating tumor DNA (ctDNA) analyses of the phase III VOYAGER trial: KIT mutational landscape and outcomes in patients with advanced gastrointestinal stromal tumor (GIST). J Clin Oncol. 2022;40(16_suppl):101: https://doi.org/10.1200/JCO.2022.40.16_suppl.101.
Vanden Bempt I, Vander Borght S, Sciot R, et al. Comprehensive targeted next-generation sequencing approach in the molecular diagnosis of gastrointestinal stromal tumor. Genes Chromosomes Cancer. 2021;60:239–49. https://doi.org/10.1002/gcc.22923.
Mahon FX, Réa D, Guilhot J, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11:1029–35. https://doi.org/10.1016/s1470-2045(10)70233-3.
Etienne G, Guilhot J, Rea D, et al. Long-term follow-up of the French stop imatinib (STIM1) study in patients with chronic myeloid leukemia. J Clin Oncol. 2017;35:298–305. https://doi.org/10.1200/jco.2016.68.2914.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Nothing directly related to this work. Out of this work, YKK has served as a consultant for ALX Oncology, Zymeworks, Amgen, Novartis, Macrogenics, Daehwa, Blueprint, Surface Oncolgy, BMS, Merck (MSD). MHR received honoraria from DAEHWA Pharmaceutical, Bristol Myers Squibb, Lilly, Ono Pharmaceutical, MSD, Taiho Pharmaceutical, Novartis, Daiichi Sankyo and AstraZeneca, and served as a consultant for DAEHWA Pharmaceutical, Bristol Myers Squibb, Lilly and Ono Pharmaceutical.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kang, YK., Kim, HD., Kim, H.J. et al. Interruption of imatinib in advanced gastrointestinal stromal tumor after prolonged imatinib maintenance in the absence of gross tumor lesions. Gastric Cancer 26, 604–613 (2023). https://doi.org/10.1007/s10120-023-01377-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-023-01377-2