Abstract
Intention
Immunosuppressive therapy is the major treatment approach for patients with anti-neutrophil cytoplasmic antibody-associated vasculitis (AAV). Due to impaired cellular immunological function and the use of glucocorticoids and immunosuppressants, AAV patients are predisposed to opportunistic infections, including tuberculosis (TB). This retrospective study aims to analyze the clinical characteristics of patients with AAV and TB and explore suitable glucocorticoid regimens for them. So as to provide a basis for future clinical guidelines and have important value for guiding clinical treatment.
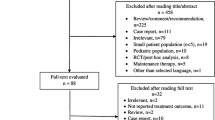
Methods
This study retrospectively reviewed 58 AAV patients (18–80 years old) with TB admitted to Changsha Central Hospital Affiliated with the University of South China from 2016.1 to 2023.4 Patients were divided into standard-dose and reduced-dose glucocorticoid groups before retrospectively analyzing their medical records.
Results
A total of 58 AAV patients with TB were enrolled, with 15 dying throughout the monitoring period. Through analysis data, compared with the standard-dose group, the reduced group had less proteinuria and hematuria. In survival analysis, the reduced-dose glucocorticoid group had lower mortality than the standard-dose group (P = 0.03); however, no significant difference was noted in the use of immunoglobulin (P = 0.39), tuberculosis activity (P = 0.64), and age stratification (P = 0.40). The BVAS score before treatment and 6 months post-treatment suggest that the two regimens cause the same risk of ESKD (P > 0.05).
Conclusion
In conclusion, the reduced glucocorticoid dose group can achieve the same curative effect as the standard dose group and has less damage to the kidney in hematuria and proteinuria. Therefore, the reduced glucocorticoid dose treatment regimen may be more suitable for AAV patients with TB.







Similar content being viewed by others
Data availability
The data sets used and/or analyzed during the present study were availed by the corresponding author upon reasonable request.
Abbreviations
- CHD:
-
Coronary heart disease
- COPD:
-
Chronic Obistructive Pulmonary Disease
- ESKD:
-
End Stage Kidney Disease
- BAVS:
-
Birmingham vasculitis activity score
- TB:
-
Tuberculosis
References
Liao QQ, Ren YF, Zhu KW et al (2022) Long-term prognostic factors in patients with Antineutrophil cytoplasmic antibody-Associated Vasculitis: a 15-Year Multicenter Retrospective Study[J]. Front Immunol 13:913667
Ponte C, Águeda AF, Luqmani RA (2018) Clinical features and structured clinical evaluation of vasculitis[J]. Best Pract Res Clin Rheumatol 32(1):31–51
Sherkat R, Mostafavizadeh K, Zeydabadi L et al (2011) Antineutrophil cytoplasmic antibodies in patients with pulmonary tuberculosis[J]. Iran J Immunol 8(1):52–57
Satoskar AA, Suleiman S, Ayoub I et al (2017) Staphylococcus infection-Associated GN - Spectrum of IgA Staining and Prevalence of ANCA in a single-center Cohort[J]. Clin J Am Soc Nephrol 12(1):39–49
Xun C (2021) Distribution characteristics of ANA and ANCA in patients with Hyperthyroidism[J]. Endocr Metab Immune Disord Drug Targets 21(11):1993–1997
Lopens S, Wunsch E, Milkiewicz M et al (2022) PR3-ANCAs detected by third-generation ELISA predicts severe disease and poor survival in primary sclerosing Cholangitis[J]. Diagnostics (Basel), 12(11)
Patel NJ, Stone JH (2022) Expert Perspective: management of Antineutrophil cytoplasmic antibody-Associated Vasculitis[J]. Arthritis Rheumatol 74(8):1305–1317
Walsh M, Collister D, Zeng L et al (2022) The effects of plasma exchange in patients with ANCA-associated vasculitis: an updated systematic review and meta-analysis[J]. BMJ 376:e064604
Bellos I, Michelakis I, Nikolopoulos D (2021) The role of plasma exchange in antineutrophil cytoplasmic antibody-associated vasculitis: a meta-analysis[J]. Clin Rheumatol 40(4):1447–1456
Winthrop KL, Novosad SA, Baddley JW et al (2015) Opportunistic infections and biologic therapies in immune-mediated inflammatory diseases: consensus recommendations for infection reporting during clinical trials and postmarketing surveillance[J]. Ann Rheum Dis 74(12):2107–2116
Chander Y, Acharya N, Naidu G et al (2022) Prevalence of Antineutrophil Cytoplasmic Antibodies and Antinuclear Antibodies in patients with pulmonary tuberculosis: a Tertiary Care Center Experience from North India[J]. J Assoc Physicians India 70(11):11–12
Ji G, Zeng X, Sandford AJ et al (2016) Rifampicin-induced antineutrophil cytoplasmic antibody-positive vasculitis: a case report and review of the literature[J]. Int J Clin Pharmacol Ther 54(10):804–807
Griffin SOB, Mclaughlin B (2021) A M, ANCA associated glomerulonephritis in tuberculosis: a paradoxical reaction[J]. BMJ Case Rep, 14(6)
Solans-Laqué R, Rodriguez-Carballeira M, Rios-Blanco JJ et al (2020) Comparison of the Birmingham Vasculitis Activity Score and the five-factor score to assess survival in Antineutrophil cytoplasmic antibody-Associated Vasculitis: a study of 550 patients from Spain (REVAS Registry)[J]. Arthritis Care Res (Hoboken) 72(7):1001–1010
Walsh M, Merkel PA, Peh CA et al (2020) Plasma exchange and glucocorticoids in severe ANCA-Associated Vasculitis[J]. N Engl J Med 382(7):622–631
Hellmich B, Sanchez-Alamo B, Schirmer JH et al (2024) EULAR recommendations for the management of ANCA-associated vasculitis: 2022 update[J]. Ann Rheum Dis 83(1):30–47
Suárez I, Fünger SM, Kröger S et al (2019) The diagnosis and treatment of Tuberculosis[J]. Dtsch Arztebl Int 116(43):729–735
WHO Guidelines Approved by the Guidelines Review Committee, WHO consolidated guidelines on tuberculosis (2022) 2022
Bossuyt X, Cohen Tervaert JW, Arimura Y et al (2017) Position paper: revised 2017 international consensus on testing of ANCAs in granulomatosis with polyangiitis and microscopic polyangiitis[J]. Nat Rev Rheumatol 13(11):683–692
Qasim A, Patel JB (2022) ANCA Positive Vasculitis, StatPearls, Treasure Island (FL): StatPearls Publishing Copyright © 2022. StatPearls Publishing LLC
Zeng L, Walsh M, Guyatt GH et al (2022) Plasma exchange and glucocorticoid dosing for patients with ANCA-associated vasculitis: a clinical practice guideline[J]. BMJ 376:e064597
Redondo-Rodriguez R, Mena-Vázquez N, Cabezas-Lucena AM et al (2022) Systematic Review and metaanalysis of Worldwide Incidence and Prevalence of Antineutrophil Cytoplasmic Antibody (ANCA) Associated Vasculitis[J]. J Clin Med, 11(9)
Mahmood FS, Schwatz E, Kurrup S et al (2013) A diagnostic dilemma: differentiating between granulomatosis with polyangiitis and tuberculosis[J]. Clin Med (Lond) 13(4):411–413
Khan M, Saleem N, Mahmud SN et al (2022) Granulomatous disorder with Pulmonary and Renal involvement: a diagnostic and therapeutic Dilemma[J]. Cureus 14(3):e23149
Sacoto G, Boukhlal S, Specks U et al (2020) Lung involvement in ANCA-associated vasculitis[J]. Presse Med 49(3):104039
Salvador F (2020) ANCA associated vasculitis[J]. Eur J Intern Med 74:18–28
Critchley JA, Young F, Orton L et al (2013) Corticosteroids for prevention of mortality in people with tuberculosis: a systematic review and meta-analysis[J]. Lancet Infect Dis 13(3):223–237
Youssef J, Novosad SA, Winthrop KL (2016) Infection risk and safety of corticosteroid Use[J]. Rheum Dis Clin North Am, 42(1): 157 – 76, ix-x.
Liu X, Zhang L, Zhang F et al (2021) Prevalence and risk factors of active tuberculosis in patients with rheumatic diseases: a multi-center, cross-sectional study in China[J]. Emerg Microbes Infect 10(1):2303–2312
Jayne D, Walsh M, Merkel PA et al (2022) Plasma exchange and glucocorticoids to delay death or end-stage renal disease in anti-neutrophil cytoplasm antibody-associated vasculitis: PEXIVAS non-inferiority factorial RCT[J]. Health Technol Assess 26(38):1–60
Haris Á, Polner K, Arányi J et al (2021) Incidence and clinical predictors of infections in patients treated with severe systemic ANCA-associated vasculitis[J]. Physiol Int
Garcia-Vives E, Segarra-Medrano A, Martinez-Valle F et al (2020) Prevalence and risk factors for major infections in patients with Antineutrophil cytoplasmic antibody-associated Vasculitis: influence on the Disease Outcome[J]. J Rheumatol 47(3):407–414
Meng T, Shen C, Tang R et al (2022) Clinical features and outcomes of anti-neutrophil cytoplasmic autoantibody-associated vasculitis in Chinese childhood-onset patients[J]. Clin Exp Med 22(3):447–453
Alchi MB, Lever R, Flossmann O et al (2023) Efficacy and safety of low- versus high-dose glucocorticoid regimens for induction of remission of anti-neutrophil cytoplasm antibody-associated vasculitis: a systematic review and meta-analysis[J]. Scand J Rheumatol, : 1–10
Furuta S, Nakagomi D, Kobayashi Y et al (2021) Effect of reduced-dose vs high-dose glucocorticoids added to Rituximab on Remission induction in ANCA-Associated Vasculitis: a randomized clinical Trial[J]. JAMA 325(21):2178–2187
Funding
This research was supported by the Hunan Provincial Natural Science Foundation Youth Foundation (Grant No. 2020JJ5611 and No. 2020JJ8044), Hunan Provincial Health Commission Foundation (Grant No. 202203052625), Changsha Central Hospital Subject of South China University (Grant No. YNKY202101), Scientific research Project of Education Department of Hunan Province (Grant No.22A0321), Hunan Provincial Science and Technology Department Project (Great No. kzd21074 and 2021SK53410).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Rui Wen, **gni **ao, Qin Jiao, and Hebin **e. The first draft of the manuscript was written by Rui Wen and **gni **ao, and Ning Ding, Yong Zhong, Qiong Yuan, Jiali Li and Qi Wang commented on previous versions of the manuscript. All authors read and approved the final manuscript. Jiao Qin and Hebin **e contributed equally to this manuscript. Rui Wen and **gni **ao contributed equally to this manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of Changsha Central Hospital, University of South China. Oral consent for this retrospective study was obtained from all patients or next of kin in the case of death.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Moreover, Jiao Qin and Hebin **e contributed equally to this manuscript, Rui Wen and **gni **ao contributed equally to this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wen, R., **ao, J., Ding, N. et al. Suitability of reduced dose glucocorticoids therapy regimen for antibody-associated vasculitis patients with TB: a retrospective study. Eur J Clin Microbiol Infect Dis 43, 1061–1072 (2024). https://doi.org/10.1007/s10096-024-04807-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-024-04807-w