Abstract
Introduction
Endoluminal functional lumen imaging probe (EndoFLIP) provides a real-time assessment of gastroesophageal junction (GEJ) compliance during fundoplication. Given the limited data on EndoFLIP measurements during the Hill procedure, we investigated the impact of the Hill procedure on GEJ compliance compared to Toupet fundoplication.
Methods
Patients who underwent robotic Hill or Toupet fundoplication with intraoperative EndoFLIP between 2017 and 2022 were included. EndoFLIP measurements of the GEJ included cross sectional surface area (CSA), intra-balloon pressure, high pressure zone length (HPZ), distensibility index (DI), and compliance. Subjective reflux symptoms, gastroesophageal reflux disease-health related quality of life (GERD-HRQL) score, and dysphagia score were assessed pre-operatively as well as at short- and longer-term follow-up.
Results
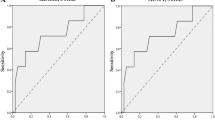
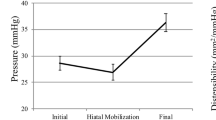
One-hundred and fifty-four patients (71.9%) had a Toupet fundoplication while sixty (28%) patients underwent the Hill procedure. The CSA [27.7 ± 10.9 mm2 vs 42.2 ± 17.8 mm2, p < 0.0001], pressure [29.5 ± 6.2 mmHg vs 33.9 ± 8.5 mmHg, p = 0.0009], DI [0.9 ± 0.4 mm2/mmHg vs 1.3 ± 0.6 mm2/mmHg, p = 0.001], and compliance [25.9 ± 12.8 mm3/mmHg vs 35.4 ± 13.4 mm3/mmHg, p = 0.01] were lower after the Hill procedure compared to Toupet. However, there was no difference in post-fundoplication HPZ between procedures [Hill: 2.9 ± 0.4 cm, Toupet: 3.1 ± 0.6 cm, p = 0.15]. Follow-up showed no significant differences in GERD-HRQL scores, overall dysphagia scores or atypical symptoms between groups (p > 0.05).
Conclusion
The Hill procedure is as effective to the Toupet fundoplication in surgically treating gastroesophageal reflux disease (GERD) despite the lower CSA, DI, and compliance after the Hill procedure. Both procedures led to DI < 2 mm2/mmHg with no significant differences in dysphagia reporting (12–24) months after the procedure. Further studies to elucidate a cutoff value for DI for postoperative dysphagia development are still warranted.

Similar content being viewed by others
References
Park Y et al (2018) Laparoscopic Hill repair: 25-year follow-up. Surg Endosc 32(10):4111–4115
Kraemer SJ et al (1994) Laparoscopic Hill repair. Gastrointest Endosc 40(2):155–159
Aye RW et al (2011) The Hill antireflux repair at 5 institutions over 25 years. Am J Surg 201(5):599–604
Aye RW et al (2012) A randomized multiinstitution comparison of the laparoscopic Nissen and Hill repairs. Ann Thorac Surg 94(3):951–958
Aye RW et al (1994) Early results with the laparoscopic Hill repair. Am J Surg 167(5):542–546
Low D (1995) Hill antireflux operation. Chest Surg Clin N Am 5(3):411–422
Hermreck AS, Coates NR (1980) Results of the Hill antireflux operation. Am J Surg 140(6):764–767
Broeders J et al (2010) Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg 97(9):1318–1330
Broeders JA et al (2013) Laparoscopic anterior 180-degree versus nissen fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis of randomized clinical trials. Ann Surg 257(5):850–859
Varin O et al (2009) Total vs partial fundoplication in the treatment of gastroesophageal reflux disease: a meta-analysis. Arch Surg 144(3):273–278
Turner B et al (2020) Is that “floppy” fundoplication tight enough? Surg Endosc 34(4):1823–1828
Donnan EN, Pandolfino JE (2020) EndoFLIP in the esophagus: assessing sphincter function, wall stiffness, and motility to guide treatment. Gastroenterol Clin North Am 49(3):427–435
Kwiatek MA et al (2010) Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg 14:268–276
Lee JM et al (2021) The usefulness of the measurement of esophagogastric junction distensibility by EndoFLIP in the diagnosis of gastroesophageal reflux disease. Gut Liver 15(4):546–552
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28(3):178–182
Su B et al (2020) Using impedance planimetry (EndoFLIP™) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc 34(4):1761–1768
Wu H et al (2022) Impedance planimetry (EndoFLIP™) reveals changes in gastroesophageal junction compliance during fundoplication. Surg Endosc 36(9):6801–6808
Stefanova DI et al (2020) Quantifying factors essential to the integrity of the esophagogastric junction during antireflux procedures. Ann Surg 272(3):488–494
Greenberg JA et al (2022) Quantifying physiologic parameters of the gastroesophageal junction during re-operative anti-reflux surgery. Surg Endosc 36(9):7008–7015
Liu M et al (2022) The impact of pneumoperitoneum on esophagogastric junction distensibility during anti-reflux surgery. Surg Endosc 36(1):367–374
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976) 27(22):2453–2458
Bramhall SR, Mourad MM (2019) Wrap choice during fundoplication. World J Gastroenterol 25(48):6876
DeMeester SR (2020) Laparoscopic hernia repair and fundoplication for gastroesophageal reflux disease. Gastrointest Endosc Clin N Am 30(2):309–324
Zornig C et al (2002) Nissen vs Toupet laparoscopic fundoplication: a prospective randomized study of 200 patients with and without preoperative esophageal motility disorders. Surg Endosc 16:758–766
McKernan J (1994) Laparoscopic repair of gastroesophageal reflux disease: Toupet partial fundoplication versus Nissen fundoplication. Surg Endosc 8:851–856
Shah A et al (2022) A novel EndoFLIP marker during hiatal hernia repair is associated with short-term postoperative dysphagia. Surg Endosc 9:1–7
Wu H et al (2022) Impedance planimetry (Endoflip) and Ideal distensibility ranges for optimal outcomes after nissen and toupet fundoplication. J Am Coll Surg 235(3):420–429
Ilczyszyn A, Botha A (2014) Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus 27(7):637–644
Nwokedi U et al (2021) Short-term outcome of routine use of EndoFLIP during hiatal hernia repair. Surg Endosc 35:3840–3849
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Rasa Zarnegar works as a consultant for Bard (BD) and Intuitive/Medtronic. Drs. Hala Al Asadi, Haythem Najah, Rodrigo Edelmuth, Jacques A. Greenberg, Teagan Marshall, Niloufar Salehi, Yeon Joo Lee, Maria Cristina Riascos, Brendan M. Finnerty, Thomas J. Fahey III have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al Asadi, H., Najah, H., Edelmuth, R. et al. Impedance planimetry (EndoFLIPTM) and surgical outcomes after Hill compared to Toupet fundoplication. Surg Endosc 38, 1020–1028 (2024). https://doi.org/10.1007/s00464-023-10640-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10640-7