Abstract
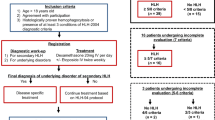
To investigate the efficacy of the doxorubicin-etoposide-methylprednisolone, DEP) regimen as an effective treatment for adult Hemophagocytic Lymphohistiocytosis secondary to rheumatic disease and analyze prognosis in these patients. Fifty-eight adult patients diagnosed with Hemophagocytic Lymphohistiocytosis secondary to rheumatic disease admitted to Bei**g Friendship Hospital from 1st Jan. 2018 to 31st Dec. 2022 were retrospectively included in this study. Patients were grouped according to previous treatment. Clinical data and laboratory characteristics of patients were retrospectively analyzed. The efficacy was evaluated every 2 weeks after initiating the first course of the DEP regimen and until the last inpatient or 31st Dec. 2023. 26 patients were included in Group A and 32 patients were included in Group B due to the previous treatment. After the first course of the DEP regimen, the overall response rate of all patients was 82.8%, with 13.8% in complete response and 69% in partial response. There was no significant statistical objective response rate between the two groups after the DEP regimen, except at 2-week. Serum ferritin, sCD25, ALT, AST, and DBIL concentrations were significantly lower at 2, 4 and 6-week than pre-treatment (P < 0.05). The overall mortality rate is 20.7% (12/58). Importantly, advanced age, initial level of HB and PLT, and central nervous system (CNS) involvement were independent poor risk factors affecting OS in bivariate analysis. The DEP regimen is effective for adult HLH secondary rheumatic disease with a high overall rate and accepted side effects.




Similar content being viewed by others
Data availability
No datasets were generated or analyzed during the current study.
References
Ramos-Casals M, Brito-Zerón P, López-Guillermo A, Khamashta MA, Bosch X (2014) Adult haemophagocytic syndrome. Lancet 383:1503–1516
Stéphan JL, Koné-Paut I, Galambrun C, Mouy R, Bader-Meunier B, Prieur AM (2001) Reactive haemophagocytic syndrome in children with inflammatory disorders. A retrospective study of 24 patients. Rheumatology (Oxford). 40:1285–92
Sawhney S, Woo P, Murray KJ (2001) Macrophage activation syndrome: a potentially fatal complication of rheumatic disorders. Arch Dis Child 85:421–426
Schulert GS, Grom AA (2014) Macrophage activation syndrome and cytokine-directed therapies. Best Pract Res Clin Rheumatol 28:277–292
Ravelli A, Minoia F, Davì S, Horne A, Bovis F, Pistorio A et al (2016) 2016 Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative. Arthritis Rheumatol 68:566–576
Batu ED, Erden A, Seyhoğlu E, Kilic L, Büyükasık Y, Karadag O et al (2017) Assessment of the HScore for reactive haemophagocytic syndrome in patients with rheumatic diseases. Scand J Rheumatol 46:44–48
Zou LX, Zhu Y, Sun L, Ma HH, Yang SR, Zeng HS et al (2020) Clinical and laboratory features, treatment, and outcomes of macrophage activation syndrome in 80 children: a multi-center study in China. World J Pediatr 16:89–98
Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S et al (2007) HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 48:124–131
Henderson LA, Cron RQ (2020) Macrophage Activation Syndrome and Secondary Hemophagocytic Lymphohistiocytosis in Childhood Inflammatory Disorders: Diagnosis and Management. Paediatr Drugs 22:29–44
Fukaya S, Yasuda S, Hashimoto T, Oku K, Kataoka H, Horita T et al (2008) Clinical features of haemophagocytic syndrome in patients with systemic autoimmune diseases: analysis of 30 cases. Rheumatology (Oxford) 47:1686–1691
Wang Y, Huang W, Hu L, Cen X, Li L, Wang J et al (2015) Multicenter study of combination DEP regimen as a salvage therapy for adult refractory hemophagocytic lymphohistiocytosis. Blood 126:2186–2192
Marsh RA, Allen CE, Mcclain KL, Weinstein JL, Kanter J, Skiles J et al (2013) Salvage therapy of refractory hemophagocytic lymphohistiocytosis with alemtuzumab. Pediatr Blood Cancer 60:101–109
Horne A, Wickström R, Jordan MB, Yeh EA, Naqvi A, Henter JI et al (2017) How to Treat Involvement of the Central Nervous System in Hemophagocytic Lymphohistiocytosis? Curr Treat Options Neurol 19:3
La Rosée P, Horne A, Hines M, von Bahr GT, Machowicz R, Berliner N et al (2019) Recommendations for the management of hemophagocytic lymphohistiocytosis in adults. Blood 133:2465–2477
Luedke CE, Cerami A (1990) Interferon-gamma overcomes glucocorticoid suppression of cachectin/tumor necrosis factor biosynthesis by murine macrophages. J Clin Invest 86:1234–1240
Gavand PE, Serio I, Arnaud L, Costedoat-Chalumeau N, Carvelli J, Dossier A et al (2017) Clinical spectrum and therapeutic management of systemic lupus erythematosus-associated macrophage activation syndrome: A study of 103 episodes in 89 adult patients. Autoimmun Rev 16:743–749
Wang Y, Huang W, Hu L, Cen X, Li L, Wang J et al (2015) Multicenter study of combination DEP regimen as a salvage therapy for adult refractory hemophagocytic lymphohistiocytosis. Blood 126:2186–2192
Wang J, Zhang R, Wu X, Li F, Yang H, Liu L et al (2021) Ruxolitinib-combined doxorubicin-etoposide-methylprednisolone regimen as a salvage therapy for refractory/relapsed haemophagocytic lymphohistiocytosis: a single-arm, multicentre, phase 2 trial. Br J Haematol 193:761–768
Crayne CB, Albeituni S, Nichols KE, Cron RQ (2019) The Immunology of Macrophage Activation Syndrome. Front Immunol 10:119
Carter SJ, Tattersall RS, Ramanan AV (2019) Macrophage activation syndrome in adults: recent advances in pathophysiology, diagnosis and treatment. Rheumatology (Oxford) 58:5–17
Huwyler J, Drewe J, Krähenbuhl S (2008) Tumor targeting using liposomal antineoplastic drugs. Int J Nanomedicine 3:21–29
He L, ** Z, Liu M, Zhang R, Wang Z, Wang Y (2022) Effectiveness of a modified doxorubicin-etoposide-methylprednisolone regimen for the treatment of refractory or relapsed macrophage activation syndrome in adults. Pol Arch Intern Med 132:16226
Johnson TS, Terrell CE, Millen SH, Katz JD, Hildeman DA, Jordan MB (2014) Etoposide selectively ablates activated T cells to control the immunoregulatory disorder hemophagocytic lymphohistiocytosis. J Immunol 192:84–91
He L, Yao S, Zhang R, Liu M, Hua Z, Zou H et al (2022) Macrophage activation syndrome in adults: Characteristics, outcomes, and therapeutic effectiveness of etoposide-based regimen. Front Immunol 13:955523
Horne A, von Bahr GT, Chiang S, Meeths M, Björklund C, Ekelund M et al (2021) Efficacy of moderately dosed etoposide in macrophage activation syndrome-hemophagocytic lymphohistiocytosis. J Rheumatol 48:1596–1602
Vilaiyuk S, Sirachainan N, Wanitkun S, Pirojsakul K, Vaewpanich J (2013) Recurrent macrophage activation syndrome as the primary manifestation in systemic lupus erythematosus and the benefit of serial ferritin measurements: a case-based review. Clin Rheumatol 32:899–904
Komp DM, Mcnamara J, Buckley P (1989) Elevated soluble interleukin-2 receptor in childhood hemophagocytic histiocytic syndromes. Blood 73:2128–2132
He L, ** Z, Liu M, Zhang R, Wang Z, Wang Y (2022) Effectiveness of a modified doxorubicin-etoposide-methylprednisolone regimen for the treatment of refractory or relapsed macrophage activation syndrome in adults. Pol Arch Intern Med 132
Carter SJ, Tattersall RS, Ramanan AV (2019) Macrophage activation syndrome in adults: recent advances in pathophysiology, diagnosis and treatment. Rheumatology (Oxford) 58:5–17
Yoon JH, Park SS, Jeon YW, Lee SE, Cho BS, Eom KS et al (2019) Treatment outcomes and prognostic factors in adult patients with secondary hemophagocytic lymphohistiocytosis not associated with malignancy. Haematologica 104:269–276
Funding
This work was supported by the National Natural Science Foundation of China (82370185) and the Key Scientific Project for Capital’s Health Development Research (2020–1-2022).
Author information
Authors and Affiliations
Contributions
ZW and JSW contributed to the design of the study. DFY conducted the data analysis and wrote the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key messages
1. The DEP regimen is an effective treatment for adult Hemophagocytic Lymphohistiocytosis secondary to rheumatic disease, even patients who exhibited refractory or relapse could achieve remission.
2. The advanced age, baseline level of HB and PLT, and CNS involvement correlated with poor overall survival and progression free survival in MAS.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yin, D., Wang, J. & Wang, Z. The effectiveness of the doxorubicin-etoposide-methylprednisolone regimen for adult HLH secondary to rheumatic disease. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05796-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05796-8