Abstract
Background
Literature on 30-day readmission in adults with sickle cell disease (SCD) is limited. This study examined the overall and age-stratified rates, risk factors, and healthcare resource utilization associated with 30-day readmission in this population.
Methods
Using the Nationwide Readmissions Database, a retrospective cohort study was conducted to identify adult patients (aged ≥ 18) with SCD in 2016. Patients were stratified by age and followed for 30 days to assess readmission following an index discharge. The primary outcome was 30-day unplanned all-cause readmission. Secondary outcomes included index hospitalization costs and readmission outcomes (e.g., time to readmission, readmission costs, and readmission lengths of stay). Separate generalized linear mixed models estimated the adjusted odds ratios (aORs) for associations of readmission with patient and hospital characteristics, overall and by age.
Results
Of 15,167 adults with SCD, 2,863 (18.9%) experienced readmission. Both the rates and odds of readmission decreased with increasing age. The SCD complications vaso-occlusive crisis and end-stage renal disease (ESRD) were significantly associated with increased likelihood of readmission (p < 0.05). Age-stratified analyses demonstrated that diagnosis of depression significantly increased risk of readmission among patients aged 18-to-29 years (aOR = 1.537, 95%CI: 1.215–1.945) but not among patients of other ages. All secondary outcomes significantly differed by age (p < 0.05).
Conclusion
This study demonstrates that patients with SCD are at very high risk of 30-day readmission and that younger adults and those with vaso-occlusive crisis and ESRD are among those at highest risk. Multifaceted, age-specific interventions targeting individuals with SCD on disease management are needed to prevent readmissions.



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed in this study are not made publicly available based on the data user agreement with the vendor.
References
CDC (2022) Data & Statistics on Sickle Cell Disease. In: Cent. Dis. Control Prev. https://www.cdc.gov/ncbddd/sicklecell/data.html. Accessed 13 Feb 2023
Ataga KI, Orringer EP (2003) Hypercoagulability in sickle cell disease: a curious paradox. Am J Med 115:721–728. https://doi.org/10.1016/j.amjmed.2003.07.011
Ataga KI, Cappellini MD, Rachmilewitz EA (2007) β-Thalassaemia and sickle cell anaemia as paradigms of hypercoagulability. Br J Haematol 139:3–13. https://doi.org/10.1111/j.1365-2141.2007.06740.x
Ataga KI, Key NS (2007) Hypercoagulability in sickle cell disease: new approaches to an old problem. Hematol Am Soc Hematol Educ Program 91–96. doi: https://doi.org/10.1182/asheducation-2007.1.91
Ballas SK, Lusardi M (2005) Hospital readmission for adult acute sickle cell painful episodes: frequency, etiology, and prognostic significance. Am J Hematol 79:17–25. https://doi.org/10.1002/ajh.20336
Characteristics of Inpatient Hospital Stays Involving Sickle Cell Disease, 2000–2016 #251. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb251-Sickle-Cell-Disease-Stays-2016.jsp. Accessed 13 Feb 2023
Brousseau DC, Owens PL, Mosso AL et al (2010) Acute Care Utilization and Rehospitalizations for Sickle Cell Disease. JAMA 303:1288–1294. https://doi.org/10.1001/jama.2010.378
Center for Medicare and Medicaid Services (CMS) (2022) CMS Hospital Readmissions Reduction Program. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program. Accessed 6 Feb 2023
Brodsky MA, Rodeghier M, Sanger M et al (2017) Risk factors for 30-day readmission in adults with sickle cell disease. Am J Med 130:601.e9-601.e15. https://doi.org/10.1016/j.amjmed.2016.12.010
Chen M, Goodin A, **ao H et al (2018) Hospitalization metrics associated with hospital-level variation in inferior vena cava filter utilization for patients with venous thromboembolism in the United States: Implications for quality of care. Vasc Med 23:365–371. https://doi.org/10.1177/1358863X18768685
Leschke J, Panepinto JA, Nimmer M et al (2012) Outpatient follow-up and rehospitalizations for sickle cell disease patients. Pediatr Blood Cancer 58:406–409. https://doi.org/10.1002/pbc.23140
Haywood C, Lanzkron S (2009) The burden of hospital readmissions for patients with sickle cell disease in California and North Carolina: 2004 to 2007. Blood 114:554. https://doi.org/10.1182/blood.V114.22.554.554
Kumar V, Chaudhary N, Achebe MM (2020) Epidemiology and predictors of all-cause 30-Day readmission in patients with sickle cell crisis. Sci Rep 10:2082. https://doi.org/10.1038/s41598-020-58934-3
UpToDate (2023) Red blood cell transfusion in sickle cell disease: Indications and transfusion techniques. https://www.uptodate.com/contents/red-blood-cell-transfusion-in-sickle-cell-disease-indications-and-transfusion-techniques. Accessed 22 June 2023
Nouraie M, Gordeuk VR (2015) Blood transfusion and 30-day readmission rate in adult patients hospitalized with sickle cell disease crisis. Transfusion (Paris) 55:2331–2338. https://doi.org/10.1111/trf.13155
Howard J, Malfroy M, Llewelyn C et al (2013) The transfusion alternatives preoperatively in sickle cell disease (TAPS) study: a randomised, controlled, multicentre clinical trial. Lancet 381:930–938. https://doi.org/10.1016/S0140-6736(12)61726-7
Agency for Healthcare Research and Quality (2018) The HCUP Nationwide Readmissions Database (NRD), 2016. https://www.hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2016.jsp#elements. Accessed 6 Feb 2023
Agency for Healthcare Research and Quality (2022) HCUP-US Cost-to-Charge Ratio for Inpatient Files. https://hcup-us.ahrq.gov/db/ccr/ip-ccr/ip-ccr.jsp. Accessed 24 Apr 2023
Quan H, Sundararajan V, Halfon P et al (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Chen M, Surbhi S, Bailey JE (2022) Association of weight loss with type 2 diabetes remission among adults in medically underserved areas: a retrospective cohort study. Am J Health Promot 36:29–37. https://doi.org/10.1177/08901171211024426
UpToDate (2022) Acute chest syndrome (ACS) in sickle cell disease (adults and children). https://www.uptodate.com/contents/acute-chest-syndrome-acs-in-sickle-cell-disease-adults-and-children. Accessed 16 Feb 2023
Candrilli SD, O’Brien SH, Ware RE et al (2011) Hydroxyurea adherence and associated outcomes among Medicaid enrollees with sickle cell disease. Am J Hematol 86:273–277. https://doi.org/10.1002/ajh.21968
Brandow AM, Panepinto JA (2010) Hydroxyurea use in sickle cell disease: the battle with low prescription rates, poor patient compliance and fears of toxicities. Expert Rev Hematol 3:255–260. https://doi.org/10.1586/ehm.10.22
Blinder MA, Vekeman F, Sasane M et al (2013) Age-related treatment patterns in sickle cell disease patients and the associated sickle cell complications and healthcare costs. Pediatr Blood Cancer 60:828–835. https://doi.org/10.1002/pbc.24459
Nolan VG, Anderson SM, Smeltzer MP et al (2018) Pediatric to adult care co-location transitional model for youth with sickle cell disease. Am J Hematol 93:E30–E32. https://doi.org/10.1002/ajh.24953
Cronin RM, Hankins JS, Byrd J et al (2019) Risk factors for hospitalizations and readmissions among individuals with sickle cell disease: results of a U.S. survey study. Hematology 24:189–198. https://doi.org/10.1080/16078454.2018.1549801
Cronin RM, Yang M, Hankins JS et al (2020) Association between hospital admissions and healthcare provider communication for individuals with sickle cell disease. Hematology 25:229–240. https://doi.org/10.1080/16078454.2020.1780737
Howell KE, Saulsberry-Abate AC, Mathias JG et al (2021) Transition care continuity promotes long-term retention in adult care among young adults with sickle cell disease. Pediatr Blood Cancer 68:e29209. https://doi.org/10.1002/pbc.29209
Desai RJ, Mahesri M, Globe D et al (2020) Clinical outcomes and healthcare utilization in patients with sickle cell disease: a nationwide cohort study of Medicaid beneficiaries. Ann Hematol 99:2497–2505. https://doi.org/10.1007/s00277-020-04233-w
Lobo C, Moura P, Fidlarczyk D et al (2022) Cost analysis of acute care resource utilization among individuals with sickle cell disease in a middle-income country. BMC Health Serv Res 22:42. https://doi.org/10.1186/s12913-021-07461-6
Inoue S, Khan I, Mushtaq R et al (2016) Pain management trend of vaso-occulsive crisis (VOC) at a community hospital emergency department (ED) for patients with sickle cell disease. Ann Hematol 95:221–225. https://doi.org/10.1007/s00277-015-2558-x
Jenerette CM, Brewer C (2010) Health-Related Stigma in Young Adults With Sickle Cell Disease. J Natl Med Assoc 102:1050–1055
Jenerette C, Funk M, Murdaugh C (2005) Sickle cell disease: a stigmatizing condition that may lead to depression. Issues Ment Health Nurs 26:1081–1101. https://doi.org/10.1080/01612840500280745
Cronin RM, Hankins JS, Byrd J et al (2018) Modifying factors of the health belief model associated with missed clinic appointments among individuals with sickle cell disease. Hematology 23:683–691. https://doi.org/10.1080/10245332.2018.1457200
Badawy SM, Cronin RM, Hankins J et al (2018) Patient-centered eHealth interventions for children, adolescents, and adults with sickle cell disease: systematic review. J Med Internet Res 20:e10940. https://doi.org/10.2196/10940
Ataga KI, Kutlar A, Kanter J et al (2017) Crizanlizumab for the prevention of pain crises in sickle cell disease. N Engl J Med 376:429–439. https://doi.org/10.1056/NEJMoa1611770
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ming Chen, Kenneth I. Ataga; Data curation: Ming Chen; Methodology: Ming Chen, Min Zhang, Jim Y. Wan; Formal analysis: Ming Chen; Visualization: Ming Chen; Resources: Ming Chen, Kenneth I. Ataga, Jane S. Hankins, Justin D. Gatwood; Project administration: Ming Chen; Writing—original draft preparation: Ming Chen; Writing—review and editing: Ming Chen, Kenneth I. Ataga, Jane S. Hankins, Justin D. Gatwood, James E. Bailey, Jim Y. Wan, Min Zhang; Supervision: James E. Bailey.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Additional file 1: Table S1.
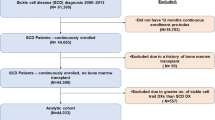
Effect tests of interaction terms between risk factors and age group in adults with SCD. Table S2. Healthcare costs of index hospitalizations in adults with SCD by age group and readmission status (N=15167). Table S3. Subgroup analyses of healthcare costs of index hospitalizations in adults with SCD who had blood transfusion versus no transfusion, by age group and readmission status. Table S4. Subgroup analyses of overall and age-stratified readmission outcomes for adult patients with SCD who had blood transfusion versus no transfusion. Figure S1. Study cohort selection diagram (N=15167). Figure S2. Subgroup analyses of unadjusted and risk-adjusted 30-day readmission rates by age groups in adult patients with SCD who had blood transfusion versus no transfusion. Figure S3. Proportion of adult patients with SCD having vaso-occlusive crisis complicated by acute chest syndrome, or vice versa. (DOCX 257 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, M., Ataga, K.I., Hankins, J.S. et al. Age-related differences in risks and outcomes of 30-day readmission in adults with sickle cell disease. Ann Hematol 102, 2329–2342 (2023). https://doi.org/10.1007/s00277-023-05365-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05365-5