Abstract
Purpose
Rectal gastrointestinal stromal tumors (GISTs) surgery is often challenging owing to the anatomical constraints of the narrow pelvis and tumor hugeness. Despite the increasing number of patients undergoing trans-anal total mesorectal excision (taTME) globally, the feasibility of trans-anal surgery with the taTME technique for rectal GISTs remains unclear. We aimed to evaluate the feasibility of trans-anal surgery with the taTME technique for rectal GISTs.
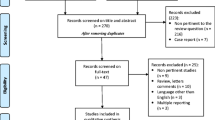
Methods
Using a prospectively collected database, we retrospectively analyzed the clinical findings, surgical outcomes, pathological outcomes, urinary and anal functions, and prognoses of patients who underwent trans-anal surgery with the taTME technique for primary rectal GISTs at the National Cancer Center Hospital East from September 2014 to March 2020.
Results
Twenty-one patients with primary rectal GISTs were included in this study. The median distance from the anal verge to the lower edge of the tumor was 40 mm (range, 15–60 mm), and the median tumor size was 59 mm (range, 11–175 mm). Moreover, seven and 14 patients underwent one-team and two-team surgeries, respectively, with curative intent. Nineteen patients (90.5%) underwent anus-preserving surgery, and the urinary tracts were preserved in all cases. Two-team surgery showed a significantly lower blood loss volume and shorter operation time than one-team surgery (58 vs. 222 mL, P = 0.017; 184 vs 356 min, P = 0.041, respectively). The pathological negative-margin resection rate was 100%. During the follow-up period, no patient developed local GIST recurrence and one (4.8%) developed distant metastasis.
Conclusion
Trans-anal surgery with the taTME technique is feasible for rectal GISTs, and two-team surgery may be more advantageous than one-team surgery in terms of operation time and blood loss.

Similar content being viewed by others
Data sharing and accessibility
The datasets generated and analyzed during the present study are available from the corresponding author upon reasonable request.
References
Tran T, Davila JA, El-Serag HB (2005) The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol 100:162–168. https://doi.org/10.1111/j.1572-0241.2005.40709.x
Wilkinson MJ, Fitzgerald JEF, Strauss DC, Hayes AJ, Thomas JM, Messiou C et al (2015) Surgical treatment of gastrointestinal stromal tumour of the rectum in the era of imatinib. Br J Surg 102:965–971. https://doi.org/10.1002/bjs.9818
DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF (2000) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231:51–58. https://doi.org/10.1097/00000658-200001000-00008
Duffaud F, Blay JY (2003) Gastrointestinal stromal tumors: biology and treatment. Oncology 65:187–197. https://doi.org/10.1159/000074470
Kumar M, Goel MM, Singh D (2013) Rare case of gastrointestinal stromal tumor of the anal canal. J Cancer Res Ther 9:736–738. https://doi.org/10.4103/0973-1482.126476
Singhal S, Singhal A, Tugnait R, Varghese V, Tiwari B, Arora PK et al (2013) Anorectal gastrointestinal stromal tumor: a case report and literature review. Case Rep Gastrointest Med 2013:934875. https://doi.org/10.1155/2013/934875
Manimaran D, Khan DM, Bharathi K, Raman TR, Anuradha S (2015) Gastrointestinal stromal tumor of the anal canal. Natl J Lab Med 4:38–39
Nagasaki T, Fukunaga Y, Akiyoshi T, Konishi T, Fujimoto Y, Nagayama S et al (2017) Laparoscopic total pelvic exenteration after neoadjuvant imatinib therapy for gastrointestinal stromal tumor of the rectum: a case report. Int Surg 102:205–209. https://doi.org/10.9738/INTSURG-D-15-00041.1
Kyo K, Azuma M, Okamoto K, Nishiyama M, Shimamura T, Maema A et al (2016) Neoadjuvant imatinib treatment and laparoscopic anus-preserving surgery for a large gastrointestinal stromal tumor of the rectum. World J Surg Oncol 14:68. https://doi.org/10.1186/s12957-016-0837-1
Fujimoto Y, Akiyoshi T, Konishi T, Nagayama S, Fukunaga Y, Ueno M (2014) Laparoscopic sphincter-preserving surgery (intersphincteric resection) after neoadjuvant imatinib treatment for gastrointestinal stromal tumor (GIST) of the rectum. Int J Colorectal Dis 29:111–116. https://doi.org/10.1007/s00384-013-1769-7
Nakamura T, Ihara A, Mitomi H, Kokuba Y, Sato T, Ozawa H et al (2007) Gastrointestinal stromal tumor of the rectum resected by laparoscopic surgery: report of a case. Surg Today 37:1004–1008. https://doi.org/10.1007/s00595-007-3509-5
Nagano S, Miyoshi N, Takahashi T, Itakura H, Fu**o S, Ogino T et al (2020) Preoperative imatinib and laparoscopic intersphincteric resection for large rectal gastrointestinal stromal tumor: a case report. Int J Surg Case Rep 71:235–239. https://doi.org/10.1016/j.ijscr.2020.05.031
Sylla P, Rattner DW, Delgado S, Lacy AM (2010) NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 24:1205–1210. https://doi.org/10.1007/s00464-010-0965-6
van Oostendorp SE, Koedam TWA, Sietses C, Bonjer HJ, Tuynman JB (2018) Transanal total mesorectal excision compared to laparoscopic TME for mid and low rectal cancer – current evidence. Ann Laparosc Endosc Surg 3:41. https://doi.org/10.21037/ales.2018.04.02
Lacy AM, Tasende MM, Delgado S, Fernandez-Hevia M, Jimenez M, De Lacy B et al (2015) Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg 221:415–423. https://doi.org/10.1016/j.jamcollsurg.2015.03.046
Shiraishi T, Ito M, Sasaki T, Nishizawa Y, Tsukada Y, Ikeda K (2021) Association between urinary function and resected pattern of the autonomic nerve system after transanal total mesorectal excision for rectal cancer. Colorectal Dis 23:405–414. https://doi.org/10.1111/codi.15416
Enomoto H, Ito M, Sasaki T, Nishizawa Y, Tsukada Y, Ikeda K, Hasegawa H (2022) Anastomosis-related complications following stapled anastomosis with reinforced sutures in transanal total mesorectal excision for low rectal cancer: A retrospective single-center study. Dis Colon Rectum 65:2021. https://doi.org/10.1097/DCR.0000000000002016
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J et al (2019) Incidence and risk factors for anastomotic failure in 1594 patients treated by transanal total mesorectal excision: results from the international TaTME registry. Ann Surg 269:700–711. https://doi.org/10.1097/SLA.0000000000002653
Roodbeen SX, De Lacy FB, van Dieren S, Penna M, Ris F, Moran B et al (2019) Predictive factors and risk model for positive circumferential resection margin rate after transanal total mesorectal excision in 2653 patients with rectal cancer. Ann Surg 270:884–891. https://doi.org/10.1097/SLA.0000000000003516
Hasegawa S, Okada T, Hida K, Kawada K, Sakai Y (2016) Transperineal minimally invasive approach for extralevator abdominoperineal excision. Surg Endosc 30:4620–4621. https://doi.org/10.1007/s00464-015-4736-2
Nagakari K, Matoba S, Toda S, Maeda Y, Ueno M, Kuroyanagi H (2021) Hybrid resection of massive rectal gastrointestinal stromal tumor using laparoscopic and transanal approaches. Asian J Endosc Surg 14:102–105. https://doi.org/10.1111/ases.12824
Wachter N, Wörns MA, Dos Santos DP, Lang H, Huber T, Kneist W (2016) Transanal minimally invasive surgery (TAMIS) approach for large juxta-anal gastrointestinal stromal tumour. J Minim Access Surg 12:289–291. https://doi.org/10.4103/0972-9941.181306
Carrillo R, Candia A, Rodriguez-Peralto JL, Caz V (1997) Prognostic significance of DNA ploidy and proliferative index (MIB-1 index) in gastrointestinal stromal tumors. Hum Pathol 28:160–165. https://doi.org/10.1016/s0046-8177(97)90100-3
Arroyave MC, DeLacy FB, Lacy AM (2017) Transanal total mesorectal excision (TaTME) for rectal cancer: step by step description of the surgical technique for a two-teams approach. Eur J Surg Oncol 43:502–505. https://doi.org/10.1016/j.ejso.2016.10.024
Ma B, Gao P, Song Y, Zhang C, Zhang C, Wang L et al (2016) Transanal total mesorectal excision (taTME) for rectal cancer: a systematic review and meta-analysis of oncological and perioperative outcomes compared with laparoscopic total mesorectal excision. BMC Cancer 16:380. https://doi.org/10.1186/s12885-016-2428-5
Chen CC, Lai YL, Jiang JK, Chu CH, Huang IP, Chen WS et al (2016) Transanal total mesorectal excision versus laparoscopic surgery for rectal cancer receiving neoadjuvant chemoradiation: a matched case-control study. Ann Surg Oncol 23:1169–1176. https://doi.org/10.1245/s10434-015-4997-y
Koedam TWA, Veltcamp Helbach MV, Van de Ven PM, Kruyt PM, van Heek NT, Bonjer HJ et al (2018) Transanal total mesorectal excision for rectal cancer: evaluation of the learning curve. Tech Coloproctol 22:279–287. https://doi.org/10.1007/s10151-018-1771-8
Imaizumi K, Tsukada Y, Komai Y, Nomura S, Ikeda K, Nishizawa Y et al (2019) Prediction of urinary retention after surgery for rectal cancer using voiding efficiency in the 24 h following Foley catheter removal. Int J Colorectal Dis 34:1431–1443. https://doi.org/10.1007/s00384-019-03333-y
Jorge JMN, Wexner SD (1993) Etiology and management of fecal incontinence. Dis Colon Rectum 36:77–97. https://doi.org/10.1007/BF02050307
Chaudhry UI, DeMatteo RP (2011) Advances in the surgical management of gastrointestinal stromal tumor. Adv Surg 45:197–209. https://doi.org/10.1016/j.yasu.2011.03.018
ESMO/European Sarcoma Network Working Group (2014) Gastrointestinal stromal tumours: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 25(Suppl 3):iii21–iii26. https://doi.org/10.1093/annonc/mdu255
Liu H, Yan Z, Liao G, Yin H (2014) Treatment strategy of rectal gastrointestinal stromal tumor (GIST). J Surg Oncol 109:708–713. https://doi.org/10.1002/jso.23562
Guo W, Yang Z, Wei Y, Qin X, Li C, Huang R et al (2020) Radical excision versus local resection for primary rectal gastrointestinal stromal tumors. Cohort Study Int J Surg 77:190–197. https://doi.org/10.1016/j.ijsu.2020.03.068
Jakob J, Mussi C, Ronellenfitsch U, Wardelmann E, Negri T, Gronchi A, Hohenberger P (2013) Gastrointestinal stromal tumor of the rectum: results of surgical and multimodality therapy in the era of imatinib. Ann Surg Oncol 20:586–592. https://doi.org/10.1245/s10434-012-2647-1
Pai VD, Demenezes JL, Patil PS, Saklani AP (2016) Multimodality therapy of rectal gastrointestinal stromal tumors in the era of imatinib-an Indian series. J Gastrointest Oncol 7:262–268. https://doi.org/10.3978/j.issn.2078-6891.2015.088
Agaimy A, Vassos N, Märkl B, Meidenbauer N, Köhler J, Spatz J et al (2013) Anorectal gastrointestinal stromal tumors: a retrospective multicenter analysis of 15 cases emphasizing their high local recurrence rate and the need for standardized therapeutic approach. Int J Colorectal Dis 28:1057–1064. https://doi.org/10.1007/s00384-013-1655-3
IJzerman NS, Mohammadi M, Tzanis D, Gelderblom H, Fiore M, Fumagalli E et al (2020) Quality of treatment and surgical approach for rectal gastrointestinal stromal tumour (GIST) in a large European cohort. Eur J Surg Oncol 46:1124–1130. https://doi.org/10.1016/j.ejso.2020.02.033
Shu P, Sun XF, Fang Y, Gao XD, Hou YY, Shen KT et al (2020) Clinical outcomes of different therapeutic modalities for rectal gastrointestinal stromal tumor: summary of 14-year clinical experience in a single center. Int J Surg 77:1–7. https://doi.org/10.1016/j.ijsu.2020.03.007
Eisenberg BL, Judson I (2004) Surgery and imatinib in the management of GIST: emerging approaches to adjuvant and neoadjuvant therapy. Ann Surg Oncol 11:465–475. https://doi.org/10.1245/ASO.2004.09.011
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J et al (2017) Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg 266:111–117. https://doi.org/10.1097/SLA.0000000000001948
Qu H, Xu Z, Ren Y, Gong Z, Ju RH, Zhang F et al (2022) Recent advancements in the treatment of rectal gastrointestinal stromal tumor: in era of imatinib. Cancer Manag Res 14:1141–1152. https://doi.org/10.2147/CMAR.S352860
Van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218. https://doi.org/10.1016/S1470-2045(13)70016-0
Burke JP, Martin-Perez B, Khan A, Nassif G, de Beche-Adams T, Larach SW et al (2016) Transanal total mesorectal excision for rectal cancer: early outcomes in 50 consecutive patients. Colorectal Dis 18:570–577. https://doi.org/10.1111/codi.13263
Aubert M, Mege D, Panis Y (2020) Total mesorectal excision for low and middle rectal cancer: laparoscopic versus transanal approach-a meta-analysis. Surg Endosc 34:3908–3919. https://doi.org/10.1007/s00464-019-07160-8
Chen CC, Lai YL, Jiang JK, Chu CH, Huang IP, Chen WS et al (2015) The evolving practice of hybrid natural orifice transluminal endoscopic surgery (NOTES) for rectal cancer. Surg Endosc 29:119–126. https://doi.org/10.1007/s00464-014-3659-7
Fernández-Hevia M, Delgado S, Castells A, Tasende M, Momblan D, Díaz del Gobbo GD et al (2015) Transanal total mesorectal excision in rectal cancer: short-term outcomes in comparison with laparoscopic surgery. Ann Surg 261:221–227. https://doi.org/10.1097/SLA.0000000000000865
Acknowledgements
We thank the staff of the National Cancer Center Hospital East, Kashiwa, Japan.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Takahiro Shigaki, Yuichiro Tsukada, and Masaaki Ito. The first draft of the manuscript was written by Takahiro Shigaki, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the provisions of the Declaration of Helsinki and approved by the institutional ethics review board of the National Cancer Center Hospital East, Japan (approval no. 2018–100). We applied opt-out method to obtain consent on this study using the document that was approved by the institutional review board.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shigaki, T., Tsukada, Y., Teramura, K. et al. Trans-anal surgery with the taTME technique for rectal gastrointestinal stromal tumors: a retrospective study. Int J Colorectal Dis 37, 1975–1982 (2022). https://doi.org/10.1007/s00384-022-04233-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04233-4