Abstract
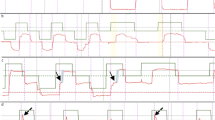
Langerhans cell histiocytosis (LCH) is a rare inflammatory myeloid neoplasm characterized by proliferation of tumor histiocytes that involves multiple organs including central nervous system. The physiopathologic process underlying degenerative neuro-LCH (i.e., DN-LCH) remains imperfectly settled. Since the main clinical features of DN-LCH are cerebellar ataxia and dysexecutive syndrome, eye movements might be disrupted and may help in disease diagnosis and monitoring. We retrospectively analyzed the medical records of twenty DN-LCH patients investigated using eye movement recording (EMR) in our hospital between 2015 and 2018. DN-LCH patients exhibited (i) abnormal gain in visually guided saccades including hypermetric saccades and excessive gain variability -45.0%-, (ii) increased mean antisaccade error rates -66.7%-, (iii) altered smooth pursuit -50.0%-, and (iv) excessive number of square wave jerks-25%- and gaze-evoked nystagmus. Our study suggests that DN-LCH patients present a peculiar pattern of eye movement impairments supporting cerebellar and prefrontal dysfunctions. As a non-invasive method, EMR could therefore be a useful tool for quantitative monitoring of DN-LCH patients. Further studies are warranted to support our findings.




Similar content being viewed by others
References
Yu RC, Chu C, Buluwela L, Chu AC (1994) Clonal proliferation of Langerhans cells in Langerhans cell histiocytosis. Lancet (London, England) 343(8900):767–768
Néel A, Artifoni M, Donadieu J, Lorillon G, Hamidou M, Tazi A (2015) Histiocytose langerhansienne de l’adulte. La Rev Médecine Interne 36(10):658–667
Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ (1999) Langerhans cell histiocytosis: diagnosis, natural history, management, and outcome. Cancer 85(10):2278–2290
Héritier S, Barkaoui M-A, Miron J et al (2018) Incidence and risk factors for clinical neurodegenerative Langerhans cell histiocytosis: a longitudinal cohort study. Br J Haematol 183(4):608–617
Le Guennec L, Martin-Duverneuil N, Mokhtari K et al (2017) Neurohistiocytose langerhansienne. Presse Med 46(1):79–84
Le Guennec L, Decaix C, Donadieu J et al (2014) The cognitive spectrum in neurodegenerative Langerhans cell histiocytosis. J Neurol 261(8):1537–1543
Martin-Duverneuil N, Idbaih A, Hoang-Xuan K et al (2006) MRI features of neurodegenerative Langerhans cell histiocytosis. Eur Radiol 16(9):2074–2082
Kennard C (2011) Disorders of higher gaze control, 1st edn. Elsevier B.V, vol 102
Moscovich M, Okun MS, Favilla C et al (2015) Clinical evaluation of eye movements in spinocerebellar ataxias. J Neuro-Ophthalmol 35(1):16–21
Attoni T, Beato R, Pinto S, Cardoso F (2016) Abnormal eye movements in three types of chorea. Arq Neuropsiquiatr 74(9):761–766
Jung I, Kim J-S (2019) Abnormal eye movements in parkinsonism and movement disorders. J Mov Disord 12(1):1–13
McDowell JE, Dyckman KA, Austin BP, Clementz BA (2008) Neurophysiology and neuroanatomy of reflexive and volitional saccades: evidence from studies of humans. Brain Cogn 68(3):255–270
Baird-Gunning JJD, Lueck CJ (2017) Central control of eye movements. Curr Opin Neurol 31(1):1
Terao Y, Fukuda H, Hikosaka O (2017) What do eye movements tell us about patients with neurological disorders? - An introduction to saccade recording in the clinical setting. Proc Jpn Acad Ser B Phys Biol Sci 93(10):772–801
Ptak R, Müri RM (2013) The parietal cortex and saccade planning: lessons from human lesion studies. Front Hum Neurosci 7:254
Gaymard B, Lynch J, Ploner CJ, Condy C, Rivaud-Péchoux S (2003) The parieto-collicular pathway: anatomical location and contribution to saccade generation. Eur J Neurosci 17(7):1518–1526
Pierrot-Deseilligny C, Müri RM, Nyffeler T, Milea D (2005) The role of the human dorsolateral prefrontal cortex in ocular motor behavior. Ann N Y Acad Sci 1039(1):239–251
Kheradmand A, Zee DS (2011) Cerebellum and ocular motor control. Front Neurol. SEP(September):1–15
Vintonyak O, Gorges M, Müller H-P et al (2017) Patterns of eye movement impairment correlate with regional brain atrophy in neurodegenerative parkinsonism. Neurodegener Dis 17(4–5):117–126
Daye PM, Optican LM, Roze E, Gaymard B, Pouget P (2013) Neuromimetic model of saccades for localizing deficits in an atypical eye-movement pathology. J Transl Med 11(1):125
van Opstal AJ, Kasap B (2019) Maps and sensorimotor transformations for eye-head gaze shifts: role of the midbrain superior colliculus. In: Progress in Brain Research. vol. 249, 19–33
Gaymard B (2012) Cortical and sub-cortical control of saccades and clinical application. Rev Neurol (Paris) 168(10):734–740. https://doi.org/10.1016/j.neurol.2012.07.016
Goffart L, Chen LL, Sparks DL (2003) Saccade dysmetria during functional perturbation of the caudal fastigial nucleus in the monkey. Ann N Y Acad Sci 1004:220–8
Kunimatsu J, Suzuki TW, Tanaka M (2016) Implications of lateral cerebellum in proactive control of saccades. J Neurosci 36(26):7066–7074
Komatsu H, Wurtz RH (1988) Relation of cortical areas MT and MST to pursuit eye movements. I. Localization and visual properties of neurons. J Neurophysiol. 60(2):580–603. https://doi.org/10.1152/jn.1988.60.2.580
Newsome WT, Wurtz RH, Komatsu H (1988) Relation of cortical areas MT and MST to pursuit eye movements. II. Differentiation of retinal from extraretinal inputs. J Neurophysiol. 60(2):604–620
Komatsu H, Wurtz RH (1988) Relation of cortical areas MT and MST to pursuit eye movements. III. Interaction with full-field visual stimulation. J Neurophysiol. 60(2):621–644
Oh AJ, Chen T, Shariati MA, Jehangir N, Hwang TN, Liao YJ (2018) A simple saccadic reading test to assess ocular motor function in cerebellar ataxia. PLoS One 13(11):e0203924 (Hu Y, ed)
Herishanu YO, Sharp JA (1981) Normal square wave jerks. Invest Ophthalmol Vis Sci 20(2):268–272
Katsuki F, Constantinidis C (2012) Unique and shared roles of the posterior parietal and dorsolateral prefrontal cortex in cognitive functions. Front Integr Neurosci 6:17
MacAskill MR, Anderson TJ (2016) Eye movements in neurodegenerative diseases. Curr Opin Neurol 29(1):61–68
Turner TH, Goldstein J, Hamilton JM et al (2011) Behavioral measures of saccade latency and inhibition in manifest and premanifest Huntington’s disease. J Mot Behav 43(4):295–302
Author information
Authors and Affiliations
Contributions
LA: acquisition and interpretation of data, drafting manuscript, and responsibility for the integrity of the study. AI and BG: study concept and design, acquisition and interpretation of data, and study supervision. EB, ADC, FC-A, NM-D, JH, SH, JD, and KH-X: critical revision of manuscript for intellectual content. All read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Ahmed Idbaih reports Research grants from Carthera, Transgene, Sanofi, Air liquide, Servier, Nutritheragene, advisory board for Leo Pharma, Novocure, Boehringer Ingelheim Int, travel funding from Novocure Carthera and Leo Pharma outside the submitted work .
Ethical approval
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Autier, L., Gaymard, B., Bayen, E. et al. Eye movement abnormalities in neurodegenerative langerhans cell histiocytosis. Neurol Sci 43, 6539–6546 (2022). https://doi.org/10.1007/s10072-022-06180-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06180-y