Abstract
Objectives
To analyze the impact of surgeon’s experience on surgical margin status, postoperative continence and operative time after radical prostatectomy (RP) in a surgeon who performed more than 2000 open RP.
Patients and methods
We retrospectively analyzed 2269 patients who underwent RP by one surgeon from April 2004 to June 2012. Multivariable logistic models were used to quantify the impact of surgeon’s experience (measured by the number of prior performed RP) on surgical margin status, postoperative continence and operative time.
Results
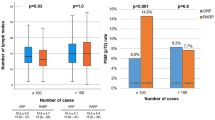
Negative surgical margin rate was 86 % for patients with pT2 stage, and continence rate at 3 years after RP was 94 %. Patients with negative surgical margin had lower preoperative PSA level (p = 0.02), lower pT stage (p < 0.001) and lower Gleason score (p < 0.001). The influence of the experience of the surgeon was nonlinear, positive and highly significant up to 750 performed surgeries (75–90 % negative surgical margin) (p < 0.01). The probability of continence rises significantly with surgeon’s experience (from 88–96 %) (p < 0.05). A reduction in operative time (90–65 min) per RP was observed up to 1000 RP.
Conclusions
In the present study, we showed evidence that surgeon’s experience has a strong positive impact on pathologic and functional outcomes as well as on operative time. While significant learning effects concerning positive surgical margin rate and preserved long-term continence were detectable during the first 750 and 300 procedures, respectively, improvement in operative time was detectable up to a threshold of almost 1000 RP and hence is relevant even for very high-volume surgeons.



Similar content being viewed by others
References
Guillonneau BD, Fizazi K (2011) Natural history of patients presenting biochemical recurrence after radical prostatectomy: some good news? Eur Urol 59:900–901
Simmons MN, Stephenson AJ, Klein EA (2007) Natural history of biochemical recurrence after radical prostatectomy: risk assessment for secondary therapy. Eur Urol 51:1175–1184
Boorjian SA, Thompson RH, Tollefson MK et al (2011) Long-term risk of clinical progression after biochemical recurrence following radical prostatectomy: the impact of time from surgery to recurrence. Eur Urol 59:893–899
Herrell SD, Smith JA Jr (2005) Robotic-assisted laparoscopic prostatectomy: What is the learning curve? Urology 66:105–107
Artibani W, Novara G (2008) Cancer-related outcome and learning curve in retropubic radical prostatectomy: “if you need an operation, the most important step is to choose the right surgeon”. Eur Urol 53:874–876
Begg CB, Riedel ER, Bach PB et al (2002) Variations in morbidity after radical prostatectomy. N Engl J Med 346:1138–1144
Hu JC, Gold KF, Pashos CL et al (2003) Role of surgeon volume in radical prostatectomy outcomes. J Clin Oncol 21:401–405
Bianco FJ Jr, Riedel ER, Begg CB et al (2005) Variations among high volume surgeons in the rate of complications after radical prostatectomy: further evidence that technique matters. J Urol 173:2099–2103
Vickers AJ, Bianco FJ, Serio AM et al (2007) The surgical learning curve for prostate cancer control after radical prostatectomy. J Natl Cancer Inst 99:1171–1177
Vickers A, Bianco F, Cronin A et al (2010) The learning curve for surgical margins after open radical prostatectomy: implications for margin status as an oncological end point. J Urol 183:1360–1365
Trinh QD, Bjartell A, Freedland SJ et al (2013) A systematic review of the volume-outcome relationship for radical prostatectomy. Eur Urol 64:786–798
Vickers AJ, Savage CJ, Hruza M et al (2009) The surgical learning curve for laparoscopic radical prostatectomy: a retrospective cohort study. Lancet Oncol 10:475–480
Wallerstedt A, Tyritzis SI, Thorsteinsdottir T et al (2014) Short-term results after robot-assisted laparoscopic radical prostatectomy compared to open radical prostatectomy. Eur Urol 67:660–670
Vesey SG, McCabe JE, Hounsome L et al (2012) UK radical prostatectomy outcomes and surgeon case volume: based on an analysis of the British Association of Urological Surgeons Complex Operations Database. BJU Int 109:346–354
Chun FK, Briganti A, Antebi E et al (2006) Surgical volume is related to the rate of positive surgical margins at radical prostatectomy in European patients. BJU Int 98:1204–1209
Secin FP, Savage C, Abbou C et al (2010) The learning curve for laparoscopic radical prostatectomy: an international multicenter study. J Urol 184:2291–2296
Van Poppel H, Collette L, Kirkali Z et al (2001) Quality control of radical prostatectomy: a feasibility study. Eur J Cancer 37:884–891
Ellison LM, Heaney JA, Birkmeyer JD (2000) The effect of hospital volume on mortality and resource use after radical prostatectomy. J Urol 163:867–869
Yao SL, Lu-Yao G (1999) Population-based study of relationships between hospital volume of prostatectomies, patient outcomes, and length of hospital stay. J Natl Cancer Inst 91:1950–1956
Eastham JA, Kattan MW, Riedel E et al (2003) Variations among individual surgeons in the rate of positive surgical margins in radical prostatectomy specimens. J Urol 170:2292–2295
Peyromaure M, Ravery V, Boccon-Gibod L (2002) The management of stress urinary incontinence after radical prostatectomy. BJU Int 90:155–161
Mettlin CJ, Murphy GP, Sylvester J et al (1997) Results of hospital cancer registry surveys by the American College of Surgeons: outcomes of prostate cancer treatment by radical prostatectomy. Cancer 80:1875–1881
Catalona WJ, Basler JW (1993) Return of erections and urinary continence following nerve sparing radical retropubic prostatectomy. J Urol 150:905–907
Hautmann RE, Sauter TW, Wenderoth UK (1994) Radical retropubic prostatectomy: morbidity and urinary continence in 418 consecutive cases. Urology 43:47–51
Abdollah F, Sun M, Suardi N et al (2013) A novel tool to assess the risk of urinary incontinence after nerve-sparing radical prostatectomy. BJU Int 111:905–913
Nuttall M, Cathcart P, van der Meulen J et al (2005) A description of radical nephrectomy practice and outcomes in England: 1995–2002. BJU Int 96:58–61
Bennette C, Vickers A (2012) Against quantiles: categorization of continuous variables in epidemiologic research, and its discontents. BMC Med Res Methodol 12:21
Vickers AJ, Cronin AM, Masterson TA et al (2010) How do you tell whether a change in surgical technique leads to a change in outcome? J Urol 183:1510–1514
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
All patients gave their informed consent prior to data collection. The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Alexander Kretschmer and Philipp Mandel have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kretschmer, A., Mandel, P., Buchner, A. et al. Surgical learning curve for open radical prostatectomy: Is there an end to the learning curve?. World J Urol 33, 1721–1727 (2015). https://doi.org/10.1007/s00345-015-1540-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1540-5