Abstract
Background
Laparoscopy provides a minimally invasive alternative to open abdominal surgery. Current data describing its association with hospital readmission and costs in relation to surgeon laparoscopic case volume is limited to smaller databases and subsets of operations.
Methods
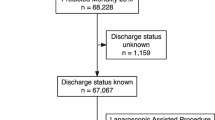
This retrospective cohort study of 23,285 adult abdominal operations from 2007 to 2015 compares 30-day readmission rate and costs between laparoscopic and open abdominal operations and examines effect modification by surgeon laparoscopic case volume. Outcomes were all-cause hospital readmission within 30 days after discharge and index hospital admission cost.
Results
All-cause hospital readmission rates were significantly lower after laparoscopic abdominal operations compared with open operations (adjusted odds ratio [aOR] 0.56, 95% CI 0.46–0.69, p < 0.001) with a difference in readmission risk attributable to laparoscopic approach of − 4.0% (95% CI − 5.4 to − 2.6%) in complete-case analysis. Among surgeons with a high laparoscopic case volume, the estimated difference in readmission risk through laparoscopy was magnified (− 5.8%, 95% CI − 7.5 to − 4.1%) compared to low surgeon laparoscopic case volume (− 2.9%, 95% CI − 4.8 to −1.1%, p for interaction = 0.005). The estimated difference in costs of the index hospital admission attributable to laparoscopic approach was − $3869 (95% CI − $4200 to − $3538; adjusted incidence rate ratio 0.77, 95% CI 0.75–0.79, p < 0.001). Laparoscopy was followed by significantly lower rates of readmissions related to gastrointestinal (aOR 0.68, 95% CI 0.55–0.85, p = 0.001), wound complications (infection: aOR 0.33, 95% CI 0.23–0.47, p < 0.001; non-infectious: aOR 0.47, 95% CI 0.30–0.74, p = 0.001), and malignancy (aOR 0.68, 95% CI 0.55–0.85, p < 0.001). The findings remain robust after multiple imputation and sensitivity analyses.
Conclusions
Laparoscopy versus open abdominal surgery is associated with reduced hospital readmissions related to malignancy, gastrointestinal, and wound complications. Effect modification by higher laparoscopy case volume argues for continued proliferation of laparoscopy in abdominal surgeries.


Similar content being viewed by others
References
Weller WE, Rosati C (2008) Comparing outcomes of laparoscopic versus open bariatric surgery. Ann Surg 248:10–15. https://doi.org/10.1097/SLA.0b013e31816d953a
Jennings AJ, Spencer RJ, Medlin E, Rice LW, Uppal S (2015) Predictors of 30-day readmission and impact of same-day discharge in laparoscopic hysterectomy. Am J Obstet Gynecol 213:344.e1–344.e7. https://doi.org/10.1016/j.ajog.2015.05.014
Guller U, Jain N, Hervey S, Purves H, Pietrobon R (2003) Laparoscopic vs open colectomy: outcomes comparison based on large nationwide databases. Arch Surg Chic Ill 138:1179–1186. https://doi.org/10.1001/archsurg.138.11.1179
Fuks D, Cauchy F, Ftériche S, Nomi T, Schwarz L, Dokmak S, Scatton O, Fusco G, Belghiti J, Gayet B, Soubrane O (2016) Laparoscopy decreases pulmonary complications in patients undergoing major liver resection: a propensity score analysis. Ann Surg 263:353–361. https://doi.org/10.1097/SLA.0000000000001140
Karayiannakis AJ, Makri GG, Mantzioka A, Karousos D, Karatzas G (1996) Postoperative pulmonary function after laparoscopic and open cholecystectomy. Br J Anaesth 77:448–452
Brenkman HJF, Gisbertz SS, Slaman AE, Goense L, Ruurda JP, van Berge Henegouwen MI, van Hillegersberg R, Dutch Upper Gastrointestinal Cancer Audit (DUCA) group (2017) Postoperative outcomes of minimally invasive gastrectomy versus open gastrectomy during the early introduction of minimally invasive gastrectomy in the Netherlands: a population-based cohort study. Ann Surg 266:831–838. https://doi.org/10.1097/SLA.0000000000002391
Bardakcioglu O, Khan A, Aldridge C, Chen J (2013) Growth of laparoscopic colectomy in the United States: analysis of regional and socioeconomic factors over time. Ann Surg 258:270–274. https://doi.org/10.1097/SLA.0b013e31828faa66
Yamada T, Okabayashi K, Hasegawa H, Tsuruta M, Yoo J-H, Seishima R, Kitagawa Y (2016) Meta-analysis of the risk of small bowel obstruction following open or laparoscopic colorectal surgery. Br J Surg 103:493–503. https://doi.org/10.1002/bjs.10105
Sharma KC, Brandstetter RD, Brensilver JM, Jung LD (1996) Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest 110:810–815
Keller DS, Lawrence JK, Nobel T, Delaney CP (2013) Optimizing cost and short-term outcomes for elderly patients in laparoscopic colonic surgery. Surg Endosc 27:4463–4468. https://doi.org/10.1007/s00464-013-3088-z
Dowson HM, Gage H, Jackson D, Qiao Y, Williams P, Rockall TA (2012) Laparoscopic and open colorectal surgery: a prospective cost analysis. Colorectal Dis Off J Assoc Coloproctology G B Irel 14:1424–1430. https://doi.org/10.1111/j.1463-1318.2012.02988.x
Zhuang C-L, Huang D-D, Chen F-F, Zhou C-J, Zheng B-S, Chen B-C, Shen X, Yu Z (2015) Laparoscopic versus open colorectal surgery within enhanced recovery after surgery programs: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc 29:2091–2100. https://doi.org/10.1007/s00464-014-3922-y
Hardy KM, Kwong J, Pitzul KB, Vergis AS, Jackson TD, Urbach DR, Okrainec A (2014) A cost comparison of laparoscopic and open colon surgery in a publicly funded academic institution. Surg Endosc 28:1213–1222. https://doi.org/10.1007/s00464-013-3311-y
Halawani HM, Tamim H, Khalifeh F, Mailhac A, Taher A, Hoballah J, Jamali FR (2017) Outcomes of laparoscopic vs open common bile duct exploration: analysis of the NSQIP database. J Am Coll Surg 224:833.e2–840.e2. https://doi.org/10.1016/j.jamcollsurg.2017.01.062
Davenport DL, Ueland WR, Kumar S, Plymale M, Bernard AC, Roth JS (2019) A comparison of short-term outcomes between laparoscopic and open emergent repair of perforated peptic ulcers. Surg Endosc 33:764–772. https://doi.org/10.1007/s00464-018-6341-7
Naffouje SA, Salloum RH, Khalaf Z, Salti GI (2019) Outcomes of open versus minimally invasive ivor-lewis esophagectomy for cancer: a propensity-score matched analysis of NSQIP database. Ann Surg Oncol 26:2001–2010. https://doi.org/10.1245/s10434-019-07319-6
Gani F, Cerullo M, Zhang X, Canner JK, Conca-Cheng A, Hartzman AE, Husain SG, Cirocco WC, Traugott AL, Arnold MW, Johnston FM, Pawlik TM (2017) Effect of surgeon “experience” with laparoscopy on postoperative outcomes after colorectal surgery. Surgery 162:880–890. https://doi.org/10.1016/j.surg.2017.06.018
Singla A, Li Y, Ng SC, Csikesz NG, Tseng JF, Shah SA (2009) Is the growth in laparoscopic surgery reproducible with more complex procedures? Surgery 146:367–374. https://doi.org/10.1016/j.surg.2009.06.006
Khorgami Z, Andalib A, Aminian A, Kroh MD, Schauer PR, Brethauer SA (2016) Predictors of readmission after laparoscopic gastric bypass and sleeve gastrectomy: a comparative analysis of ACS-NSQIP database. Surg Endosc 30:2342–2350. https://doi.org/10.1007/s00464-015-4477-2
Abraham CR, Werter CR, Ata A, Hazimeh YM, Shah US, Bhakta A, Tafen M, Singh PT, Beyer TD, Stain SC (2015) Predictors of hospital readmission after bariatric surgery. J Am Coll Surg 221:220–227. https://doi.org/10.1016/j.jamcollsurg.2015.02.018
Tevis SE, Weber SM, Kent KC, Kennedy GD (2015) Nomogram to predict postoperative readmission in patients who undergo general surgery. JAMA Surg 150:505–510. https://doi.org/10.1001/jamasurg.2014.4043
Raakow J, Schulte-Mäter J, Callister Y, Aydin M, Denecke C, Pratschke J, Kilian M (2018) A comparison of laparoscopic and open repair of subxiphoid incisional hernias. Hernia J Hernias Abdom Wall Surg 22:1083–1088. https://doi.org/10.1007/s10029-018-1815-z
Friedrich S, Raub D, Teja BJ, Neves SE, Thevathasan T, Houle TT, Eikermann M (2019) Effects of low-dose intraoperative fentanyl on postoperative respiratory complication rate: a pre-specified, retrospective analysis. Br J Anaesth 122:e180–e188. https://doi.org/10.1016/j.bja.2019.03.017
Ng PY, Ng AK-Y, Subramaniam B, Burns SM, Herisson F, Timm FP, Rudolph MI, Scheffenbichler F, Friedrich S, Houle TT, Bhatt DL, Eikermann M (2018) Association of preoperatively diagnosed patent foramen ovale with perioperative ischemic stroke. JAMA 319:452. https://doi.org/10.1001/jama.2017.21899
Grabitz SD, Rajaratnam N, Chhagani K, Thevathasan T, Teja BJ, Deng H, Eikermann M, Kelly BJ (2019) The effects of postoperative residual neuromuscular blockade on hospital costs and intensive care unit admission: a population-based cohort study. Anesth Analg 128:1129–1136. https://doi.org/10.1213/ANE.0000000000004028
Sheetz KH, Norton EC, Birkmeyer JD, Dimick JB (2017) Provider experience and the comparative safety of laparoscopic and open colectomy. Health Serv Res 52:56–73. https://doi.org/10.1111/1475-6773.12482
Sheetz KH, Ibrahim AM, Regenbogen SE, Dimick JB (2017) Surgeon experience and medicare expenditures for laparoscopic compared to open colectomy. Ann Surg. https://doi.org/10.1097/sla.0000000000002312
Long DR, Lihn AL, Friedrich S, Scheffenbichler FT, Safavi KC, Burns SM, Schneider JC, Grabitz SD, Houle TT, Eikermann M (2018) Association between intraoperative opioid administration and 30-day readmission: a pre-specified analysis of registry data from a healthcare network in New England. Br J Anaesth 120:1090–1102. https://doi.org/10.1016/j.bja.2017.12.044
Canet J, Gallart L, Gomar C, Paluzie G, Vallès J, Castillo J, Sabaté S, Mazo V, Briones Z, Sanchis J, ARISCAT Group (2010) Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 113:1338–1350. https://doi.org/10.1097/aln.0b013e3181fc6e0a
Thevathasan T, Shih SL, Safavi KC, Berger DL, Burns SM, Grabitz SD, Glidden RS, Zafonte RD, Eikermann M, Schneider JC (2017) Association between intraoperative non-depolarising neuromuscular blocking agent dose and 30-day readmission after abdominal surgery. Br J Anaesth 119:595–605. https://doi.org/10.1093/bja/aex240
Donzé J, Aujesky D, Williams D, Schnipper JL (2013) Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model. JAMA Intern Med 173:632–638. https://doi.org/10.1001/jamainternmed.2013.3023
Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, Tsai TC, Ko CY, Bilimoria KY (2015) Underlying reasons associated with hospital readmission following surgery in the United States. JAMA 313:483–495. https://doi.org/10.1001/jama.2014.18614
Fisher AV, Fernandes-Taylor S, Schumacher JR, Havlena JA, Wang X, Lawson EH, Ronnekleiv-Kelly SM, Winslow ER, Weber SM, Abbott DE (2018) Analysis of 90-day cost for open versus minimally invasive distal pancreatectomy. HPB. https://doi.org/10.1016/j.hpb.2018.07.003
Shin CH, Long DR, McLean D, Grabitz SD, Ladha K, Timm FP, Thevathasan T, Pieretti A, Ferrone C, Hoeft A, Scheeren TWL, Thompson BT, Kurth T, Eikermann M (2018) Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg 267:1084–1092. https://doi.org/10.1097/SLA.0000000000002220
POISE Study Group, Devereaux PJ, Yang H, Yusuf S, Guyatt G, Leslie K, Villar JC, Xavier D, Chrolavicius S, Greenspan L, Pogue J, Pais P, Liu L, Xu S, Málaga G, Avezum A, Chan M, Montori VM, Jacka M, Choi P (2008) Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet Lond Engl 371:1839–1847. https://doi.org/10.1016/s0140-6736(08)60601-7
Mascha EJ, Yang D, Weiss S, Sessler DI (2015) Intraoperative mean arterial pressure variability and 30-day mortality in patients having noncardiac surgery. Anesthesiology 123:79–91. https://doi.org/10.1097/ALN.0000000000000686
Saravanan S, Kocarev M, Wilson RC, Watkins E, Columb MO, Lyons G (2006) Equivalent dose of ephedrine and phenylephrine in the prevention of post-spinal hypotension in Caesarean section. Br J Anaesth 96:95–99. https://doi.org/10.1093/bja/aei265
Lukannek C, Shaefi S, Platzbecker K, Raub D, Santer P, Nabel S, Lecamwasam HS, Houle TT, Eikermann M (2019) The development and validation of the Score for the Prediction of Postoperative Respiratory Complications (SPORC-2) to predict the requirement for early postoperative tracheal re-intubation: a hospital registry study. Anaesthesia 74:1165–1174. https://doi.org/10.1111/anae.14742
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Grabitz SD, Farhan HN, Ruscic KJ, Timm FP, Shin CH, Thevathasan T, Staehr-Rye AK, Kurth T, Eikermann M (2017) Dose-dependent protective effect of inhalational anesthetics against postoperative respiratory complications: a prospective analysis of data on file from three hospitals in New England. Crit Care Med 45:e30–e39. https://doi.org/10.1097/CCM.0000000000002015
Shin CH, Grabitz SD, Timm FP, Mueller N, Chhangani K, Ladha K, Devine S, Kurth T, Eikermann M (2017) Development and validation of a Score for Preoperative Prediction of Obstructive Sleep Apnea (SPOSA) and its perioperative outcomes. BMC Anesthesiol 17:71. https://doi.org/10.1186/s12871-017-0361-z
Baltodano PA, Webb-Vargas Y, Soares KC, Hicks CW, Cooney CM, Cornell P, Burce KK, Pawlik TM, Eckhauser FE (2016) A validated, risk assessment tool for predicting readmission after open ventral hernia repair. Hernia 20:119–129. https://doi.org/10.1007/s10029-015-1413-2
Morris MS, Graham LA, Richman JS, Hollis RH, Jones CE, Wahl T, Itani KMF, Mull HJ, Rosen AK, Copeland L, Burns E, Telford G, Whittle J, Wilson M, Knight SJ, Hawn MT (2016) Postoperative 30-day readmission: time to focus on what happens outside the hospital. Ann Surg 264:621–631. https://doi.org/10.1097/SLA.0000000000001855
Sheetz KH, Norton EC, Regenbogen SE, Dimick JB (2017) An instrumental variable analysis comparing medicare expenditures for laparoscopic vs open colectomy. JAMA Surg 152:921–929. https://doi.org/10.1001/jamasurg.2017.1578
Delaney CP, Chang E, Senagore AJ, Broder M (2008) Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg 247:819–824. https://doi.org/10.1097/SLA.0b013e31816d950e
Koh FH, Tan KK, Tsang CB, Koh DC (2013) Laparoscopic versus an open colectomy in an emergency setting: a case-controlled study. Ann Coloproctol 29:12–16. https://doi.org/10.3393/ac.2013.29.1.12
Biondi A, Di Stefano C, Ferrara F, Bellia A, Vacante M, Piazza L (2016) Laparoscopic versus open appendectomy: a retrospective cohort study assessing outcomes and cost-effectiveness. World J Emerg Surg 11:44. https://doi.org/10.1186/s13017-016-0102-5
Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Cole CJ, Lee SJ, Wolfe BM (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234:279–289; discussion 289–291
Tiwari MM, Reynoso JF, High R, Tsang AW, Oleynikov D (2011) Safety, efficacy, and cost-effectiveness of common laparoscopic procedures. Surg Endosc 25:1127–1135. https://doi.org/10.1007/s00464-010-1328-z
Fitch K, Bochner A, Keller DS (2017) Cost comparison of laparoscopic colectomy versus open colectomy in colon cancer. Curr Med Res Opin 33:1215–1221. https://doi.org/10.1080/03007995.2017.1310719
Ielpo B, Nuñez-Alfonsel J, Duran H, Diaz E, Fabra I, Caruso R, Malavé L, Ferri V, Barzola E, Quijano Y, Vicente E (2018) Cost-effectiveness of randomized study of laparoscopic versus open bilateral inguinal hernia repair. Ann Surg 268:725. https://doi.org/10.1097/SLA.0000000000002894
Banki F, Weaver M, Roife D, Kaushik C, Khanna A, Ochoa K, Miller CC (2017) Laparoscopic reoperative antireflux surgery is more cost-effective than open approach. J Am Coll Surg 225:235–242. https://doi.org/10.1016/j.jamcollsurg.2017.03.019
Franks PJ, Bosanquet N, Thorpe H, Brown JM, Copeland J, Smith AM, Quirke P, Guillou PJ (2006) Short-term costs of conventional vs laparoscopic assisted surgery in patients with colorectal cancer (MRC CLASICC trial). Br J Cancer 95:6–12. https://doi.org/10.1038/sj.bjc.6603203
Yasunaga H, Horiguchi H, Kuwabara K, Matsuda S, Fushimi K, Hashimoto H, Ayanian JZ (2013) Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann Surg 257:640–646. https://doi.org/10.1097/SLA.0b013e31826fd541
Chen K, Zhang Z, Zuo Y, Ren S (2014) Comparison of the clinical outcomes of laparoscopic-assisted versus open surgery for colorectal cancer. Oncol Lett 7:1213–1218. https://doi.org/10.3892/ol.2014.1859
Janson M, Björholt I, Carlsson P, Haglind E, Henriksson M, Lindholm E, Anderberg B (2004) Randomized clinical trial of the costs of open and laparoscopic surgery for colonic cancer. Br J Surg 91:409–417. https://doi.org/10.1002/bjs.4469
Hara T, Fujiwara Y, Sugimura K, Kishi K, Motoori M, Miyoshi N, Akita H, Gotoh K, Takahashi H, Marubashi S, Noura S, Ohue M, Sakon M, Yano M (2014) Comparison of early clinical outcomes between laparoscopic total gastrectomy and open total gastrectomy for early-stage gastric cancer. Gan Kagaku Ryoho 41:1476–1478
Liao CH, Tan EC, Chen CC, Yang MC (2017) Real-world cost-effectiveness of laparoscopy versus open colectomy for colon cancer: a nationwide population-based study. Surg Endosc 31:1796–1805. https://doi.org/10.1007/s00464-016-5176-3
Sood A, Meyer CP, Abdollah F, Sammon JD, Sun M, Lipsitz SR, Hollis M, Weissman JS, Menon M, Trinh Q-D (2017) Minimally invasive surgery and its impact on 30-day postoperative complications, unplanned readmissions and mortality. Br J Surg 104:1372–1381. https://doi.org/10.1002/bjs.10561
Jaschinski T, Mosch CG, Eikermann M, Neugebauer EA, Sauerland S (2018) Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 11:CD001546. https://doi.org/10.1002/14651858.cd001546.pub4
Cirocchi R, Cesare Campanile F, Di Saverio S, Popivanov G, Carlini L, Pironi D, Tabola R, Vettoretto N (2017) Laparoscopic versus open colectomy for obstructing right colon cancer: a systematic review and meta-analysis. J Visc Surg 154:387–399. https://doi.org/10.1016/j.jviscsurg.2017.09.002
Lujan J, Valero G, Hernandez Q, Sanchez A, Frutos MD, Parrilla P (2009) Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg 96:982–989. https://doi.org/10.1002/bjs.6662
Acknowledgments
The authors would like to acknowledge Dr. Christina H. Shin and Sara M. Burns for assistance with statistical analyses and scientific discourse.
Funding
This work was supported by Jeffrey and Judith Buzen in an unrestricted grant (philanthropic donation) to Matthias Eikermann.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
This work was supported by Jeffrey and Judith Buzen in an unrestricted grant to Matthias Eikermann. The funders had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. Dr. T. Houle reports grants from NINDS (PI), grants from NIGMS, personal fees from Headache, personal fees from Anesthesiology, personal fees from Cephalalgia, outside the submitted work. Dr. E. Eikermann received funding for investigator-initiated trials from Merck, and received honorarium for giving advice to Merck, he holds equity of Calabash Bioscience Inc., and is an Associate Editor of the British Journal of Anaesthesia. Drs. T. Shin, G. Brat, V. Sein, R. Munoz-Acuna, and C. Ferrone as well as Ms. S. Friedrich and M. Rudolph have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shin, T.H., Friedrich, S., Brat, G.A. et al. Effects of laparoscopic vs open abdominal surgery on costs and hospital readmission rate and its effect modification by surgeons’ case volume. Surg Endosc 34, 1–12 (2020). https://doi.org/10.1007/s00464-019-07222-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07222-x