Abstract
Background
Minimally invasive endoscopic hematoma evacuation (MEHE) is an emerging surgical technique for treating spontaneous supratentorial intracerebral haemorrhage (SSICH). Multiple studies, analysing whether the outcome after such a procedure is improved, are still ongoing.
Method
We herein present the indications, advantages, and perioperative considerations for the surgical technique of MEHE applied at our institution.
Conclusion
MEHE with a view through a transparent brain access device is a valid and safe approach for the surgical evacuation of SSICH.





Similar content being viewed by others
References
Hanley DF, Thompson RE, Rosenblum M, Yenokyan G, Lane K, McBee N, Mayo SW, Bistran-Hall AJ, Gandhi D, Mould WA, Ullman N, Ali H, Carhuapoma JR, Kase CS, Lees KR, Dawson J, Wilson A, Betz JF, Sugar EA, Hao Y, Avadhani R, Caron JL, Harrigan MR, Carlson AP, Bulters D, LeDoux D, Huang J, Cobb C, Gupta G, Kitagawa R, Chicoine MR, Patel H, Dodd R, Camarata PJ, Wolfe S, Stadnik A, Money PL, Mitchell P, Sarabia R, Harnof S, Barzo P, Unterberg A, Teitelbaum JS, Wang W, Anderson CS, Mendelow AD, Gregson B, Janis S, Vespa P, Ziai W, Zuccarello M, Awad IA (2019) Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet 393:1021–1032. https://doi.org/10.1016/s0140-6736(19)30195-3
Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, Scott PA, Selim MH, Woo D (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:2032–2060. https://doi.org/10.1161/str.0000000000000069
Kellner CP, Song R, Ali M, Nistal DA, Samarage M, Dangayach NS, Liang J, McNeill I, Zhang X, Bederson JB, Mocco J (2021) Time to evacuation and functional outcome after minimally invasive endoscopic intracerebral hemorrhage evacuation. Stroke 52:e536–e539. https://doi.org/10.1161/STROKEAHA.121.034392
Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, Karimi A, Shaw MD, Barer DH (2005) Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet 365:387–397. https://doi.org/10.1016/s0140-6736(05)17826-x
Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM (2013) Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet 382:397–408. https://doi.org/10.1016/s0140-6736(13)60986-1
Morgenstern LB, Demchuk AM, Kim DH, Frankowski RF, Grotta JC (2001) Rebleeding leads to poor outcome in ultra-early craniotomy for intracerebral hemorrhage. Neurology 56:1294–1299. https://doi.org/10.1212/wnl.56.10.1294
Scaggiante J, Zhang X, Mocco J, Kellner CP (2018) Minimally Invasive Surgery for Intracerebral Hemorrhage. Stroke 49:2612–2620. https://doi.org/10.1161/strokeaha.118.020688
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ (2010) Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 9:167–176. https://doi.org/10.1016/s1474-4422(09)70340-0
** G, Keep RF, Hoff JT (2006) Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol 5:53–63. https://doi.org/10.1016/s1474-4422(05)70283-0
Yao Z, Hu X, You C, He M (2018) Effect and feasibility of endoscopic surgery in spontaneous intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg 113:348-356.e342. https://doi.org/10.1016/j.wneu.2018.02.022
Funding
TJH receives a personal MD PhD Scholarship jointly from the Swiss National Science Foundation and the Swiss Academy of Medical Sciences (SNF 323630_207030). A research grant from the Swiss Heart Foundation (FF19092) in the setting of a pilot trial (NCT04805177) was obtained. The funders had no involvement in the conception, design and decision for publication of this work.
Author information
Authors and Affiliations
Contributions
Conception and design: RG and JS. Drafting the manuscript: TJH and JS. Critically revising the manuscript: all authors. Permission to submit manuscript: all authors. Images and videos: TJH, JS, RG. Study supervision: RG and JS.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the local ethics committee (Ethikkommission Nordwestschweiz) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The pilot trial, in which this technique was used, was approved by the local ethics committee (EKNZ-2021–00161).
Consent to participate
Informed consent was obtained from all patients or their relatives/legal guardians included in the pilot trial.
Conflict of interest
The authors declare no competing interests.
Additional information
10 key point summary
• MEHE shows promising results, while the indication remains relative, it can be recommended within study protocols for patients with a hematoma volume > 20 mL exhibiting focal neurological deficits.
• It seems that early (within 6–24 h from ictus) MEHE helps improve mortality and morbidity rates.
• A transparent trocar enables 360° view of the surrounding brain parenchyma and hematoma cavity reducing the risk for postoperative residual hematoma and brain tissue damage.
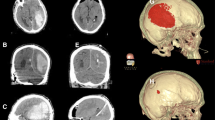
• The shortest path to the hematoma cavity across the parenchyma using neuronavigation should be chosen.
• The transparent VSBAD should be inserted at 2/3 depth of the hematoma cavity where the evacuation is started and thereafter continued proximally.
• Through endoscopic view, the hematoma can be removed safely in a minimal invasive fashion.
• Active bleeding sites are coagulated with the endoscopic bipolar, and, if needed, Floseal® can be applied.
• Immediate perioperative imaging is advised to confirm satisfactory hematoma evacuation and rule out acute rebleeding.
• Rigorous blood pressure regimes should be implemented to avoid hematoma recurrence.
• Experience in endoscopic assisted surgery is required; however, the learning curve is steep.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Other
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 118149 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hallenberger, T.J., Guzman, R. & Soleman, J. Minimally invasive image-guided endoscopic evacuation of intracerebral haemorrhage: How I Do it. Acta Neurochir 165, 1597–1602 (2023). https://doi.org/10.1007/s00701-022-05326-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05326-3