Abstract
Purpose
The severity of congenital tracheal stenosis (CTS) is commonly evaluated based on the degree of stenosis. However, it does not always reflect the clinical respiratory status. We applied computational fluid dynamics (CFD) to the assessment of CTS. The aim of this study was to evaluate its validity.
Methods
CFD models were constructed on 15 patients (12 preoperative models and 15 postoperative models) with CTS before and after surgery, using the computed tomographic data. Energy flux, needed to drive airflow, measured by CFD and the minimum cross-sectional area of the trachea (MCAT) were quantified and evaluated retrospectively.
Results
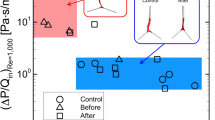
The energy flux correlated positively with the clinical respiratory status before and after surgery (rs = 0.611, p = 0.035 and rs = 0.591, p = 0.020, respectively). Although MCAT correlated negatively with the clinical respiratory status before surgery (rs = -0.578, p = 0.044), there was not significant correlation between the two after surgery (p = 0.572).
Conclusions
The energy flux measured by CFD assessment reflects the respiratory status in CTS before and after surgery. CFD can be an additional objective and quantitative evaluation tool for CTS.






Similar content being viewed by others
Data availability
Not applicable.
References
Hofferberth SC, Watters K, Rahbar R, Fynn-Thompson F (2015) Management of congenital tracheal stenosis. Pediatrics 136:e660–e669. https://doi.org/10.1542/peds.2014-3931
Antón-Pacheco JL, Cano I, Comas J, Galletti L, Polo L, García A, López M, Cabezalí D (2006) Management of congenital tracheal stenosis in infancy. Eur J Cardiothorac Surg 29:991–996
Cheng W, Manson DE, Forte V, Ein SH, MacLusky I, Papsin BC, Hechter S, Kim PC (2006) The role of conservative management in congenital tracheal stenosis: an evidence-based long-term follow-up study. J Pediatr Surg 41:1203–1207. https://doi.org/10.1016/j.jpedsurg.2006.03.046
Yamoto M, Fukumoto K, Sekioka A, Iwazaki T, Sano K, Takahashi T, Nakaya K, Nomura A, Yamada Y, Urushihara N (2019) Non-operative management of congenital tracheal stenosis: criteria by computed tomography. Pediatr Surg Int 35:1123–1130. https://doi.org/10.1007/s00383-019-04532-y
Mimouni-Benabu O, Meister L, Giordano J, Fayoux P, Loundon N, Triglia JM, Nicollas R (2012) A preliminary study of computer assisted evaluation of congenital tracheal stenosis: a new tool for surgical decision-making. Int J Pediatr Otorhinolaryngol 76:1552–1557. https://doi.org/10.1016/j.ijporl.2012.07.009
Qi S, Li Z, Yue Y, van Triest HJ, Kang Y (2014) Computational fluid dynamics simulation of airflow in the trachea and main bronchi for the subjects with left pulmonary artery sling. Biomed Eng Online 13:85. https://doi.org/10.1186/1475-925X-13-85
Takeishi N, Miki T, Otani T, Ii S, Morita K, Wada S (2019) Fluid dynamic assessment of tracheal flow in infants with congenital tracheal stenosis before and after surgery. Med Biol Eng Comput 57:837–847. https://doi.org/10.1007/s11517-018-1928-7
Bates AJ, Comerford A, Cetto R, Schroter RC, Tolley NS, Doorly DJ (2016) Power loss mechanisms in pathological tracheas. J Biomech 49:2187–2192. https://doi.org/10.1016/j.jbiomech.2015.11.033
**ao Q, Cetto R, Doorly DJ, Bates AJ, Rose JN, McIntyre C, Comerford A, Madani G, Tolley NS, Schroter R (2020) Assessing changes in airflow and energy loss in a progressive tracheal compression before and after surgical correction. Ann Biomed Eng 48:822–833. https://doi.org/10.1007/s10439-019-02410-1
Morita K, Maeda K, Yabe K, Oshima Y (2017) Management of congenital tracheal stenosis in the neonatal period. Pediatr Surg Int 33:1059–1063. https://doi.org/10.1007/s00383-017-4137-9
Motoyama EK, Finder JD (2016) Respiratory physiology. In: Davis PJ, Cladis FP (eds) Smith’s anesthesia for infants and children, 9th edn. Elsevier, Philadelphia, pp 23–72
Sharma A, Ford S, Calvert J (2008) Adaptation for life: a review of neonatal physiology. Anaesth Intensive Care 9:93–98. https://doi.org/10.1016/j.mpaic.2008.01.009
Cantrell JR, Guild HG (1964) Congenital stenosis of the trachea. Am J Surg 108:297–305. https://doi.org/10.1016/0002-9610(64)90023-6
Brouns M, Jayaraju ST, Lacor C, De Mey J, Noppen M, Vincken W, Verbanck S (2007) Tracheal stenosis: a flow dynamics study. J Appl Physiol 102:1178–1184. https://doi.org/10.1152/japplphysiol.01063.2006
Bates AJ, Cetto R, Doorly DJ, Schroter RC, Tolley NS, Comerford A (2016) The effects of curvature and constriction on airflow and energy loss in pathological tracheas. Respir Physiol Neurobiol 234:69–78. https://doi.org/10.1016/j.resp.2016.09.002
Acknowledgements
Partial financial support was received from JSPS KAKENHI Grant Numbers JP19H01175, and JP20H04504. The authors thank Ms. Shiori Kageyama and Ms. Kao Taniguchi for their assistance in the preparation of this work.
Funding
Partial financial support was received from JSPS KAKENHI Grant Numbers JP19H01175, and JP20H04504.
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, formal analysis, investigation, and writing: KM, NT; supervision: SW, TH.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study has been approved by the Institutional ethics committee (approval number: R30-12) and performed in line with the principles of the Declaration of Helsinki.
Consent to participate and consent to publish
This study was open to the public and guaranteed a refusal to cooperate; the data were anonymous, and the need for a separate informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morita, K., Takeishi, N., Wada, S. et al. Computational fluid dynamics assessment of congenital tracheal stenosis. Pediatr Surg Int 38, 1769–1776 (2022). https://doi.org/10.1007/s00383-022-05228-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05228-6