Abstract
Background
Superficial temporal artery–middle cerebral artery (STA–MCA) bypass is a common surgery in treating moyamoya disease (MMD) with occluded MCA. Computational fluid dynamics (CFD) simulation might provide a simple, non-invasive, and low-cost tool to evaluate the efficacy of STA–MCA surgery.
Aim
We aim to quantitatively investigate the treatment efficacy of STA–MCA surgery in improving the blood flow of MMD patients using CFD simulation.
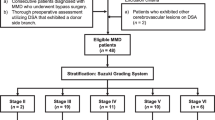
Methods
This retrospective study included 11 MMD patients with occlusion around proximal MCA who underwent STA–MCA bypass surgery. CFD simulation was performed using patient-specific blood pressure and postoperative artery geometry. The volumetric flow rates of STA and the bypass, average flow velocity in the proximal segment of transcranial bypass, transcranial pressure drop, and transcranial flow resistance were measured and compared with a postoperative increment of cerebral blood flow (CBF) in MCA territories derived from perfusion imaging. Per-branch pressure drop from model inlet to bypass branch outlet was calculated.
Results
The volumetric flow rates of STA and the bypass were 80.84 ± 14.54 mL/min and 46.03 ± 4.21 mL/min. Average flow velocity in proximal bypass, transcranial pressure drop, and transcranial flow resistance were 0.19 ± 0.07 m/s, 3.72 ± 3.10 mmHg, and 6.54 ± 5.65 10−8 Pa s m−3. Postoperative mean increment of CBF in MCA territories was 16.03 ± 11.72 mL·100 g−1·min−1. Per-branch pressure drop was 10.96 ± 5.59 mmHg and 7.26 ± 4.25 mmHg in branches with and without stenosis.
Conclusions
CFD simulation results are consistent with CBF observation in verifying the efficacy of STA–MCA bypass, where postoperative stenosis may influence the hemodynamics.




Similar content being viewed by others
Data Availability
Data availability is restricted due to their sensitive nature. Anonymized data are available on reasonable request.
References
Alastruey J, Parker KH, Peiró J, Byrd SM, Sherwin SJ (2007) Modelling the circle of Willis to assess the effects of anatomical variations and occlusions on cerebral flows. J Biomech 40(8):1794–1805
Agarwal V, Singh P, Ahuja CK, Gupta SK, Aggarwal A, Narayanan R (2021) Non-invasive assessment of cerebral microvascular changes for predicting postoperative cerebral hyperperfusion after surgical revascularisation for moyamoya disease: an arterial spin labelling MRI study. Neuroradiol 63(4):563–572
Bai J, Zhao Y-l, Wang R, Zhang D, Wang S, Zhao J-z et al (2012) Regional cerebral perfusion and ischemic status after standard superficial temporal artery–middle cerebral artery (STA–MCA) bypass surgery in ischemic cerebrovascular disease. Child’s Nerv Syst 28(4):579–86
Claassen JAHR, Thijssen DHJ, Panerai RB, Faraci FM (2021) Regulation of cerebral blood flow in humans: physiology and clinical implications of autoregulation. Physiol Rev 101(4):1487–1559
Chnafa C, Brina O, Pereira VM, Steinman DA (2018) Better than nothing: a rational approach for minimizing the impact of outflow strategy on cerebrovascular simulations. Am J Neuroradiol 39(2):337
Connolly F, Alsolivany J, Czabanka M, Vajkoczy P, Valdueza JM, Röhl JE et al (2021) Blood volume flow in the superficial temporal artery assessed by duplex sonography: predicting extracranial-intracranial bypass patency in moyamoya disease. J Neurosurg 135(6):1666–1673
Fujimura M, Bang OY, Kim JS (2016) Moyamoya disease. Front Neurol Neurosci 40:204–220
Funaki T, Takahashi JC, Takagi Y, Kikuchi T, Yoshida K, Mitsuhara T et al (2015) Unstable moyamoya disease: clinical features and impact on perioperative ischemic complications. J Neurosurg JNS 122(2):400–407
Gross BA, Du R (2012) STA–MCA bypass. Acta Neurochir 154(8):1463–1467
Han Q, Huang Y (2020) Quantitative analysis of revascularization in ischemic moyamoya disease via whole-brain computed tomography perfusion: a retrospective single-center study. Med 99(7):e19168
Helthuis JHG, van Doormaal TPC, Amin-Hanjani S, Du X, Charbel FT, Hillen B et al (2020) A patient-specific cerebral blood flow model. J Biomech 98:109445
** S-W, Ha S-K, Lee H-B, Kim S-D, Kim S-H, Lim D-J (2017) Increased ratio of superficial temporal artery flow rate after superficial temporal artery-to-middle cerebral artery anastomosis: can it reflect the extent of collateral flow? World Neurosurg 107:302–307
Karunanithi K, Han C, Lee C-J, Shi W, Duan L, Qian Y (2015) Identification of a hemodynamic parameter for assessing treatment outcome of EDAS in Moyamoya disease. J Biomech 48(2):304–309
Khan NI, Saherwala AA, Chen M, Salehian S, Salahuddin H, Welch BG et al (2019) Prevalence of and risk factors for cerebral microbleeds in moyamoya disease and syndrome in the American population. Cerebrovasc Dis Extra 9(3):139–147
Kuroda S, Nakayama N, Yamamoto S, Kashiwazaki D, Uchino H, Saito H et al (2021) Late (5–20 years) outcomes after STA–MCA anastomosis and encephalo-duro-myo-arterio-pericranial synangiosis in patients with moyamoya disease. J Neurosurg JNS 134(3):909–916
Lan L, Liu H, Ip V, Soo Y, Abrigo J, Fan F et al (2020) Regional high wall shear stress associated with stenosis regression in symptomatic intracranial atherosclerotic disease. Stroke 51(10):3064–3073
Lee M, Guzman R, Bell-Stephens T, Steinberg GK (2010) Intraoperative blood flow analysis of direct revascularization procedures in patients with moyamoya disease. J Cereb Blood Flow Metab 31(1):262–274
Lee M, Zaharchuk G, Guzman R, Achrol A, Bell-Stephens T, Steinberg GK (2009) Quantitative hemodynamic studies in moyamoya disease: a review. Neurosurg Focus FOC 26(4):E5
Leng X, Lan L, Ip HL, Abrigo J, Scalzo F, Liu H et al (2019) Hemodynamics and stroke risk in intracranial atherosclerotic disease. Ann Neurol 85(5):752–764
Liu H, Lan L, Abrigo J, Ip HL, Soo Y, Zheng D et al (2021) Comparison of Newtonian and non-Newtonian fluid models in blood flow simulation in patients with intracranial arterial stenosis. Front Physiol 12:718540
Liu H, Lan L, Leng X, Ip HL, Leung TWH, Wang D et al (2018) Impact of side branches on the computation of fractional flow in intracranial arterial stenosis using the computational fluid dynamics method. J Stroke Cerebrovasc Dis 27(1):44–52
Liu H, Wang D, Leng X, Zheng D, Chen F, Wong LKS, et al. (2020) State-of-the-art computational models of circle of willis with physiological applications: a review. IEEE Access 8:156261–73
Mesiwala AH, Sviri G, Fatemi N, Britz GW, Newell DW (2008) Long-term outcome of superficial temporal artery–middle cerebral artery bypass for patients with moyamoya disease in the US. Neurosurg Focus FOC 24(2):E15
Miller C, Armonda R (2014) The participants in the international multi-disciplinary consensus conference on multimodality M. monitoring of cerebral blood flow and ischemia in the critically ill. Neurocrit Care 21(2):121–8
Morisawa H, Kawamata T, Kawashima A, Hayashi M, Yamaguchi K, Yoneyama T et al (2013) Hemodynamics and changes after STA–MCA anastomosis in moyamoya disease and atherosclerotic cerebrovascular disease measured by micro-Doppler ultrasonography. Neurosurg Rev 36(3):411–419
Morris PD, Narracott A, von Tengg-Kobligk H, Silva Soto DA, Hsiao S, Lungu A et al (2016) Computational fluid dynamics modelling in cardiovascular medicine. Heart 102(1):18
Murayama Y, Fujimura S, Suzuki T, Takao H (2019) Computational fluid dynamics as a risk assessment tool for aneurysm rupture. Neurosurg Focus FOC 47(1):E12
Naqvi J, Yap KH, Ahmad G, Ghosh J (2013) Transcranial Doppler ultrasound: a review of the physical principles and major applications in critical care. Int J Vasc Med 2013:629378
Nariai T, Matsushima Y, Imae S, Tanaka Y, Ishii K, Senda M et al (2005) Severe haemodynamic stress in selected subtypes of patients with moyamoya disease: a positron emission tomography study. J Neurol Neurosurg Psychiatry 76(5):663
Ozgur BM, Aryan HE, Levy ML (2006) Indirect revascularisation for paediatric moyamoya disease: the EDAMS technique. J Clin Neurosci 13(1):105–108
Reymond P, Merenda F, Perren F, Rüfenacht D, Stergiopulos N (2009) Validation of a one-dimensional model of the systemic arterial tree. Am J Physiol-Heart Circ Physiol 297(1):H208–H222
Research Committee on the P (2012) Treatment of Spontaneous Occlusion of the Circle of W, Health Labour Sciences Research Grant for Research on Measures for Intractable D. Guidelines for Diagnosis and Treatment of Moyamoya Disease (Spontaneous Occlusion of the Circle of Willis). Neurol Med-Chirurg 52(5):245–66
Sebök M, Esposito G, Niftrik CHBv, Fierstra J, Schubert T, Wegener S, et al. (2022) Flow augmentation STA–MCA bypass evaluation for patients with acute stroke and unilateral large vessel occlusion: a proposal for an urgent bypass flowchart. J Neurosurg. 1–9. https://doi.org/10.3171/2021.10.JNS21986
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360(12):1226–1237
So Y, Lee H-Y, Kim S-K, Lee JS, Wang K-C, Cho B-K et al (2005) Prediction of the clinical outcome of pediatric moyamoya disease with postoperative basal/acetazolamide stress brain perfusion SPECT after revascularization surgery. Stroke 36(7):1485–1489
Sternheim D, Power DA, Samtani R, Kini A, Fuster V, Sharma S (2021) Myocardial bridging: diagnosis, functional assessment, and management: JACC state-of-the-art review. J Am Coll Cardiol 78(22):2196–2212
Tanaka K, Takao H, Suzuki T, Fujimura S, Uchiyama Y, Ishibashi T, et al. (2018) Relationship between hemodynamic parameters and cerebral aneurysm initiation. 2018 40th Ann IntConf IEEE Eng Med Biol Soc (EMBC) https://doi.org/10.1109/EMBC.2018.8512466
Tian B, Xu B, Liu Q, Hao Q, Lu J (2013) Adult Moyamoya disease: 320-Multidetector row CT for evaluation of revascularization in STA–MCA bypasses surgery. Eur J Radiol 82(12):2342–2347
Wan M, Han C, **an P, Yang W-Z, Li D-S, Duan L (2015) Moyamoya disease presenting with subarachnoid hemorrhage: clinical features and neuroimaging of a case series. Br J Neurosurg 29(6):804–810
Wang G, Xa Zhang, Wang B, Wen Y, Chen S, Liu J et al (2020) Flow evaluation of STA–MCA bypass using quantitative ultrasonography: an alternative to standard angiography for follow up of bypass graft. J Stroke Cerebrovasc Dis 29(9):105000
Wu M, Huang Z, Zhang D, Wang L, Sun J, Wang S et al (2011) Color Doppler hemodynamic study of the superficial temporal arteries in superficial temporal artery–middle cerebral artery (STA–MCA) bypass surgery for moyamoya disease. World Neurosurg 75(2):258–263
Zhao WG, Luo Q, Jia JB, Yu JL (2013) Cerebral hyperperfusion syndrome after revascularization surgery in patients with moyamoya disease. Br J Neurosurg 27(3):321–325
Zhong L, Zhang J-M, Su B, Tan RS, Allen JC, Kassab GS (2018) Application of patient-specific computational fluid dynamics in coronary and intra-cardiac flow simulations: challenges and opportunities. Front Physiol 9. https://doi.org/10.3389/fphys.2018.00742
Zhu F, Karunanithi K, Qian Y, Mao Y, Xu B, Gu Y et al (2015) Assessing surgical treatment outcome following superficial temporal artery to middle cerebral artery bypass based on computational haemodynamic analysis. J Biomech 48(15):4053–4058
Zhu F-P, Zhang Y, Higurashi M, Xu B, Gu Y-X, Mao Y et al (2014) Haemodynamic analysis of vessel remodelling in STA–MCA bypass for moyamoya disease and its impact on bypass patency. J Biomech 47(8):1800–1805
Acknowledgements
We would like to acknowledge Dr. Syed Aziz Shah from Coventry University, UK, for his valuable advice in scientific writing.
Funding
This research was funded by the National Key Research and Development Program of China (Grant No. 2018YFE0198400).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethics committee of The Second Affiliated Hospital, Zhejiang University School of Medicine (Date 20 August 2020/ No.12020001732).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery—Ischemia
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Liu, H., Xu, M. et al. Efficacy assessment of superficial temporal artery–middle cerebral artery bypass surgery in treating moyamoya disease from a hemodynamic perspective: a pilot study using computational modeling and perfusion imaging. Acta Neurochir 165, 613–623 (2023). https://doi.org/10.1007/s00701-022-05455-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05455-9