Abstract
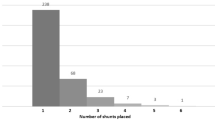
Further study is needed to determine the safest mode of delivery and anesthetic management for parturients with ventriculoperitoneal shunts (VP). Prior recommendation for delivery in women with ventriculoperitoneal shunts was cesarean delivery. However, both vaginal delivery and neuraxial anesthesia have been shown to be safe in women with appropriately functioning VP shunts. We present a case series of parturients with VP shunt. Parturients with VP shunts were identified and VP shunt placement indications, neurologic symptoms during pregnancy, delivery mode, anesthetic type, and postpartum complications were reviewed. Forty patients were identified, and fifteen women with twenty deliveries were included. Two women experienced neurological symptoms during pregnancy and one required postpartum shunt revision for blurry vision and ataxia. There were ten cesarean deliveries and ten vaginal deliveries (eight normal spontaneous, one vacuum assisted, and one forceps assisted). Assisted vaginal deliveries were performed to decrease Valsalva including the patient with neurological symptoms related to shunt malfunction. Of the vaginal deliveries, six (60%) had epidural analgesia. Anesthesia for cesarean delivery included neuraxial anesthesia (n = 5) and general anesthesia (n = 5). In our cohort, women with VP shunt received neuraxial blockade without complication. Neuraxial techniques should be offered to women with appropriately functioning VP shunt.

Similar content being viewed by others
Data Availability
All data generated or analysed during this study are included in this published article.
References
Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F, Piatt J, Haines S, Schiff S, Cochrane D, Steinbok P, MacNeil N. Long-term follow-up data from the Shunt Design Trial. Pediatr Neurosurg. 2000;33(5):230–6. https://doi.org/10.1159/000055960.
Landwehr JB Jr, Isada NB, Pryde PG, Johnson MP, Evans MI, Canady AI. Maternal neurosurgical shunts and pregnancy outcome. Obstet Gynecol. 1994;83(1):134–7.
Rajagopalan S, Gopinath S, Trinh VT, Chandrasekhar S. Anesthetic considerations for labor and delivery in women with cerebrospinal fluid shunts. Int J Obstet Anesth. 2017;30:23–9. https://doi.org/10.1016/j.ijoa.2017.01.005.
Bursac D, Kulas T, Persec J, Persec Z, Duić Z, Partl JZ, Glavić Z, Hrgović Z, Bojanić K. Pregnancy and vaginal delivery in epidural analgesia in woman with cerebrospinal fluid shunt. Coll Antropol. 2013;37(4):1343–5.
Freo U, Pitton M, Carron M, Ori C. Anesthesia for urgent sequential ventriculoperitoneal shunt revision and cesarean delivery. Int J Obstet Anesth. 2009;18(3):284–7. https://doi.org/10.1016/j.ijoa.2009.02.011.
Wisoff JH, Kratzert KJ, Handwerker SM, Young BK, Epstein F. Pregnancy in patients with cerebrospinal fluid shunts: report of a series and review of the literature. Neurosurgery. 1991;29(6):827–31.
Cusimano MD, Meffe FM, Gentili F, Sermer M. Management of pregnant women with cerebrospinal fluid shunts. Pediatr Neurosurg. 1991;17(1):10–3. https://doi.org/10.1159/000120558.
Palop R, Choed-Amphai E, Miller R. Epidural anesthesia for delivery complicated by benign intracranial hypertension. Anesthesiology. 1979;50(2):159–60. https://doi.org/10.1097/00000542-197902000-00017.
Celik M, Kizilkaya M, Dostbil A, Dogan N, Parlak M, Can FK, Bayar M. Meningitis following spinal anaesthesia in an obstetric patient. Trop Doct. 2014;44(3):179–81. https://doi.org/10.1177/0049475514529760.
Leffert LR, Schwamm LH. Neuraxial anesthesia in parturients with intracranial pathology: a comprehensive review and reassessment of risk. Anesthesiology. 2013;119(3):703–18. https://doi.org/10.1097/ALN.0b013e31829374c2.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Wehrle, A.A., Welch, T.L., Hirte, I.L. et al. Obstetric and anesthetic management in parturients with ventriculoperitoneal shunt: a case series. J Anesth (2024). https://doi.org/10.1007/s00540-024-03369-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00540-024-03369-7