Abstract
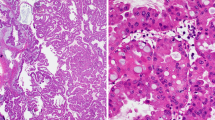
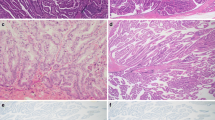
Intestinal-type intraductal papillary mucinous neoplasm (IPMN) of the pancreas is clinicopathologically distinctive. Our research aimed to elucidate the molecular mechanism of the development and progression of the intestinal-type IPMN. In 60 intestinal-type IPMN specimens, histological transitions from gastric-type epithelia to intestinal-type epithelia were observed in 48 cases (80%). CDX2/MUC2/alcian blue triple staining indicated that CDX2 appeared to precede MUC2 expression and subsequent alcian blue-positive mucin production. Expression of p21 and Ki-67 seemed to be accelerated by CDX2 expression (p = 6.02e-13 and p = 3.1e-09, respectively). p21/Ki-67 double staining revealed that p21 was mostly expressed in differentiated cells in the apex of papillae, while Ki-67 was expressed in proliferative cells in the base of papillae. This clear cellular arrangement seemed to break down with the progression of atypical grade and development of invasion (p = 0.00197). Intestinal-type IPMNs harbored frequent GNAS mutations (100%, 25/25) and RNF43 mutations (57%, 8/14) and shared identical GNAS and KRAS mutations with concurrent gastric-type IPMNs or incipient gastric-type neoplasia (100%, 25/25). RNF43 mutations showed emerging or being selected in intestinal-type neoplasms along with ß-catenin aberration. Activation of protein kinase A and extracellular-regulated kinase was observed in CDX2-positive intestinal-type neoplasm. These results suggest that gastric-type epithelia that acquire GNAS mutations together with induction of intrinsic CDX2 expression may evolve with clonal selection and additional molecular aberrations including RNF43 and ß-catenin into intestinal-type IPMNs, which may further progress with complex villous growth due to disoriented cell cycle regulation, acceleration of atypical grade, and advance to show an invasive phenotype.





Similar content being viewed by others
Data availability
Supplementary information is available at Virchows Archiv’s website.
References
Furukawa T, Klöppel G, Volkan Adsay N, Albores-Saavedra J, Fukushima N, Horii A, Hruban RH, Kato Y, Klimstra DS, Longnecker DS, Lüttges J, Offerhaus GJ, Shimizu M, Sunamura M, Suriawinata A, Takaori K, Yonezawa S (2005) Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch 447:794–799
Adsay V, Mino-Kenudson M, Furukawa T, Basturk O, Zamboni G, Marchegiani G, Bassi C, Salvia R, Malleo G, Paiella S, Wolfgang CL, Matthaei H, Offerhaus GJ, Adham M, Bruno MJ, Reid MD, Krasinskas A, Klöppel G, Ohike N, Tajiri T, Jang KT, Roa JC, Allen P, Fernández-del Castillo C, Jang JY, Klimstra DS, Hruban RH (2016) Pathologic evaluation and reporting of intraductal papillary mucinous neoplasms of the pancreas and other tumoral intraepithelial neoplasms of pancreatobiliary tract: recommendations of Verona consensus meeting. Ann Surg 263:162–177
Basturk O, Hong SM, Wood LD, Adsay NV, Albores-Saavedra J, Biankin AV, Brosens LA, Fukushima N, Goggins M, Hruban RH, Kato Y, Klimstra DS, Klöppel G, Krasinskas A, Longnecker DS, Matthaei H, Offerhaus GJ, Shimizu M, Takaori K, Terris B, Yachida S, Esposito I, Furukawa T (2015) A revised classification system and recommendations from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol 39:1730–1741
Furukawa T, Hatori T, Fujita I, Yamamoto M, Kobayashi M, Ohike N, Morohoshi T, Egawa S, Unno M, Takao S, Osako M, Yonezawa S, Mino-Kenudson M, Lauwers GY, Yamaguchi H, Ban S, Shimizu M (2011) Prognostic relevance of morphological types of intraductal papillary mucinous neoplasms of the pancreas. Gut 60:509–516
Gum JR, Byrd JC, Hicks JW, Toribara NW, Lamport DT, Kim YS (1989) Molecular cloning of human intestinal mucin cDNAs. Sequence analysis and evidence for genetic polymorphism. J Biol Chem 264:6480–6487
Kwak HA, Liu X, Allende DS, Pai RK, Hart J, **ao SY (2016) Interobserver variability in intraductal papillary mucinous neoplasm subtypes and application of their mucin immunoprofiles. Mod Pathol 29:977–984
Adsay NV, Merati K, Basturk O, Iacobuzio-Donahue C, Levi E, Cheng JD, Sarkar FH, Hruban RH, Klimstra DS (2004) Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasms: delineation of an “intestinal” pathway of carcinogenesis in the pancreas. Am J Surg Pathol 28:839–848
Allen A, Hutton DA, Pearson JP (1998) The MUC2 gene product: a human intestinal mucin. Int J Biochem Cell Biol 30:797–801
James R, Erler T, Kazenwadel J (1994) Structure of the murine homeobox gene cdx2. Expression in embryonic and adult intestinal epithelium. J Biol Chem 269:15229–15237
Guo RJ, Suh ER, Lynch JP (2004) The role of Cdx proteins in intestinal development and cancer. Cancer Biol Ther 3:593–601
Yamamoto H, Bai Y-Q, Yuasa Y (2003) Homeodomain protein CDX2 regulates goblet-specific MUC2 gene expression. Biochem Biophys Res Commun 300:813–818
Kuboki Y, Shimizu K, Hatori T, Yamamoto M, Shibata N, Shiratori K, Furukawa T (2015) Molecular biomarkers for progression of intraductal papillary mucinous neoplasm of the pancreas. Pancreas 44:227–235
Furukawa T, Fukushima N, Itoi T, Ohike N, Mitsuhashi T, Nakagohri T, Notohara K, Shimizu M, Tajiri T, Tanaka M, Yamaguchi H, Yanagisawa A, Sugiyama M, Okazaki K (2019) A consensus study of the grading and ty** of intraductal papillary mucinous neoplasms of the pancreas. Pancreas 48:480–487
Omori Y, Ono Y, Tanino M, Karasaki H, Yamaguchi H, Furukawa T, Enomoto K, Ueda J, Sumi A, Katayama J, Muraki M, Taniue K, Takahashi K, Ambo Y, Shinohara T, Nishihara H, Sasajima J, Maguchi H, Mizukami Y, Okumura T, Tanaka S (2019) Pathways of progression from intraductal papillary mucinous neoplasm to pancreatic ductal adenocarcinoma based on molecular features. Gastroenterology 156:647–661.e2
Yeh TS, Ho YP, Chiu CT, Chen TC, Jan YY, Chen MF (2005) Aberrant expression of CDX2 homeobox gene in intraductal papillary-mucinous neoplasm of the pancreas but not in pancreatic ductal adenocarcinoma. Pancreas 30:233–238
Bai YQ, Miyake S, Iwai T, Yuasa Y (2003) CDX2, a homeobox transcription factor, upregulates transcription of the p21/WAF1/CIP1 gene. Oncogene 22:7942–7949
Jiao YF, Nakamura S, Sugai T, Yamada N, Habano W (2008) Serrated adenoma of the colorectum undergoes a proliferation versus differentiation process: new conceptual interpretation of morphogenesis. Oncology 74:127–134
Komori K, Ajioka Y, Watanabe H, Oda K, Nimura Y (2003) p21WAF1/CIP1 and Ki-67 expression of serrated adenoma of the colorectum: an investigation of cell differentiation/maturation and its relationship with cell proliferation. Acta Med Biol 51:117–124
Doglioni C, Pelosio P, Laurino L, Macri E, Meggiolaro E, Favretti F, Barbareschi M (1996) p21/WAF1/CIP1 expression in normal mucosa and in adenomas and adenocarcinomas of the colon: its relationship with differentiation. J Pathol 179:248–253
Gala MK, Mizukami Y, Le LP, Moriichi K, Austin T, Yamamoto M, Lauwers GY, Bardeesy N, Chung DC (2014) Germline mutations in oncogene-induced senescence pathways are associated with multiple sessile serrated adenomas. Gastroenterology 146:520–529
Yan HHN, Lai JCW, Ho SL, Leung WK, Law WL, Lee JFY, Chan AKW, Tsui WY, Chan ASY, Lee BCH, Yue SSK, Man AHY, Clevers H, Yuen ST, Leung SY (2017) RNF43 germline and somatic mutation in serrated neoplasia pathway and its association with BRAF mutation. Gut 66:1645–1656
Lee JH, Kim Y, Choi JW, Kim YS (2016) KRAS, GNAS, and RNF43 mutations in intraductal papillary mucinous neoplasm of the pancreas: a meta-analysis. Springerplus 26:1172
Kinzler KW, Vogelstein B (1996) Lessons from hereditary colorectal cancer. Cell 18:159–170
Network CGA (2012) Comprehensive molecular characterization of human colon and rectal cancer. Nature 487:330–337
Taki K, Ohmuraya M, Tanji E, Komatsu H, Hashimoto D, Semba K, Araki K, Kawaguchi Y, Baba H, Furukawa T (2016) GNASR201H and KrasG12D cooperate to promote murine pancreatic tumorigenesis recapitulating human intraductal papillary mucinous neoplasm. Oncogene 35:2407–2412
Patra KC, Kato Y, Mizukami Y, Widholz S, Boukhali M, Revenco I, Grossman EA, Ji F, Sadreyev RI, Liss AS, Screaton RA, Sakamoto K, Ryan DP, Mino-Kenudson M, Castillo CF, Nomura DK, Haas W, Bardeesy N (2018) Mutant GNAS drives pancreatic tumourigenesis by inducing PKA-mediated SIK suppression and reprogramming lipid metabolism. Nat Cell Biol 20:811–822
Ideno N, Yamaguchi H, Ghosh B, Gupta S, Okumura T, Steffen DJ, Fisher CG, Wood LD, Singhi AD, Nakamura M, Gutkind JS, Maitra A (2018) GNASR201C induces pancreatic cystic neoplasms in mice that express activated KRAS by inhibiting YAP1 signaling. Gastroenterology 155:1593–1607 e12
Sakamoto H, Kuboki Y, Hatori T, Yamamoto M, Sugiyama M, Shibata N, Shimizu K, Shiratori K, Furukawa T (2015) Clinicopathological significance of somatic RNF43 mutation and aberrant expression of ring finger protein 43 in intraductal papillary mucinous neoplasms of the pancreas. Mod Pathol 28:261–267
Dhanasekaran DN (2006) Transducing the signals: a G protein takes a new identity. Sci STKE 347:pe31
Landis CA, Masters SB, Spada A, Pace AM, Bourne HR, Vallar L (1989) GTPase inhibiting mutations activate the alpha chain of Gs and stimulate adenylyl cyclase in human pituitary tumours. Nature 340:692–696
Komatsu H, Tanji E, Sakata N, Aoki T, Motoi F, Naitoh T, Katayose Y, Egawa S, Unno M, Furukawa T (2014) A GNAS mutation found in pancreatic intraductal papillary mucinous neoplasms induces drastic alterations of gene expression profiles with upregulation of mucin genes. PLoS One 9:e87875
Acknowledgments
We would like to thank Ms. Fumiko Date (Biomedical Research Core of Tohoku University Graduate School of Medicine) for tissue sample preparation, and Ms. Yuko Hayakawa (Sapporo Higashi Tokushukai Hospital) for technical support in the genetic analysis. The authors would also like to thank Mr. David Hochman for the editorial review of the manuscript.
Funding
This work was supported by the Japan Society for the Promotion of Science, KAKENHI Grant Number JP19K16576 (to Y. Omori).
Author information
Authors and Affiliations
Contributions
Y. Omori and T.F. performed the histological analysis; Y. Omori performed the immunohistochemical analysis; Y. Omori and Y. Ono performed genetic analysis and Y. Omori interpreted the data; T.K., F.M., and M.U. collected clinical samples; Y. Omori obtained the funding; Y.M., H.K., N.M., Y.U., and T.F. supervised the project; Y. Omori developed the concept, designed experimental studies, analyzed the data, and wrote the manuscript with feedback from all authors. T.F. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board of Tohoku University, Graduated School of Medicine (#2018-1-752).
Conflict of interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 47553 kb).
Rights and permissions
About this article
Cite this article
Omori, Y., Ono, Y., Kobayashi, T. et al. How does intestinal-type intraductal papillary mucinous neoplasm emerge? CDX2 plays a critical role in the process of intestinal differentiation and progression. Virchows Arch 477, 21–31 (2020). https://doi.org/10.1007/s00428-020-02806-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-020-02806-8