Abstract
Background
Laparoscopic adrenalectomy (LA) is the gold standard treatment for unilateral primary aldosteronism. However, satisfactory results have also been published with radiofrequency ablation (RFA). The aim of this study was to compare LA and RFA for the treatment of primary aldosteronism.
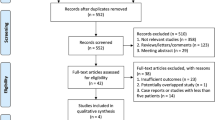
Methods
A retrospective cohort study of the patients who underwent LA or RFA in a single center was performed. Morbidity and long-term effectiveness (cure rate and blood pressure control) were analyzed. A multivariate analysis with a propensity score was also performed.
Results
Thirty-four patients were included in the study, 24 in the LA group and 10 in the RFA group. Hypertension had been diagnosed a median of 12 years before the intervention. Hypertension was properly controlled before the intervention in 55.9% of the patients. Hypertensive crisis was more common during RFA (4.2% vs. 70.0%, p < 0.001), although no patient suffered any complication because of these crises. LA was longer (174.6 vs. 105.5 min, p = 0.001) and had a longer length of stay (median 2 vs 1 days, p < 0.001). No severe complications were observed in any of the patients. After a median follow-up of 46.2 months, more patients had hypertension cured and blood pressure controlled in the LA group (29.2% vs. 0%, p = 0.078 and 95.5% vs. 50.0%, p = 0.006, respectively). Also, patients in the LA group were taking less antihypertensive drugs (1.8 vs. 3.0, p = 0.054) or mineralocorticoid receptor antagonists (41.7% vs. 90.0%, p = 0.020). Multivariate analysis adjusted by propensity score showed that LA had an OR = 11.3 (p = 0.138) for hypertension cure and an OR = 55.1 (p = 0.040) for blood pressure control.
Conclusions
Although RFA was a less invasive procedure than LA, hypertension was cured and blood pressure was properly controlled in more patients from the LA group. Patients who underwent LA were taking less antihypertensive drugs than patients who had undergone RFA.


Similar content being viewed by others
References
Conn JW (1955) Presidential address I. Painting background. II. Primary aldosteronism, a new clinical syndrome. J Lab Clin Med 45:3–17
Conn JW, Louis LH (1956) Primary aldosteronism, a new clinical entity. Ann Intern Med 44:1–15
Gagner M, Lacroix A, Bolte E (1992) Laparoscopic adrenalectomy in cushing’s syndrome and pheochromocytoma. N Engl J Med 327:1033
McManus C, Kuo JH (2020) Surgical approach to patients with primary aldosteronism. Gland Surg 9:25–31
Funder JW, Carey RM, Mantero F, et al. 2016 The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 101(5): 1889–1916
Kigure T, Harada T, Satoh Y, Fujieda N, Wakayama Y (1996) Microwave ablation of the adrenal gland: experimental study and clinical application. Br J Urol 77:215–220
Liu SY, Chu CC, Tsui TK et al (2016) Aldosterone-producing adenoma in primary aldosteronism: CT-guided radiofrequency ablation-long-term results and recurrence rate. Radiology 281:625–634
Liu SY, Chu CM, Kong AP et al (2016) Radiofrequency ablation compared with laparoscopic adrenalectomy for aldosterone-producing adenoma. Br J Surg 103:1476–1486
Sarwar A, Brook OR, Vaidya A et al (2016) Clinical outcomes following percutaneous radiofrequency ablation of unilateral aldosterone-producing adenoma: comparison with adrenalectomy. J Vasc Interv Radiol 27:961–967
Yang MH, Tyan YS, Huang YH, Wang SC, Chen SL (2016) Comparison of radiofrequency ablation versus laparoscopic adrenalectomy for benign aldosterone-producing adenoma. Radiol Med 121:811–819
Yang R, Xu L, Lian H, Gan W, Guo H (2014) Retroperitoneoscopic-guided cool-tip radiofrequency ablation of adrenocortical aldosteronoma. J Endourol 28:1208–1214
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Shimamoto K, Fujita T, Ito S et al (2008) Impact of blood pressure control on cardiovascular events in 26,512 Japanese hypertensive patients: the Japan hypertension evaluation with angiotensin II antagonist losartan therapy (J-HEALTH) study, a prospective nationwide observational study. Hypertens Res 31:469–478
Control hypertension to prevent cardiovascular complications (2007) 24/7 blood pressure control helps reduce stroke risk, especially during the early morning hours, when the incidence is greatest. Heart Advis 10:4–5
Gaciong Z, Sinski M, Lewandowski J (2013) Blood pressure control and primary prevention of stroke: summary of the recent clinical trial data and meta-analyses. Curr Hypertens Rep 15:559–574
Kjeldsen SE, Narkiewicz K, Burnier M, Oparil S (2019) Systolic blood pressure control prevents cognitive decline and slows development of white matter lesions in the brain: the SPRINT MIND study outcomes. Blood Press 28:356–357
Yamazaki Y, Nakamura Y, Omata K et al (2017) Histopathological classification of cross-sectional image-negative hyperaldosteronism. J Clin Endocrinol Metab 102:1182–1192
Volpe C, Hamberger B, Hoog A et al (2015) Primary aldosteronism: functional histopathology and long-term follow-up after unilateral adrenalectomy. Clin Endocrinol 82:639–647
Nanba AT, Nanba K, Byrd JB et al (2017) Discordance between imaging and immunohistochemistry in unilateral primary aldosteronism. Clin Endocrinol 87:665–672
Williams TA, Gómez-Sánchez CE, Rainey WE et al (2021) International histopathology consensus for unilateral primary aldosteronism. J Clin Endocrinol Metab 106:42–54
Liang KW, Jahangiri Y, Tsao TF, Tyan YS, Huang HH (2019) Effectiveness of thermal ablation for aldosterone-producing adrenal adenoma: a systematic review and meta-analysis of clinical and biochemical parameters. J Vasc Interv Radiol 30:1335–1342
Jaffe G, Gray Z, Krishnan G et al (2020) Screening rates for primary aldosteronism in resistant hypertension: a cohort study. Hypertension 75:650–659
Vorselaars W, van Beek DJ, Suurd DPD et al (2020) Adrenalectomy for primary aldosteronism: significant variability in work-up strategies and low guideline adherence in worldwide daily clinical practice. World J Surg 44:1905–1915
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Oscar Cano-Valderrama, Jimena González-Nieto, María Abad-Cardiel, Santiago Ochagavía, Isabelle Rünkle, José V. Méndez, José A. García-Donaire, Martín Cuesta-Hernández, Javier E. Armijo, Paz Miguel-Novoa, Antonio J. Torres and Nieves Martell-Claros have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cano-Valderrama, O., González-Nieto, J., Abad-Cardiel, M. et al. Laparoscopic adrenalectomy vs. radiofrequency ablation for the treatment of primary aldosteronism. A single center retrospective cohort analysis adjusted with propensity score. Surg Endosc 36, 1970–1978 (2022). https://doi.org/10.1007/s00464-021-08481-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08481-3