Abstract
Purpose
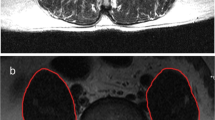
The retrospective study aimed to report the surgical technique and clinic-radiological outcomes of endoscopic anterior to psoas interbody lumbar fusion through the retroperitoneal approach with direct and indirect decompression.
Methods
We retrospectively analyzed the results of clinical parameters of patients who underwent endoscopic anterior to psoas interbody lumbar fusion between June 2013 and June 2022. Clinical outcomes were evaluated by the visual analog scale (VAS) and Oswestry Disability Index (ODI) scores. The radiological outcomes were measured and statistically compared in disc height index (DHI), whole lumbar lordosis (WLL), pelvic Incidence (PI), pelvic tilt (PT), Segmental lordosis (SL), the sagittal vertical axis (SVA).
Results
A total of 35 patients were selected for the procedure ranging in age from 51 to 84 years with 17.83 ± 8.85 months follow-up. The mean operation time in lateral position for one level was 162.96 ± 35.76 min (n = 24), and 207.73 ± 66.60 min for two-level fusion. The mean endoscopic time was 32.83 ± 17.71 min per level, with a total estimated blood loss of 230.57 ± 187.22 cc. The mean postoperative VAS back, leg pain score and ODI improved significantly compared to the preoperative values; Radiological data showed significant change in WLL, SL, DHI, PI, PT, and SS; however, there is no significant difference in SVA postoperatively. Subgroup analysis for the radiographic data showed 50 mm length cage has significantly improved for the DHI, SS and SVA compare to 40 mm length cage. The subgroup analysis results showed that hypertensive patients had significantly higher proportion in the incomplete fusion group compare to complete fusion group at one-year follow-up.
Outcomes
The endoscopic anterior to psoas interbody lumbar fusion achieves satisfactory indirect and direct decompression. This convergent technique presents an effective choice for treating lumbar instability associated with disc herniations and foraminal stenosis, thus complementing the indications for oblique lumbar interbody fusion.









Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request. The data are not publicly available due to privacy and ethical restrictions.
References
Reisener M-J, Pumberger M, Shue J, Girardi FP, Hughes AP (2020) Trends in lumbar spinal fusion—a literature review. J Spine Surg 6:752–761
Mayer MH (1997) A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine 22(6):691–699. https://doi.org/10.1097/00007632-199703150-00023
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1:2–18. https://doi.org/10.3978/j.issn.2414-469X.2015.10.05
Qureshi R, Puvanesarajah V, Jain A, Shimer AL, Shen FH, Hassanzadeh H (2017) A comparison of anterior and posterior lumbar interbody fusions complications, readmissions, discharge dispositions, and costs. Spine 42:1865–1870. https://doi.org/10.1097/brs.0000000000002248
Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7:379–386. https://doi.org/10.3171/spi-07/10/379
Fritzell P, Hagg O, Nordwall A (2003) Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. a report from the swedish lumbar spine study group. Eur Spine J 12:178–189. https://doi.org/10.1007/s00586-002-0493-8
Yang PL, Zang QJ, Kang J, Li HP, He XJ (2016) Comparison of clinical efficacy and safety among three surgical approaches for the treatment of spinal tuberculosis: a meta-analysis. Eur Spine J 25:3862–3874. https://doi.org/10.1007/s00586-016-4546-9
Makanji H, Schoenfeld AJ, Bhalla A, Bono CM (2018) Critical analysis of trends in lumbar fusion for degenerative disorders revisited: influence of technique on fusion rate and clinical outcomes. Eur Spine J 27:1868–1876. https://doi.org/10.1007/s00586-018-5544-x
Kepler CK, Vaccaro AR, Hilibrand AS, Greg Anderson D, Rihn JA, Albert TJ, Radcliff KE (2014) National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine 39(19):1584–1589. https://doi.org/10.1097/BRS.0000000000000486
Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS (2019) Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the united states, 2004 to 2015. Spine 44:369–376. https://doi.org/10.1097/brs.0000000000002822
Malham GM, Parker RM, Goss B, Blecher CM, Ballok ZE (2014) Indirect foraminal decompression is independent of metabolically active facet arthropathy in extreme lateral interbody fusion. Spine 39(22):E1303–E1310. https://doi.org/10.1097/BRS.0000000000000551
Adogwa O, Elsamadicy AA, Han JL, Cheng J, Karikari I, Bagley CA (2016) Do measures of surgical effectiveness at 1 year after lumbar spine surgery accurately predict 2-year outcomes? J Neurosurg Spine 25:689–696. https://doi.org/10.3171/2015.8.Spine15476
Jung JM, Chung CK, Kim CH, Yang SH, Ko YS, Choi Y (2021) Intraoperative Radiographs in single-level lateral lumbar interbody fusion can predict radiographic and clinical outcomes of follow-up 2 years after surgery. Spine 46:772–780. https://doi.org/10.1097/brs.0000000000003889
Katz AD, Mancini N, Karukonda T, Greenwood M, Cote M, Moss IL (2019) Approach-based Comparative and predictor analysis of 30-day readmission, reoperation, and morbidity in patients undergoing lumbar interbody fusion using the ACS-NSQIP dataset. Spine 44:432–441. https://doi.org/10.1097/brs.0000000000002850
Heo DH, Choi WS, Park CK, Kim JS (2016) Minimally invasive oblique lumbar interbody fusion with spinal endoscope assistance: technical note. World Neurosurg 96:530–536. https://doi.org/10.1016/j.wneu.2016.09.033
Kim JS, Seong JH (2017) Endoscope-assisted oblique lumbar interbody fusion for the treatment of cauda equina syndrome: a technical note. Eur Spine J 26:397–403. https://doi.org/10.1007/s00586-016-4902-9
Heo DH, Kim JS (2017) Clinical and radiological outcomes of spinal endoscopic discectomy-assisted oblique lumbar interbody fusion: preliminary results. Neurosurg Focus 43:E13. https://doi.org/10.3171/2017.5.Focus17196
Aguirre AO, Soliman MAR, Azmy S, Khan A, Jowdy PK, Mullin JP, Pollina J (2022) Incidence of major and minor vascular injuries during lateral access lumbar interbody fusion procedures: a retrospective comparative study and systematic literature review. Neurosurg Rev 45:1275–1289. https://doi.org/10.1007/s10143-021-01699-8
Pham MH, Hassan O, Diaz-Aguilar LD, Lehman RA (2021) Complications associated with oblique lumbar interbody fusion at l5-s1: a systematic review of the literature. Neurosurg Open. https://doi.org/10.1093/neuopn/okab018
Phan K, Joshua X, Scherman DB, Rao PJ, Mobbs RJ (2017) Anterior lumbar interbody fusion with and without an “access surgeon”: a systematic review and meta-analysis. Spine 42(10):E592–E601. https://doi.org/10.1097/BRS.0000000000001905
Joseph JR, Smith BW, La Marca F, Park P (2015) Comparison of complication rates of minimally invasive transforaminal lumbar interbody fusion and lateral lumbar interbody fusion: a systematic review of the literature. Neurosurg Focus 39:E4. https://doi.org/10.3171/2015.7.Focus15278
Berry CA, Thawrani DP, Makhoul FR (2021) Inclusion of L5–S1 in oblique lumbar interbody fusion-techniques and early complications-a single center experience. Spine J 21:418–429. https://doi.org/10.1016/j.spinee.2020.10.016
Kim KS, Chin DK, Park JY (2009) Herniated nucleus pulposus in isthmic spondylolisthesis: higher incidence of foraminal and extraforaminal types. Acta Neurochir (Wien) 151:1445–1450. https://doi.org/10.1007/s00701-009-0411-5
Jenkins NW, Parrish JM, Nolte MT, Jadczak CN, Geoghegan CE, Mohan S, Hrynewycz NM, Singh K (2021) Charlson comorbidity index: an inaccurate predictor of minimally invasive lumbar spinal fusion outcomes. Int J Spine Surg 15:770–779. https://doi.org/10.14444/8099
Funding
This research is supported by a grant from Korea’s Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (Grant No: HC20C0163). The funder had no role in the design of the study or collection, analysis, or interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
YT Liu and CW Park are all the Co-first authors with the same contribution to this research.
Corresponding author
Ethics declarations
Conflict interest
The corresponding author, **-Sung Kim, is a consultant of Richard Wolf, GmbH, and Elliquence, LLC. The other authors have no conflicts of interest to declare.
Ethical approval
IRB approval was obtained from Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Y., Park, C.W., Sharma, S. et al. Endoscopic anterior to psoas lumbar interbody fusion: indications, techniques, and clinical outcomes. Eur Spine J 32, 2776–2795 (2023). https://doi.org/10.1007/s00586-023-07700-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07700-w