Abstract
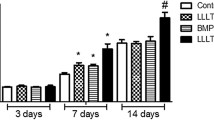
Melatonin has anabolic effects on the bone, even under hypoxia, and laser irradiation has been shown to improve osteoblastic differentiation. The aim of this study was to investigate whether laser irradiation and melatonin would have synergistic effects on osteoblastic differentiation and mineralization under hypoxic conditions. MC3T3-E1 cells were exposed to 1% oxygen tension for the hypoxia condition. The cells were divided into four groups: G1-osteoblast differentiation medium only (as the hypoxic condition), G2-treatment with 50 μM melatonin only, G3-laser irradiation (808 nm, 80 mW, GaAlAs diode) only, and G4-treatment with 50 μM melatonin and laser irradiation (808 nm, 80 mW, GaAlAs diode). Immunoblotting showed that osterix expression was markedly increased in the melatonin-treated and laser-irradiated cells at 48 and 72 h. In addition, alkaline phosphatase activity significantly increased and continued to rise throughout the experiment. Alizarin Red staining showed markedly increased mineralized nodules as compared with only melatonin-treated or laser-irradiated cells at day 7, which significantly increased by day 14. Moreover, when melatonin-treated cells were laser-irradiated, the differentiation and mineralization of cells were found to involve p38 MAPK and PRKD1 signaling mechanisms. However, the enhanced effects of laser irradiation with melatonin were markedly inhibited when the cells were treated with luzindole, a selective melatonin receptor antagonist. Therefore, we concluded that laser irradiation could promote the effect of melatonin on the differentiation and mineralization of MC3T3-E1 cells under hypoxic conditions, and that this process is mediated through melatonin 1/2 receptors and PKRD/p38 signaling pathways.





Similar content being viewed by others
References
Stehle JH, Saade A, Rawashdeh O, Ackermann K, Jilg A, Sebesteny T, Maronde E (2011) A survey of molecular details in the human pineal gland in the light of phylogeny, structure, function and chronobiological diseases. J Pineal Res 51:17–43
Roth JA, Kim BG, Lin WL, Cho MI (1999) Melatonin promotes osteoblast differentiation and bone formation. J Biol Chem 274:22041–22047
Amstrup AK, Sikjaer T, Mosekilde L, Rejnmark L (2013) Melatonin and the skeleton. Osteoporos Int 24:2919–2927
Radio NM, Doctor JS, Witt-Enderby PA (2006) Melatonin enhances alkaline phosphatase activity in differentiating human adult mesenchymal stem cells grown in osteogenic medium via MT2 melatonin receptors and the MEK/ERK (1/2) signaling cascade. J Pineal Res 40:332–342
Ekmekcioglu C (2006) Melatonin receptors in humans: biological role and clinical relevance. Biomed Pharmacother 60:97–108
Reiter RJ (2000) Melatonin: lowering the high price of free radicals. News Physiol Sci 15:246–250
Lopez A, Garcia JA, Escames G, Venegas C, Ortiz F, Lopez LC, Acuna-Castroviejo D (2009) Melatonin protects the mitochondria from oxidative damage reducing oxygen consumption, membrane potential, and superoxide anion production. J Pineal Res 46:188–198
Yilmaz S, Yilmaz E (2006) Effects of melatonin and vitamin E on oxidative-antioxidative status in rats exposed to irradiation. Toxicology 222:1–7
Son JH, Cho YC, Sung IY, Kim IR, Park BS, Kim YD (2014) Melatonin promotes osteoblast differentiation and mineralization of MC3T3-E1 cells under hypoxic conditions through activation of PKD/p38 pathways. J Pineal Res 57:385–392
Rola P, Doroszko A, Derkacz A (2014) The use of low-level energy laser radiation in basic and clinical research. Adv Clin Exp Med 23:835–842
Kushibiki T, Hirasawa T, Okawa S, Ishihara M (2015) Low reactive level laser therapy for mesenchymal stromal cells therapies. Stem Cells Int 2015:974864
Silva Junior AN, Pinheiro AL, Oliveira MG, Weismann R, Ramalho LM, Nicolau RA (2002) Computerized morphometric assessment of the effect of low-level laser therapy on bone repair: an experimental animal study. J Clin Laser Med Surg 20:83–87
Shimizu N, Mayahara K, Kiyosaki T, Yamaguchi A, Ozawa Y, Abiko Y (2007) Low-intensity laser irradiation stimulates bone nodule formation via insulin-like growth factor-I expression in rat calvarial cells. Lasers Surg Med 39:551–559
AlGhamdi KM, Kumar A, Moussa NA (2012) Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci 27:237–249
Karu TI, Pyatibrat LV, Kalendo GS (2004) Photobiological modulation of cell attachment via cytochrome c oxidase. Photochem Photobiol Sci 3:211–216
Saygun I, Nizam N, Ural AU, Serdar MA, Avcu F, Tozum TF (2012) Low-level laser irradiation affects the release of basic fibroblast growth factor (bFGF), insulin-like growth factor-I (IGF-I), and receptor of IGF-I (IGFBP3) from osteoblasts. Photomed Laser Surg 30:149–154
Nissan J, Assif D, Gross MD, Yaffe A, Binderman I (2006) Effect of low intensity laser irradiation on surgically created bony defects in rats. J Oral Rehabil 33:619–924
Cury V, Moretti AI, Assis L, Bossini P, Crusca Jde S, Neto CB, Fangel R, de Souza HP, Hamblin MR, Parizotto NA (2013) Low level laser therapy increases angiogenesis in a model of ischemic skin flap in rats mediated by VEGF, HIF-1alpha and MMP-2. J Photochem Photobiol B 125:164–170
Khadra M, Lyngstadaas SP, Haanaes HR, Mustafa K (2005) Effect of laser therapy on attachment, proliferation and differentiation of human osteoblast-like cells cultured on titanium implant material. Biomaterials 26:3503–3509
Theodoro LH, Sampaio JE, Haypek P, Bachmann L, Zezell DM, Garcia VG (2006) Effect of Er:YAG and diode lasers on the adhesion of blood components and on the morphology of irradiated root surfaces. J Periodontal Res 41:381–390
Taylor CT (2008) Mitochondria and cellular oxygen sensing in the HIF pathway. Biochem J 409:19–26
Zhang LF, Qi J, Zuo G, Jia P, Shen X, Shao J, Kang H, Yang H, Deng L (2014) Osteoblast-secreted factors promote proliferation and osteogenic differentiation of bone marrow stromal cells via VEGF/heme-oxygenase-1 pathway. PLoS One 9, e99946
Semenza GL (2009) Regulation of oxygen homeostasis by hypoxia-inducible factor 1. Physiology (Bethesda) 24:97–106
Bilezikian JP, Raisz LG, Martin TJ (2008) Principles of bone biology. Academic Press/Elsevier, San Diego
Kimira Y, Ogura K, Taniuchi Y, Kataoka A, Inoue N, Sugihara F, Nakatani S, Shimizu J, Wada M, Mano H (2014) Collagen-derived dipeptide prolyl-hydroxyproline promotes differentiation of MC3T3-E1 osteoblastic cells. Biochem Biophys Res Commun 453:498–501
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B (2002) The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 108:17–29
Nishio Y, Dong Y, Paris M, O’Keefe RJ, Schwarz EM, Drissi H (2006) Runx2-mediated regulation of the zinc finger Osterix/Sp7 gene. Gene 372:62–70
Pearson G, Robinson F, Beers Gibson T, Xu BE, Karandikar M, Berman K, Cobb MH (2001) Mitogen-activated protein (MAP) kinase pathways: regulation and physiological functions. Endocr Rev 22:153–183
Cuschieri J, Maier RV (2005) Mitogen-activated protein kinase (MAPK). Crit Care Med 33:S417–419
Lemonnier J, Ghayor C, Guicheux J, Caverzasio J (2004) Protein kinase C-independent activation of protein kinase D is involved in BMP-2-induced activation of stress mitogen-activated protein kinases JNK and p38 and osteoblastic cell differentiation. J Biol Chem 279:259–264
Celil AB, Campbell PG (2005) BMP-2 and insulin-like growth factor-I mediate Osterix (Osx) expression in human mesenchymal stem cells via the MAPK and protein kinase D signaling pathways. J Biol Chem 280:31353–31359
Aleksic V, Aoki A, Iwasaki K, Takasaki AA, Wang CY, Abiko Y, Ishikawa I, Izumi Y (2010) Low-level Er:YAG laser irradiation enhances osteoblast proliferation through activation of MAPK/ERK. Lasers Med Sci 25:559–569
Miyata H, Genma T, Ohshima M, Yamaguchi Y, Hayashi M, Takeichi O, Ogiso B, Otsuka K (2006) Mitogen-activated protein kinase/extracellular signal-regulated protein kinase activation of cultured human dental pulp cells by low-power gallium-aluminium-arsenic laser irradiation. Int Endod J 39:238–244
Komarova SV, Ataullakhanov FI, Globus RK (2000) Bioenergetics and mitochondrial transmembrane potential during differentiation of cultured osteoblasts. Am J Physiol Cell Physiol 279:C1220–1229
Pires Oliveira DA, de Oliveira RF, Zangaro RA, Soares CP (2008) Evaluation of low-level laser therapy of osteoblastic cells. Photomed Laser Surg 26:401–404
Kujawa J, Zavodnik L, Zavodnik I, Buko V, Lapshyna A, Bryszewska M (2004) Effect of low-intensity (3.75-25 J/cm2) near-infrared (810 nm) laser radiation on red blood cell ATPase activities and membrane structure. J Clin Laser Med Surg 22:111–117
Kujawa J, Pasternak K, Zavodnik I, Irzmanski R, Wrobel D, Bryszewska M (2014) The effect of near-infrared MLS laser radiation on cell membrane structure and radical generation. Lasers Med Sci 29:1663–1668
Cipolla-Neto J, Amaral FG, Afeche SC, Tan DX, Reiter RJ (2014) Melatonin, energy metabolism, and obesity: a review. J Pineal Res 56:371–381
Liu J, Clough SJ, Hutchinson AJ, Adamah-Biassi EB, Popovska-Gorevski M, Dubocovich ML (2016) MT1 and MT2 melatonin receptors: a therapeutic perspective. Annu Rev Pharmacol Toxicol 56:361–383
Laakso L, Richardson C, Cramond T (1993) Factors affecting low level laser therapy. Aust J Physiother 39:95–99
Gao X, **ng D (2009) Molecular mechanisms of cell proliferation induced by low power laser irradiation. J Biomed Sci 16:4
Migliario M, Pittarella P, Fanuli M, Rizzi M, Reno F (2014) Laser-induced osteoblast proliferation is mediated by ROS production. Lasers Med Sci 29:1463–1467
Wu S, **ng D, Gao X, Chen WR (2009) High fluence low-power laser irradiation induces mitochondrial permeability transition mediated by reactive oxygen species. J Cell Physiol 218:603–611
Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82:47–95
Acknowledgements
Special thanks to Ji-Eun Kim for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the National Research Foundation of Korea (NRF2015R1D1A3A01016667).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
Rights and permissions
About this article
Cite this article
Son, JH., Park, BS., Kim, IR. et al. A novel combination treatment to stimulate bone healing and regeneration under hypoxic conditions: photobiomodulation and melatonin. Lasers Med Sci 32, 533–541 (2017). https://doi.org/10.1007/s10103-017-2145-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2145-6