Abstract
An 82-year-old woman presented with abdominal pain, nausea, emesis, and weight loss of ~25 lb over 6 months. A CT scan and MRI of the abdomen revealed a mass in the tail of the pancreas that was suspicious for malignancy. The patient underwent successful laparoscopic distal pancreatectomy and was discharged home on the 4th postoperative day after an uneventful course. Pathology revealed an inflammatory pseudotumor of the pancreas (IPT). Pancreatic IPT is a rare entity, and this case represents the first report of laparoscopic resection of this lesion. The presentation, diagnosis, histologic features, and therapy of IPT of the pancreas are reviewed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inflammatory pseudotumors (ITP) are rare nonencapsulated solid tumorlike lesions of unclear etiology that can be found in multiple organ systems. The lesions are comprised of aggregations of inflammatory cells surrounded by a proliferative fibrous stroma and are generally considered benign in nature. However, the constellation of presenting symptoms and the radiographic appearance of ITP of the pancreas are often consistent with a pancreatic malignancy, and operative resection of these lesions is necessary to rule out a malignant process. We present the case of an 82-year-old woman who to our knowledge is the first reported case of pancreatic IPT treated laparoscopically.
Case report
An 82-year-old woman with a medical history of non–insulin-dependent diabetes and hypertension presented with a 2-month history of intermittent nausea and vomiting after meals and postprandial abdominal pain. The patient had sustained a 25-lb weight loss and systemic complaints of generalized fatigue over the preceding 6 months. The patient denied alcohol or tobacco use and stated no risk factors for pancreatitis.
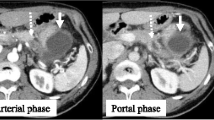
Physical exam revealed a thin but well-appearing elderly woman with a soft abdomen and no palpable abdominal masses and adenopathy. Laboratory examination—including complete blood count, amylase, lipase, liver function tests, and triglycerides—revealed no significant abnormalities. Abdominal ultrasound showed no evidence of biliary disease. Esophagogastroduodenoscopy, colonoscopy, and gastric emptying studies demonstrated only diverticulosis and evidence of gastroparesis. A CT scan of the abdomen and pelvis revealed an irregularity in the tail of the pancreas consistent with a pancreatic neoplasm, but there was no evidence of pancreatitis, pancreatic duct dilation, adenopathy, or metastatic disease. An MRI confirmed the presence of a 2.5 × 1.9 cm mass located in the pancreatic tail (Fig. 1). The lesion appeared to be confined to pancreatic parenchyma and was not associated with evidence of metastasis.
Because of the concern regarding malignancy, the patient was brought to the operating room for laparoscopic distal pancreatectomy and splenectomy, which proceeded without complications. At exploration, a solid, nonencapsulated lesion confined to the parenchyma of the tail of the pancreas was discovered (Fig. 2). No evidence of metastatic disease was present. Complete mobilization and resection of the spleen and pancreatic tail en bloc was performed laparoscopically. A Harmonic Scalpel was used for dissection and an endo-GIA stapler with 2.5-mm staples for dividing the pancreas. The specimen was removed from the abdomen via a small upper midline incision and a wound protection device.
On intraoperative frozen sections of the tumor, we were unable to differentiate between low-grade carcinoma and chronic pancreatitis. However, permanent histology revealed that the lesion was a benign inflammatory pseudotumor with chronic fibrosing pancreatitis (Fig. 3).
A Low-power view of the fibrotic pancreas showing dense fibrosis and lymphoid follicles scattered throughout the lesion. B Paucicellular fibrotic process composed of interlacing bands of myofibroblasts centered on blood vessel walls with a dense inflammatory infiltrate of lymphocytes and plasma cells (×100)
The patient underwent an uneventful recovery and was discharged home on the 4th postoperative day. At 12-month follow-up, the patient had achieved stabilization of her weight and complete resolution of her abdominal symptoms. She remains free of evidence of recurrent or multifocal disease.
Discussion
Inflammatory pseudotumor (IPT) is a rare pathologic entity characterized by inflammatory and fibrous components. Histologic examination of this lesion reveals centrally localized mononuclear cells including lymphocytes, eosinophils, macrophages, plasma cells, and mast cells surrounded by proliferation of spindle cell–shaped mesenchymal cells and fibroblasts [7, 23]. Because of its variable histology, this entity has been referred to by a variety of terms, including inflammatory myofibrohystiocytic proliferation, inflammatory myofibroblastic tumor, and plasma cell granuloma. IPT is generally considered to be a benign lesion without malignant histologic features. However, recent reports of local recurrence and progressive multifocal disease have led some investigators to emphasize their potential for aggressive behavior and propose the possibility of malignant degeneration of pseudotumor lesions [5, 8, 12, 29].
Although IPT is most commonly seen in the lung, multiple extrapulmonary sites have been described, including liver, spleen, intestinal mesentery, lymphatics, and pancreas [6, 7].
Pancreatic IPT is rare, with only 27 reported cases in the English literature [1, 2, 3, 4, 9, 10, 11, 13, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 28, 30]. Patients with pancreatic IPT generally fall into two categories—those associated with retroperitoneal fibrosis and those isolated to the pancreas.
Patients with retroperitoneal fibrosis are often older individuals who present with abdominal pain, jaundice, and weight loss. Although operative exploration and resection of the pancreatic mass remains the mainstay of therapy for these patients, there have been several reports of regression of the pancreatic IPT and resolution of symptoms after corticosteroid therapy [3, 4, 11].
IPT isolated to the pancreas can have a variety of presentations. Many of these presentations can be attributable to local effects of the mass; they include abdominal or back pain, anorexia, nausea, emesis, weight loss, jaundice, anemia, and fatigue [13, 23]. The etiology of pancreatic IPT is unclear. The pathogenesis of this lesion may involve autoimmune processes; various authors have shown associations between IPT of the pancreas and other autoimmune-mediated diseases, such as Crohn’s colitis, Sjogren’s syndrome, retroperitoneal fibrosis, and idiopathic thrombocytopenic purpura [13, 22, 25]. An infectious etiology may also play a role in the development of this lesion. It has been hypothesized that an infectious agent may incite a localized immune response, leading to the recruitment of inflammatory cells and development of the fibrous changes seen in this lesion. Epstein-Barr virus (EBV) may be a likely candidate for this infectious agent because it has been identified in IPT of the liver and spleen [2, 15]. However, pancreatic IPT lesions that have been tested have not yet shown EBV [19].
The presentation and radiographic appearance of pancreatic IPT usually mandates operative exploration and pancreatic resection to rule out malignancy. Rarely is the diagnosis made preoperatively, although it can be suspected in the patient who has a pancreatic mass in the setting of an associated condition such as sclerosing cholangitis or retroperitoneal fibrosis. Even in such patients, care must be taken when contemplating nonoperative therapy in a patient with a potential pancreatic malignancy.
Resection can be attained either by pancreaticoduodenectomy, distal pancreatectomy, or total pancreatectomy, and resection often results in the resolution of the presenting symptoms. In all previous reports of resection of pancreatic IPT, laparotomy and open resection were used. Although laparoscopic splenectomy has been reported for splenic IPT, this is the first reported case of pancreatic IPT resected laparoscopically [27].
The prognosis of patients with pancreatic IPT is quite favorable. Resection by partial pancreatectomy or pancreaticodoudenectomy usually decreases or eliminates presenting symptoms of abdominal pain, nausea, and biliary obstruction. Although several authors have reported the development of subsequent multifocal ITP or local recurrence after resection, most patients undergo curative resection and remain free of disease at follow-up [5, 8, 12, 29].
Conclusion
Inflammatory pseudotumor of the pancreas is a rare entity that can present clinically and radiographically as a malignant lesion of the pancreas. For this reason, these lesions are generally treated by resection in appropriate surgical candidates. Laparoscopic distal pancreatectomy is an alternative to open resection in patients with lesions in the tail of the pancreas. Microscopic examination of IPT reveals a benign lesion, and thus complete resection results in definitive treatment.
References
P Abrebanel S Sarfaty R Gal C Chaimoff E Kessler (1984) ArticleTitlePlasma cell granuloma of the pancreas. Arch Pathol Lab Med 108 531–532 Occurrence Handle1:STN:280:DyaL2c3jtVGgsQ%3D%3D Occurrence Handle6547314
DA Arber OW Kamel M Rijn Particlevan de RE Davis LJ Medeiros ES Jaffe LM Weiss (1995) ArticleTitleFrequent presence of the Epstein-Barr virus in inflammatory pseudotumor. Hum Pathol 26 1093–1098 Occurrence Handle1:STN:280:DyaK28%2Fhtl2huw%3D%3D Occurrence Handle10.1016/0046-8177(95)90271-6
A Chutaputti MI Burrell JL Boyer (1995) ArticleTitlePseudotumor of the pancreas associated with retroperitoneal fibrosis: a dramatic response to corticosteroid therapy. Am J Gastroenterol 90 1155–1158 Occurrence Handle1:STN:280:DyaK2MzjsFGquw%3D%3D Occurrence Handle7611217
A Clark RK Zeman PL Choyke EM White MI Burrell EG Grant MH Jaffe (1988) ArticleTitlePancreatic pseudotumors associated with multifocal idiopathic fibrosclerosis. Gastrointest Radiol 13 30–32 Occurrence Handle1:STN:280:DyaL1c7mslGnug%3D%3D Occurrence Handle10.1007/BF01889019
CM Coffin LP Dehner JM Meis-Kindblom (1998) ArticleTitleInflammatory myofibroblastic tumor, inflammatory fibrosarcoma, and related lesions: an historical review with differential diagnostic considerations. Semin Diagn Pathol 15 102–110 Occurrence Handle1:STN:280:DyaK1c3mvFKntQ%3D%3D Occurrence Handle9606802
CM Coffin PA Humphrey LP Dehner (1998) ArticleTitleExtrapulmonary inflammatory myofibroblastic tumor: a clinical and pathological survey. Semin Diagn Pathol 15 85–101 Occurrence Handle1:STN:280:DyaK1c3mvFKntA%3D%3D Occurrence Handle9606801
CM Coffin J Watterson JR Priest LP Dehner (1995) ArticleTitleExtrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor): a clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol 19 859–872 Occurrence Handle1:STN:280:DyaK2MzjsF2ntQ%3D%3D Occurrence Handle10.1097/00000478-199508000-00001
LR Donner RA Trompler 4th White RR (1996) ArticleTitleProgression of inflammatory myofibroblastic tumor (inflammatory pseudotumor) of soft tissue into sarcoma after several recurrences. Hum Pathol 27 1095–1098 Occurrence Handle1:STN:280:DyaK2s%2FkslOmtQ%3D%3D Occurrence Handle10.1016/S0046-8177(96)90291-9
KM Dudiak (1993) ArticleTitleAbdominal case of the day: inflammatory pseudotumor of the pancreas. AJR 160 1324–1325 Occurrence Handle1:STN:280:DyaK3s3mvFOhsw%3D%3D Occurrence Handle10.2214/ajr.160.6.8498248
RP Eckstein RM Rollings PA Martin CH Katelaris (1995) ArticleTitlePancreatic pseudotumor arising in association with Sjogren’s syndrome. Pathology 27 284–288 Occurrence Handle1:STN:280:DyaK287gsF2gtQ%3D%3D Occurrence Handle10.1080/00313029500169133
L Inaraja T Franquet P Caballero B Encabo P Humbert (1986) ArticleTitleCT findings in circumscribed upper abdominal idiopathic retroperitoneal fibrosis. J Comput Assist Tomogr 10 1063–1064 Occurrence Handle1:STN:280:DyaL2s%2FlvVaqsA%3D%3D Occurrence Handle10.1097/00004728-198611000-00038
RL Johnson DL Page RH Dean (1983) ArticleTitlePseudotumor of the pancreas. South Med J 76 647–649 Occurrence Handle1:STN:280:DyaL3s7pslKmtQ%3D%3D Occurrence Handle10.1097/00007611-198305000-00028
TH Liu ET Consorti (2000) ArticleTitleInflammatory pseudotumor presenting as a cystic tumor of the pancreas. Am Surg 66 993–997 Occurrence Handle1:STN:280:DC%2BD3M%2FmvVCnsQ%3D%3D Occurrence Handle11090004
MB McClain EM Burton DS Day (2000) ArticleTitlePancreatic pseudotumor in an 11-year-old child: imaging findings. Pediatr Radiol 30 610–613 Occurrence Handle1:STN:280:DC%2BD3cvlt12itQ%3D%3D Occurrence Handle10.1007/s002470000227
DM Menke H Griesser I Araujo HD Foss H Herbst PM Banks H Stein (1996) ArticleTitleInflammatory pseudotumors of lymph node origin show macrophage-derived spindle cells and lymphocyte-derived cytokine transcripts without evidence of T-cell receptor gene rearrangements: implications for pathogenesis and classification as an idiopathic retroperitoneal fibrosis-like sclerosing immune reaction. Am J Clin Pathol 105 430–439 Occurrence Handle1:STN:280:DyaK287otFSksA%3D%3D Occurrence Handle10.1093/ajcp/105.4.430
G Morris-Stiff GM Vujanic A Al-Wafi J Lari (1998) ArticleTitlePancreatic inflammatory pseudotumour: an uncommon childhood lesion mimicking a malignant tumour. Pediatr Surg Int 13 52–54 Occurrence Handle1:STN:280:DyaK1c%2FlsVCjsA%3D%3D Occurrence Handle10.1007/s003830050243
JP Palazzo CD Chang (1993) ArticleTitleInflammatory pseudotumour of the pancreas. Histopathology 23 475–477 Occurrence Handle1:STN:280:DyaK2c7kvVersw%3D%3D Occurrence Handle10.1111/j.1365-2559.1993.tb00498.x
JF Perry SuffixJr JW LaFave WB Carpenter (1965) ArticleTitleRetroperitoneal fibrosis simulating carcinoma of the pancreas. Minn Med 48 371–374 Occurrence Handle14255324
LM Petter JK Martin SuffixJr DM Menke (1998) ArticleTitleLocalized lymphoplasmacellular pancreatitis forming a pancreatic inflammatory pseudotumor. Mayo Clin Proc 73 447–450 Occurrence Handle1:STN:280:DyaK1c3ktVKlsA%3D%3D Occurrence Handle10.1016/S0025-6196(11)63728-2
DJ Purdy EJ Levine KJ Forsthoefel JJ Fromkes (1994) ArticleTitlePeriampullary pseudotumor secondary to granulomatous disease. Am J Gastroenterol 89 2087–2088 Occurrence Handle1:STN:280:DyaK2M%2FivFaltg%3D%3D Occurrence Handle7942748
IG Renner GC Ponto 3rd Savage WT WD Boswell (1980) ArticleTitleIdiopathic retroperitoneal fibrosis producing common bile duct and pancreatic duct obstruction. Gastroenterology 79 348–351 Occurrence Handle1:STN:280:DyaL3c3kslelsA%3D%3D Occurrence Handle10.1016/0016-5085(80)90153-5
H Reynaert O Peters J Auwera ParticleVan der MJ Vanstapel D Urbain (2001) ArticleTitleJaundice caused by a pancreatic mass: an exceptional presentation of Crohn’s disease. J Clin Gastroenterol 32 255–258 Occurrence Handle1:STN:280:DC%2BD3M7mslGqsA%3D%3D Occurrence Handle10.1097/00004836-200103000-00018
L Scott G Blair G Taylor J Dimmick G Fraser (1988) ArticleTitleInflammatory pseudotumors in children. J Pediatr Surg 23 755–758 Occurrence Handle1:STN:280:DyaL1M%2FhtFarsA%3D%3D Occurrence Handle10.1016/S0022-3468(88)80419-6
KR Shankar PD Losty MM Rhine GL Lamont HP McDowell (1998) ArticleTitlePancreatic inflammatory tumour: a rare entity in childhood. J R Coll Surg Edinb 43 422–423 Occurrence Handle1:STN:280:DyaK1M7ksVKjtQ%3D%3D Occurrence Handle9990796
G Stathopoulos AD Nourmand M Blackstone D Andersen AL Baker (1995) ArticleTitleRapidly progressive sclerosing cholangitis following surgical treatment of pancreatic pseudotumor. J Clin Gastroenterol 21 143–148 Occurrence Handle1:STN:280:DyaK28%2FmsVWrtw%3D%3D Occurrence Handle10.1097/00004836-199509000-00016
MD Stringer P Ramani CK Yeung SN Capps EM Kiely L Spitz (1992) ArticleTitleAbdominal inflammatory myofibroblastic tumours in children. Br J Surg 79 1357–1360 Occurrence Handle1:STN:280:DyaK3s7js12muw%3D%3D Occurrence Handle10.1002/bjs.1800791239
K Tsugawa M Hashizume S Migou H Kawanaka K Sugimachi H Irie T Maeda et al. (1998) ArticleTitleLaparoscopic splenectomy for an inflammatory pseudotumor of the spleen: operative technique and case report. Hepatogastroenterology 45 1887–1891 Occurrence Handle1:STN:280:DyaK1M%2Fltl2jtw%3D%3D Occurrence Handle9840170
I Uzoaru P Chou M Reyes-Mugica (1993) ArticleTitleInflammatory myofibroblastic tumor of the pancreas. Surg Pathol 5 181–188
SD Voss JB Kruskal RA Kane (1999) ArticleTitleChronic inflammatory pseudotumor arising in the hepatobiliary-pancreatic system: progressive multisystemic organ involvement in four patients. AJR 173 1049–1054 Occurrence Handle1:STN:280:DyaK1MvjvFWqtg%3D%3D Occurrence Handle10.2214/ajr.173.4.10511176
W Wiesner T Kocher C Beglinger F Harder W Steinbrich (2001) ArticleTitlePseudotumor of the pancreatic head associated with idiopathic retroperitoneal fibrosis. Dig Surg 18 418–421 Occurrence Handle1:STN:280:DC%2BD3MnnsV2guw%3D%3D Occurrence Handle10.1159/000050184
Acknowledgments
We thank Syed Hoda, MD, and Anuradha Goplaln, MD, for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DeRubertis, B.G., McGinty, J., Rivera, M. et al. Laparoscopic distal pancreatectomy for inflammatory pseudotumor of the pancreas. Surg Endosc 18, 1001 (2004). https://doi.org/10.1007/s00464-003-4546-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-4546-9