Abstract
Objective
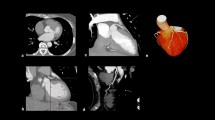
The current study aimed to explore a deep convolutional neural network (DCNN) model that integrates multidimensional CMR data to accurately identify LV paradoxical pulsation after reperfusion by primary percutaneous coronary intervention with isolated anterior infarction.
Methods
A total of 401 participants (311 patients and 90 age-matched volunteers) were recruited for this prospective study. The two-dimensional UNet segmentation model of the LV and classification model for identifying paradoxical pulsation were established using the DCNN model. Features of 2- and 3-chamber images were extracted with 2-dimensional (2D) and 3D ResNets with masks generated by a segmentation model. Next, the accuracy of the segmentation model was evaluated using the Dice score and classification model by receiver operating characteristic (ROC) curve and confusion matrix. The areas under the ROC curve (AUCs) of the physicians in training and DCNN models were compared using the DeLong method.
Results
The DCNN model showed that the AUCs for the detection of paradoxical pulsation were 0.97, 0.91, and 0.83 in the training, internal, and external testing cohorts, respectively (p < 0.001). The 2.5-dimensional model established using the end-systolic and end-diastolic images combined with 2-chamber and 3-chamber images was more efficient than the 3D model. The discrimination performance of the DCNN model was better than that of physicians in training (p < 0.05).
Conclusions
Compared to the model trained by 2-chamber or 3-chamber images alone or 3D multiview, our 2.5D multiview model can combine the information of 2-chamber and 3-chamber more efficiently and obtain the highest diagnostic sensitivity.
Clinical relevance statement
A deep convolutional neural network model that integrates 2-chamber and 3-chamber CMR images can identify LV paradoxical pulsation which correlates with LV thrombosis, heart failure, ventricular tachycardia after reperfusion by primary percutaneous coronary intervention with isolated anterior infarction.
Key Points
• The epicardial segmentation model was established using the 2D UNet based on end-diastole 2- and 3-chamber cine images.
• The DCNN model proposed in this study had better performance for discriminating LV paradoxical pulsation accurately and objectively using CMR cine images after anterior AMI compared to the diagnosis of physicians in training.
• The 2.5-dimensional multiview model combined the information of 2- and 3-chamber efficiently and obtained the highest diagnostic sensitivity.





Similar content being viewed by others
Abbreviations
- 2D UNet:
-
Two-dimensional UNet
- AMI:
-
Acute myocardial infarction
- BNPmax :
-
Peak brain natriuretic peptide
- CK-MBmax :
-
Peak creatinine kinase-MB
- CMR:
-
Cardiac magnetic resonance
- CRPmax :
-
Peak C-creative protein
- cTnImax :
-
Peak troponin I
- DCNN:
-
Deep convolutional neural network
- HF:
-
Heart failure
- IMH:
-
Intramyocardial hemorrhage
- LAD:
-
Left anterior descending
- LGE:
-
Late Gadolinium enhancement
- LVEF:
-
Left ventricular ejection fraction
- LVT:
-
Left ventricular thrombosis
- MVO:
-
Microvascular obstruction
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- SSFP:
-
Steady-state free-precession
- T2WI-STIR:
-
T2-weighted short-tau triple inversion recovery
References
Kidambi A, Motwani M, Uddin A et al (2017) Myocardial extracellular volume estimation by CMR predicts functional recovery following acute MI. JACC Cardiovasc Imaging 10:989–999
D’Elia N, D’Hooge J, Marwick TH (2015) Association between myocardial mechanics and ischemic LV remodeling. JACC Cardiovasc Imaging 8:1430–1443
Cabin HS, Roberts WC (1980) Left ventricular aneurysm, intraaneurysmal thrombus and systemic embolus in coronary heart disease. Chest 77:586–590
Konen E, Merchant N, Gutierrez C et al (2005) True versus false left ventricular aneurysm: differentiation with MR imaging–initial experience. Radiology 236:65–70
Meizlish J, Berger H, Plankey M, Errico D, Levy W, Zaret B (1984) Functional left ventricular aneurysm formation after acute anterior transmural myocardial infarction. Incidence, natural history, and prognostic implications. N Engl J Med 311:1001–1006
Shen W, Tribouilloy C, Mirode A, Dufossé H, Lesbre J (1992) Left ventricular aneurysm and prognosis in patients with first acute transmural anterior myocardial infarction and isolated left anterior descending artery disease. Eur Heart J 13:39–44
Heatlie GJ, Mohiaddin R (2005) Left ventricular aneurysm: comprehensive assessment of morphology, structure and thrombus using cardiovascular magnetic resonance. Clin Radiol 60:687–692
Lam C, Gale H, Drake E (1964) Surgical treatment of left ventricular aneurysms. JAMA 187:1-3
Matsumoto M, Watanabe F, Goto A et al (1985) Left ventricular aneurysm and the prediction of left ventricular enlargement studied by two-dimensional echocardiography: quantitative assessment of aneurysm size in relation to clinical course. Circulation 72:280–286
Zhou H, Li L, Liu Z et al (2021) Deep learning algorithm to improve hypertrophic cardiomyopathy mutation prediction using cardiac cine images. Eur Radiol 31:3931–3940
Montalt-Tordera J, Quail M, Steeden JA, Muthurangu V (2021) Reducing contrast agent dose in cardiovascular MR angiography with deep learning. J Magn Reson Imaging 54:795–805
Hamilton JI, Currey D, Rajagopalan S, Seiberlich N (2021) Deep learning reconstruction for cardiac magnetic resonance fingerprinting T1 and T2 map**. Magn Reson Med 85:2127–2135
Ghadimi S, Auger DA, Feng X et al (2021) Fully-automated global and segmental strain analysis of DENSE cardiovascular magnetic resonance using deep learning for segmentation and phase unwrap**. J Cardiovasc Magn Reson 23:20
Duan J, Bello G, Schlemper J et al (2019) Automatic 3D bi-ventricular segmentation of cardiac images by a shape-refined multi-task deep learning approach. IEEE Trans Med Imaging. https://doi.org/10.1109/TMI.2019.2894322
Litjens G, Ciompi F, Wolterink JM et al (2019) State-of-the-art deep learning in cardiovascular image analysis. JACC Cardiovasc Imaging 12:1549–1565
Chen C, Qin C, Qiu H et al (2020) Deep learning for cardiac image segmentation: a review. Front Cardiovasc Med 7:25
Martini N, Aimo A, Barison A et al (2020) Deep learning to diagnose cardiac amyloidosis from cardiovascular magnetic resonance. J Cardiovasc Magn Reson 22:84
Goldfarb JW, Craft J, Cao JJ (2019) Water-fat separation and parameter map** in cardiac MRI via deep learning with a convolutional neural network. J Magn Reson Imaging. https://doi.org/10.1002/jmri.26658
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521:436–444
Thygesen K, Alpert JS, Jaffe AS et al (2018) Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 72:2231–2264
Douglas PZ, Peter L, Robert OB, Douglas LM, Gordon FT, Eugene B (2018) Braunwald’s heart disease: a textbook of cardiovascular medicine, 11th Edition. Elsevier, Canada. BMH Med J:3067–3069
Joyce E, Hoogslag GE, Leong DP et al (2014) Association between left ventricular global longitudinal strain and adverse left ventricular dilatation after ST-segment-elevation myocardial infarction. Circ Cardiovasc Imaging 7:74–81
Geras KJ, Wolfson S, Shen Y et al (2017) High-resolution breast cancer screening with multiview deep convolutional neural networks. ar**v preprint ar**v:1703.07047. https://arxiv.org/abs/1703.07047. Accessed 19 June 2023
Juarez-Orozco LE, Martinez-Manzanera O, van der Zant FM, Knol RJJ, Knuuti J (2020) Deep learning in quantitative PET myocardial perfusion imaging: a study on cardiovascular event prediction. JACC Cardiovasc Imaging 13:180–182
Mehta RH, Harjai KJ, Cox D et al (2003) Clinical and angiographic correlates and outcomes of suboptimal coronary flow inpatients with acute myocardial infarction undergoing primary percutaneous coronary intervention. J Am Coll Cardiol 42:1739–1746
Writing Group M, Mozaffarian D, Benjamin EJ et al (2016) Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 133:e38-360
Gupta KB, Ratcliffe MB, Fallert MA, Edmunds LH Jr, Bogen DK (1994) Changes in passive mechanical stiffness of myocardial tissue with aneurysm formation. Circulation 89:2315–2326
Goldberg RJ, Konstam MA (1999) Assessing the population burden from heart failure: need for sentinel population-based surveillance systems. Arch Intern Med 159:15–17
Shah AM, Solomon SD (2010) A unified view of ventricular remodelling. Eur J Heart Fail 12:779–781
Pezel T, Viallon M, Croisille P et al (2021) Imaging Interstitial fibrosis, left ventricular remodeling, and function in stage A and B heart failure. JACC Cardiovasc Imaging 14:1038–1052
Tao Q, Yan W, Wang Y et al (2019) Deep learning-based method for fully automatic quantification of left ventricle function from cine mr images: a multivendor, multicenter study. Radiology 290:81–88
Zhang N, Yang G, Gao Z et al (2019) Deep learning for diagnosis of chronic myocardial infarction on nonenhanced cardiac Cine MRI. Radiology 291:606–617
Kusunose K, Abe T, Haga A et al (2020) A deep learning approach for assessment of regional wall motion abnormality from echocardiographic images. JACC Cardiovasc Imaging 13:374–381
Pandey A, Kagiyama N, Yanamala N et al (2021) Deep-Learning models for the echocardiographic assessment of diastolic dysfunction. JACC Cardiovasc Imaging 14:1887–1900
Heras M, Sanz G, Betriu A, Mont L, de Flores T, Navarro-López F (1990) Does left ventricular aneurysm influence survival after acute myocardial infarction? Eur Heart J 11:441–446
Gong FF, Vaitenas I, Malaisrie SC, Maganti K (2021) Mechanical complications of acute myocardial infarction: a review. JAMA Cardiol 6:341–349
Acknowledgements
We are very grateful to the Philips Healthcare team for their support in image analysis and deep learning methods. We appreciate the support of Yan Zhou in providing a research platform for this study. We appreciate Jun Pu and Meng Jiang made a great contribution to the study, mainly including patient recruitment, baseline clinical data collection, diagnosis, and standardized treatment.
Funding
Supported by National Natural Science Foundation of China (No. 81873886, 81873887, and 82171884); National Natural Science Foundation of China Youth project (No. 82101981); Shanghai Science and Technology Innovation Action Plan, Technology Standard Project Grant numbers (No. 19DZ2203800); Shanghai Science and technology innovation action plan, technology standard project (No. 19DZ2203800); Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant: Shanghai Jiao Tong University school of medicine Double hundred outstanding person project (No. 20191904); Shanghai Jiao Tong University Medical Engineering Cross Project (No. YG2022QN016).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Lian-Ming Wu.
Conflict of interest
The authors state that there neither exists a conflict of interest nor that there is financial information to disclose.
Statistics and biometry
Lian-Ming Wu kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all participants in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Study subjects or cohorts have not been previously reported.
Methodology
• Prospective
• Observational
• Multicentre study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, BH., Wu, CW., An, DA. et al. A deep learning method for the automated assessment of paradoxical pulsation after myocardial infarction using multicenter cardiac MRI data. Eur Radiol 33, 8477–8487 (2023). https://doi.org/10.1007/s00330-023-09807-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09807-6