Abstract
Purpose
We aimed to identify factors that affect the time to diagnosis in pediatric brain tumors and investigate the effect of time to diagnosis on clinical outcome.
Methods
A retrospective study of children with brain tumors aged less than 18 years diagnosed at the University of Tsukuba Hospital over a period of 7 years was conducted.
Results
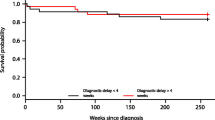
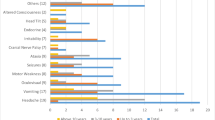
Eighty-five consecutive patients, with a mean age of 9.1 years, were included in the study. The median interval from symptom onset to diagnosis was 45 days (range 0–1673); median interval from symptom onset to first presentation was 31.0 days; and median interval from first presentation to diagnosis was 13.5 days. Germinoma had the longest interval from symptom onset to first presentation, and from first presentation to diagnosis. Patients presenting with endocrine disorder had a significantly longer interval from symptom onset to first presentation (p = 0.019); those with visual disturbance (p = 0.016) or endocrine disorder (p = 0.030) had significantly longer intervals from first presentation to diagnosis.
Conclusion
Pediatric brain tumor patients with germinoma and presenting symptoms of endocrine disorder or visual disturbance have a longer time to diagnosis. Although improved prognosis is not clearly related to a shorter time to diagnosis, we believe that early diagnosis can lead to improved treatment and better quality of life. A detailed medical history and neuroimaging studies at the earliest time possible are important for early diagnosis.

Similar content being viewed by others
References
Abdelkhalek ER, Sherief LM, Kamal NM, Soliman RM (2014) Factors associated with delayed cancer diagnosis in Egyptian children. Clin Med Insights Pediatr 8:CMPed.S16413–6. https://doi.org/10.4137/CMPed.S16413
Aggarwal A, Herz N, Campbell P, Arkush L, Short S, Rees J (2015) Diagnostic delay and survival in high-grade gliomas - evidence of the ‘waiting time paradox’? Br J Neurosurg 29:520–523. https://doi.org/10.3109/02688697.2015.1012050
Ahrensberg JM, Olesen F, Hansen RP, Schrøder H, Vedsted P (2013) Childhood cancer and factors related to prolonged diagnostic intervals: a Danish population-based study. Br J Cancer 108:1280–1287. https://doi.org/10.1038/bjc.2013.88
Arnautovic A, Billups C, Broniscer A, Gajjar A, Boop F, Qaddoumi I (2015) Delayed diagnosis of childhood low-grade glioma: causes, consequences, and potential solutions. Childs Nerv Syst 31:1067–1077. https://doi.org/10.1007/s00381-015-2670-1
Azizi AA, Heßler K, Leiss U, Grylli C, Chocholous M, Peyrl A, Gojo J, Slavc I (2017) From symptom to diagnosis—the prediagnostic symptomatic interval of pediatric central nervous system tumors in Austria. Pediatr Neurol 76:27–36. https://doi.org/10.1016/j.pediatrneurol.2017.08.006
Brown BJ, James BO, Ajayi SO, Ogun OA, Oladokun RE (2009) Factors influencing time to diagnosis of childhood cancer in Ibadan, Nigeria. Afr Health Sci 9:247–253
Dang-Tan T, Franco EL (2007) Diagnosis delays in childhood cancer: a review. Cancer 110:703–713. https://doi.org/10.1002/cncr.22849
Dang-Tan T, Trottier H, Mery LS, Morrison HI, Barr RD, Greenberg ML, Franco EL (2008) Delays in diagnosis and treatment among children and adolescents with cancer in Canada. Pediatr Blood Cancer 51:468–474. https://doi.org/10.1002/pbc.21600
Halperin EC, Friedman HS (1996) Is there a correlation between duration of presenting symptoms and stage of medulloblastoma at the time of diagnosis? Cancer 78:874–880. https://doi.org/10.1002/(SICI)1097-0142(19960815)78:4<874::AID-CNCR26>3.0.CO;2-R
Molineus A, Boxberger N, Redlich A, Vorwerk P (2013) Time to diagnosis of brain tumors in children: a single-centre experience. Pediatr Int 55:305–309. https://doi.org/10.1111/ped.12095
Nakajima Y, Yamada K, Imamura K, Kobayashi K (2008) Radiologist supply and workload: international comparison. Radiat Med 26:455–465. https://doi.org/10.1007/s11604-008-0259-2
Neal RD (2009) Do diagnostic delays in cancer matter & quest. Br J Cancer 101:S9–S12. https://doi.org/10.1038/sj.bjc.6605384
Patel V, McNinch NL, Rush S (2019) Diagnostic delay and morbidity of central nervous system tumors in children and young adults: a pediatric hospital experience. J Neuro-Oncol 143:1–8. https://doi.org/10.1007/s11060-019-03160-9
Phi JH, Kim S-K, Lee YA, Shin CH, Cheon J-E, Kim I-O, Yang SW, Wang K-C (2013) Latency of intracranial germ cell tumors and diagnosis delay. Childs Nerv Syst 29:1871–1881. https://doi.org/10.1007/s00381-013-2164-y
Shay V, Fattal-Valevski A, Beni-Adani L, Constantini S (2011) Diagnostic delay of pediatric brain tumors in Israel: a retrospective risk factor analysis. Childs Nerv Syst 28:93–100. https://doi.org/10.1007/s00381-011-1564-0
Shibui S (2012) The present status and trend of brain tumors based on the data of the brain tumor registry of Japan. Brain Nerve 64:286–290
Stocco C, Pilotto C, Passone E, Nocerino A, Tosolini R, Pusiol A, Cogo P (2017) Presentation and symptom interval in children with central nervous system tumors. A single-center experience. Childs Nerv Syst 33:1–8. https://doi.org/10.1007/s00381-017-3572-1
Ueoka DI, Nogueira J, Campos JC, Filho PM, Ferman S, Lima MA (2009) Brainstem gliomas—retrospective analysis of 86 patients. J Neurol Sci 281:20–23. https://doi.org/10.1016/j.jns.2009.03.009
Vasquez L, Oscanoa M, Tello M, Tapia E, Maza I, Geronimo J (2016) Factors associated with the latency to diagnosis of childhood cancer in Peru. Pediatr Blood Cancer 63:1959–1965. https://doi.org/10.1002/pbc.26134
Wilne S, Collier J, Kennedy C, Koller K, Grundy R, Walker D (2007) Presentation of childhood CNS tumours: a systematic review and meta-analysis. Lancet Oncol 8:685–695. https://doi.org/10.1016/S1470-2045(07)70207-3
Zhang Y, Deng K, Zhu H, Lu L, Pan H, Ma W, Wang R, Yao Y (2019) Delays in diagnosis of pediatric histologically confirmed sellar germ cell tumors in China: a retrospective risk factor analysis. World Neurosurg 122:e472–e479. https://doi.org/10.1016/j.wneu.2018.10.082
Acknowledgments
We thank Enago for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
The study was approved by the Ethics Committee of the University of Tsukuba Hospital.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirata, K., Muroi, A., Tsurubuchi, T. et al. Time to diagnosis and clinical characteristics in pediatric brain tumor patients. Childs Nerv Syst 36, 2047–2054 (2020). https://doi.org/10.1007/s00381-020-04573-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04573-y