Abstract
Background
The subaxial spine has high risk of fatal damage by trauma and thereby requires more accurate and aggressive treatment. For the proper treatment and predicting the prognosis, the evaluation to reveal the risk factors for the prognosis is important. We analyzed the various factors contributing to the prognosis in distractive extension injuries of the subaxial cervical spine.
Methods
The study included 103 patients who were diagnosed as distractive extension injury of subaxial cervical spine. We evaluate the patient age, sex, cause of injury, initial neurological impairment, number and portion of injured segment, spinal stenosis, extent of soft tissue damage, ossification of the posterior longitudinal ligament, and degenerative spondylosis as a prognostic factor. To analyze the factor related with prognosis, the subjects were divided into group A, in which patients had neurological recovery ≥grade 2 on the ASIA scale or showed normal in final follow-up and group B, in which patients have no neurological recovery.
Results
Prognosis was not associated with age, sex, and cause of injury (P = 0.677, 0.541, and 0.965, respectively). Prognosis was poor in cases with spinal stenosis (P = 0.009), soft tissue damage ≥grade 3 on magnetic resonance imaging (MRI) (P = 0.002), or severe neurological impairment (P ≤ 0.001). Logistic regression analysis also showed that prognosis was poor in cases with spinal stenosis (OR 5.03; 95 % CI 1.20–16.93), soft tissue damage ≥grade 3 on MRI (OR 7.63; 95 % CI 1.86–31.34), or severe neurological impairment (ASIA C, D, OR 0.59, 95 % CI 0.14–2.41; ASIA A, B, OR 18.43, 95 % CI 1.64–207.69).
Conclusion
The prognosis of patients with distractive extension injury of the subaxial cervical spine was poor in cases with spinal stenosis, severe soft tissue damage in MRI findings or severe initial neurological impairment.

Similar content being viewed by others
References
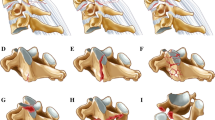
Allen BL Jr, Ferguson RL, Lehmann TR, O’Brien RP (1982) A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine 197(1):1–27 (Phila Pa 1976)
Song KJ, Kim GH, Lee KB (2008) The efficacy of the modified classification system of soft tissue injury in extension injury of the lower cervical spine. Spine 33(15):E488–E493
Song KJ, Lee KB (2008) The significance of soft tissue injury in lower cervical spine trauma. Neurosurg Q 18:28–33
Marar BC (1974) Hyperextension injuries of the cervical spine. The pathogenesis of damage to the spinal cord. J Bone Joint Surg Am 56:1655–1662
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, Haak M, Hudson LM, Priebe MM (2003) International standards for neurological classification of spinal cord injury. J Spinal Cord Med 26:S50–S56
Herzog RJ, Wiens JJ, Dillingham MF, Sontag MJ (1991) Normal cervical spine morphometry and cervical spinal stenosis in asymptomatic professional football players: plain film radiography, multiplanar computed tomography and magnetic resonance imaging. Spine 16:178–186
Pavlov H, Torg JS, Robie B, Jahre C (1987) Cervical spinal stenosis: determination with vertebral body ratio method. Radiology 164:771–775
Song KJ, Choi BW, Lee KB, Chang H (2012) The relationship between soft tissue damages and neurologic deficits in distractive extension injury of the lower cervical spine. J Korean Orthop Assoc 47:15–20
Taylor AR, Blackwood W (1948) Paraplegia in hyperextension cervical injuries with normal radiographic appearances. J Bone Jont Surg Br 30B(2):245–248
Herkowitz HN (2011) Rothman-Simeone. The Spine, 6th edn. Elsevier
Friedenberg BZB, Jack E (1959) Distractive extension injury. H. Newton Spencer; S. C. Tolentino: degenerative changes in the cervical spine. J Bone Joint Surg Am 41:61–102
Stauffer ES, MacMillan M (1996) Fractures and dislocations of the cervical spine. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD (eds) Rockwood and Green’s fractures in adults, 4th edn. Lippincott-Raven, Philadelphia, pp 1475–1477
Hohl M (1974) Soft-tissue injuries of the neck in automobile accidents. Factors influencing prognosis. J Bone Joint Surg Am 56:1675–1682
Eismont FJ, Clifford S, Goldberg M, Green B (1984) Cervical sagittal spinal canal size in spine injury. Spine 9:663–666 (Phila Pa 1976)
Nakashima H, Yukawa Y, Ito K, Machino M, Kato F (2011) Mechanical patterns of cervical injury influence postoperative neurological outcome: a verification of the allen system. Spine 15;36(6):E441–E446 (Phila Pa 1976)
Acknowledgments
2013 Inje University research grant funds were received to support this work.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Song, KJ., Choi, BW., Park, CI. et al. Prognostic factors in distractive extension injuries of the subaxial cervical spine. Eur J Orthop Surg Traumatol 25 (Suppl 1), 101–106 (2015). https://doi.org/10.1007/s00590-014-1479-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1479-z