Abstract
Background
Astigmatism is commonly reported in children with and without nystagmus. In children less than 4 years of age the astigmatism changes from against the rule (ATR) to with the rule (WTR) astigmatism in children without nystagmus. However, little is known about children with congenital nystagmus. We compared astigmatism in children with congenital nystagmus below 4 years and above 4 years of age.
Material and methods
Three hundred and fifty-six eyes in 178 children who satisfied the study criteria were included. The children were divided into those below 4 years of age (n of eyes = 192) and those above (n of eyes = 164). Cycloplegic refraction (with manual retinoscopy) carried out at presentation and at the last follow-up were recorded and compared. Cycloplegia was achieved using cyclopentolate eye drops. Outcome of eyes with no astigmatism at initial presentation was compared with the final refraction in both the age groups. The visual acuity at the first presentation was compared with the visual acuity at the last presentation.
Results
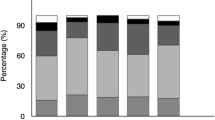
Average follow-up duration was 3.36±1.59 years. On presentation, 176 (49.44%) eyes did not have any astigmatism. We found that 26 (25.2%) out of the 103 children below 4 years of age who did not have any astigmatism on presentation developed WTR astigmatism after a mean follow-up of 3.5±1.5 years. (p= 0.042). In children ≥4 years of age only 7 (9.6%) children out of 73 developed WTR after a mean follow-up of 3.4±1.4 years. The visual acuity change was not found to be significant in the two groups. The majority (90.3%) improved or had same visual acuity in group A and 88.9% improved or had the same visual acuity in group B at the last follow-up (p= 0.77).
Discussion
Our incidence of WTR astigmatism in children with congenital nystagmus is similar to those previously reported series. Our data suggest that there is a significant chance that children under 4 years with congenital nystagmus may develop WTR astigmatism compared with children above 4 years of age.
Conclusion
With the rule (WTR) astigmatism is common in children with nystagmus. Children under 4 years of age presenting with no astigmatism may acquire WTR astigmatism as they grow. The amount of astigmatism increases with age in children with nystagmus. Visual acuity, however, remains stable as the age advances.
Similar content being viewed by others
References
Abadi RV, Bjerre A (2002) Motor and sensory characteristics of infantile nystagmus. Br J Ophthalmol 86:1152–1160
Abrahamsson M, Fabian G, Sjostrand J (1988). Changes in astigmatism between the ages of 1 and 4 years: a longitudinal study. Br J Ophthalmol 72:145–149
Brodsky MC, Baker RS, Hamed LM (1996) Paediatric neuroophthalmology, 1st edn. Springer, New York Berlin Heidelberg, pp 302–349
Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Munoz SR, Pokharel GP, Ellwein LB (2002) Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci 43:615–622
Dickinson CM, Abadi RV (1984) Corneal topography of humans with congenital nystagmus. Ophthalmic Physiol Opt 4:3–13
Dobson V, Fultron AB, Sebris L (1984) Cycloplegic refractions of infants and young children: the axis of astigmatism. Invest Ophthalmol Vis Sci 25:83–87
Gwiazda J, Scheiman M, Mohindra I, Held R (1984) Astigmatism in children: changes in axis and amount from birth to six years. Invest Ophthalmol Vis Sci 25:88–92
Hertle RW (2000) Examination and refractive management of patients with nystagmus. Surv Ophthalmol 455:215–222
Hertle RW, Zhu X (1999) Oculographic and clinical characterisation of thirty-seven children with anomalous head postures, nystagmus and strabismus: the basis of clinical algorithm. JAAPOS 3:25–32
Montes-Mico R (2000) Astigmatism in infancy and childhood. J Paediatr Ophthalmol Strabismus 37:349–353
Murthy GVS, Gupta SV, Ellwein LB, Munoz SR, Pokharel GP, Sanga L, Bachani D (2002) Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 43:623–631
Ohmi G, Reinecke RD (1993) Astigmatism of nystagmus subjects. Invest Ophthalmol Vis Sci 34 [Suppl]:1125
Sampath V, Bedell HE (2002) Distribution of refractive errors in albinos and persons with idiopathic congenital nystagmus. Optom Vis Sci 79:292–299
Tong L, Saw SM, Chia KS, Koh D, Tan D (2004) Incidence and progression of astigmatism in Singaporean children. Invest Ophthalmol Vis Sci 45:3914–3918
Wildsoet CF, Oswald PJ, Clark S (2000) Albinism: its implications for refractive development. Invest Ophthalmol Vis Sci 41:1–7
Acknowledgement
We acknowledge Dr. Stephen Kraft, Ontario, Canada for his valuable comments and timely help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jethani, J., Prakash, K., Vijayalakshmi, P. et al. Changes in astigmatism in children with congenital nystagmus. Graefe's Arch Clin Exp Ophthalmo 244, 938–943 (2006). https://doi.org/10.1007/s00417-005-0157-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0157-6