Abstract
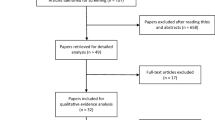
Parameter reproducibility in photobiomodulation therapy (PBMT) is still scarce in literature for the management of oral mucositis (OM). This study aimed to identify the most used PBMT dosimetry parameters (DP) and their efficacy in OM management after preconditioning for hematopoietic stem cell transplantation (HSCT). This research was conducted according to the PRISMA guidelines. The search for primary studies was in PubMed/MEDLINE, Web of Science, Embase, BVS, and Cochrane Library. Gray literature was verified on BDTD-Ibict and Open Gray. A total of 1044 studies were identified. Nine met the eligibility criteria for qualitative assessment and 7 for meta-analysis. The studies involved 396 patients submitted to preconditioning for HSCT, 211 with PBMT and 185 without PBMT in the OM management. The WHO scale was the most used to assess OM degree. The most used parameters were 660-nm wavelength, 40-mw power, 0.16-J energy, 1-W/cm2 power density, 4-J/cm2 energy density, and 0.04-cm2 spot size. The meta-analysis demonstrated that PBMT decreased the severity of OM, with a protection factor 20% higher than the control group (without PBMT), and when the parameters are similar to the DP mentioned, the protection factor increases to 94%. These most used DP with similarity seem to be a therapeutic strategy for the management of OM in this population.



Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Kusiak A, Jereczek-Fossa B, Cichońska D, Alterio D (2020) Oncological-therapy related oral mucositis as an interdisciplinary problem—literature review. Int J Environ Health Res 17(7):2464. https://doi.org/10.3390/ijerph17072464
Lalla RV, Bowen J, Barasch A, Elting L, Epstein J, Keefe DM, McGuire DB, Migliorati C, Nicolatou-Galitis O, Peterson DE, Raber-Durlacher JE, Sonis ST, Elad S (2014) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 120(10):1453–1461. https://doi.org/10.1002/cncr.28592
Sonis S (2009) Mucositis: the impact, biology and therapeutic opportunities of oral mucositis. Oral Oncol 45(12):1015–1020. https://doi.org/10.1016/j.oraloncology.2009.08.006
Santos P, Messaggi A, Mantesso A, Magalhães M (2009) Oral mucositis: recent perspectives on prevention and treatment. RBO 57(3):339–344
Avci S, Sari HY (2019) Effect of an evidence-based nursing intervention on the diagnosis of oral mucositis in the pediatric stem cell transplant unit. Asia Pac J Oncol Nurs 6:292–299. https://doi.org/10.4103/apjon.apjon_5_19
Scully C, Sonis S, Diz PD (2006) Oral mucositis. Oral Dis 12(3):229–241. https://doi.org/10.1111/j.1601-0825.2006.01258.x
Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM, Bowen J, Gibson R, Saunders DP, Zadik Y, Ariyawardana A, Correa ME, Ranna V, Bossi P (2020) Mucositis guidelines leadership group of the multinational association of supportive care in cancer and international society of oral oncology (MASCC/ISOO). MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 126(19):4423–4431. https://doi.org/10.1002/cncr.33100
Legouté F, Bensadoun R, Seegers V, Pointreau Y, Caron D, Lang P, Prévost A, Martin L, Schick U, Morvant B, Capitain O, Calais G, Jadaud E (2019) Low-level laser therapy in treatment of chemoradiotherapy-induced mucositis in head and neck cancer: results of a randomised, triple blind, multicentre phase III trial. Radiat Oncol 14(1):83. https://doi.org/10.1186/s13014-019-1292-2
Tunér J, Jenkins PA (2016) Parameter reproducibility in photobiomodulation. Photomed Laser Surg 34(3):91–92. https://doi.org/10.1089/pho.2016.4105
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group (2016) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:7647. https://doi.org/10.1136/bmj.g7647
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:5928. https://doi.org/10.1136/bmj.d5928
Carvalho AP, Silva V, Grande AJ (2013) Avaliação do risco de viés de ensaios clínicos randomizados pela ferramenta da colaboração Cochrane. Diagn Tratamento 18(1):38–44
Antunes HS, de Azevedo AM, da Silva Bouzas LF, Adão CA, Pinheiro CT, Mayhe R, Pinheiro LH, Azevedo R, D’Aiuto de Matos V, Rodrigues PC, Small IA, Zangaro RA, Ferreira CG (2007) Low-power laser in the prevention of induced oral mucositis in bone marrow transplantation patients: a randomized trial. Blood 109(5):2250–5. https://doi.org/10.1182/blood-2006-07-035022
Cowen D, Tardieu C, Schubert M, Peterson D, Resbeut M, Faucher C, Franquin JC (1997) Low energy Helium-Neon laser in the prevention of oral mucositis in patients undergoing bone marrow transplant: results of a double blind randomized trial. Int J Radiat Oncol Biol Phys 38(4):697–703. https://doi.org/10.1016/s0360-3016(97)00076-x
Hodgson BD, Margolis DM, Salzman DE, Eastwood D, Tarima S, Williams LD, Sande JE, Vaughan WP, Whelan HT (2012) Amelioration of oral mucositis pain by NASA near-infrared light-emitting diodes in bone marrow transplant patients. Support Care Cancer 20(7):1405–1415. https://doi.org/10.1007/s00520-011-1223-8
Khouri VY, Stracieri AB, Rodrigues MC, Moraes DA, Pieroni F, Simões BP, Voltarelli JC (2009) Use of therapeutic laser for prevention and treatment of oral mucositis. Braz Dent J 20(3):215–220. https://doi.org/10.1590/s0103-64402009000300008
Salvador DRN, Soave DF, Sacono NT, de Castro EF, Silva GBL, Silva LPE, Silva TA, Valadares MC, Mendonça EF, Batista AC (2017) Effect of photobiomodulation therapy on reducing the chemo-induced oral mucositis severity and on salivary levels of CXCL8/interleukin 8, nitrite, and myeloperoxidase in patients undergoing hematopoietic stem cell transplantation: a randomized clinical trial. Lasers Med Sci 32(8):1801–1810. https://doi.org/10.1007/s10103-017-2263-1
Schubert MM, Eduardo FP, Guthrie KA, Franquin JC, Bensadoun RJ, Migliorati CA, Lloid CM, Eduardo CP, Walter NF, Marques MM, Hamdi M (2007) A phase III randomized double-blind placebo-controlled clinical trial to determine the efficacy of low level laser therapy for the prevention of oral mucositis in patients undergoing hematopoietic cell transplantation. Support Care Cancer 15(10):1145–1154. https://doi.org/10.1007/s00520-007-0238-7
Silva GB, Mendonça EF, Bariani C, Antunes HS, Silva MA (2011) The prevention of induced oral mucositis with low-level laser therapy in bone marrow transplantation patients: a randomized clinical trial. Photomed Laser Surg 29(1):27–31. https://doi.org/10.1089/pho.2009.2699
Silva GB, Sacono NT, Othon-Leite AF, Mendonça EF, Arantes AM, Bariani C, Duarte LG, Abreu MH, Queiroz-Júnior CM, Silva TA, Batista AC (2015) Effect of low-level laser therapy on inflammatory mediator release during chemotherapy-induced oral mucositis: a randomized preliminary study. Lasers Med Sci 30(1):117–126. https://doi.org/10.1007/s10103-014-1624-2
Silva LC, Sacono NT, Freire Mdo C, Costa LR, Batista AC, Silva GB (2015) The impact of Low-level laser therapy on oral mucositis and quality of life in patients undergoing hematopoietic stem cell transplantation using the oral health impact profile and the functional assessment of cancer therapy-bone marrow transplantation questionnaires. Photomed Laser Surg 33(7):357–363. https://doi.org/10.1089/pho.2015.3911
Schubert MM, Williams BE, Lloid ME, Donaldson G, Chapko MK (1992) Clinical assessment scale for the rating of oral mucosal changes associated with bone marrow transplantation. Development of an oral mucositis index. Cancer 69(10):2469–77. https://doi.org/10.1002/1097-0142(19920515)69:10%3c2469::aid-cncr2820691015%3e3.0.co;2-w
Oberoi S, Zamperlini-Netto G, Beyene J, Treister NS, Sung L (2014) Effect of prophylactic low level laser therapy on oral mucositis: a systematic review and meta-analysis. PLoS One 9(9):e107418. https://doi.org/10.1371/journal.pone.0107418
Ferreira B, da Motta Silveira FM, de Orange FA (2016) Low-level laser therapy prevents severe oral mucositis in patients submitted to hematopoietic stem cell transplantation: a randomized clinical trial. Support Care Cancer 24(3):1035–1042. https://doi.org/10.1007/s00520-015-2881-8
Peralta-Mamani M, da Silva BM, da Silva Pinto AC, Rubira-Bullen IRF, Honório HM, Rubira CMF, da Silva Santos OS (2019) Low-level laser therapy dosimetry most used for oral mucositis due to radiotherapy for head and neck cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol 138:14–23. https://doi.org/10.1016/j.critrevonc.2019.03.009
Cavalcanti T, Almeida-Barros R, Catão M, Feitosa A, Lins R (2011) Conhecimento das propriedades físicas e da interação do laser com os tecidos biológicos na odontologia. Anais Bras Dermat. 86(5):955–960. https://doi.org/10.1590/S0365-05962011000500014
Wardley AM, Jayson GC, Swindell R, Morgenstern GR, Chang J, Bloor R, Fraser CJ, Scarffe JH (2000) Prospective evaluation of oral mucositis in patients receiving myeloablative conditioning regimens and haemopoietic progenitor rescue. Br J Haematol 110(2):292–299. https://doi.org/10.1046/j.1365-2141.2000.02202.x
Jewkes R, Gibbs A, Chirwa E, Dunkle K (2020) What can we learn from studying control arms of randomised VAW prevention intervention evaluations: reflections on expected measurement error, meaningful change and the utility of RCTs. Glob Health Action 13(1):1748401. https://doi.org/10.1080/16549716.2020.1748401
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2021) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane. https://training.cochrane.org/handbook. Accessed Feb 2021
Elad S, Arany P, Bensadoun RJ, Epstein JB, Barasch A, Raber-Durlacher J (2018) Photobiomodulation therapy in the management of oral mucositis: search for the optimal clinical treatment parameters. Support Care Cancer 26(10):3319–3321. https://doi.org/10.1007/s00520-018-4262-6
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), through the postgraduate program in stomatology at the University Federal of Paraná.
Author information
Authors and Affiliations
Contributions
Conceptualization, BMS1; methodology, BMS1; MLP; LRG; validation, MRA; formal analysis, MRA and JMA.; resources, BMS1; MLP; LRG and BMS2; writing, BMS1; MLP; LRG, BMS2; review and editing, MRA, JMA, and BMS1. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
da Silva, B.M., Prosdócimo, M.L., Gasparini, L.R. et al. Most used photobiomodulation dosimetry parameters to treat oral mucositis after preconditioning for hematopoietic stem cell transplantation: systematic review and meta-analysis. Support Care Cancer 30, 3721–3732 (2022). https://doi.org/10.1007/s00520-022-06817-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06817-w