Abstract
Purpose
The present knowledge about lymphatic drainage of the ovary is based on carcinological studies, but it has only rarely been studied under physiological conditions. However, it is one of the preferential routes of dissemination in ovarian cancer, and understanding it is therefore vital for optimal carcinological management.Our purpose was to evaluate the feasibility of an innovative technique to study the lymphatic drainage territories of the ovary using a recirculation module on the cadaveric model.
Methods
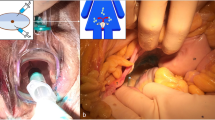
We injected patent blue into the cortex of twenty “revascularised” cadaver ovaries with the Simlife recirculation model. We observed the migration of the dye live and described the drainage territories of each ovary.
Results
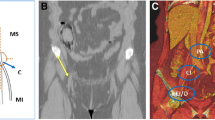
We observed a staining of the lymphatic vessels and migration of the dye in all the subjects, systematically ipsilateral to the injected ovary. We identified a staining of the lumbo-aortic territory in 65% of cases, with a preferential lateral-caval involvement (60%) for the right ovary and lateral-aortic territory (40%) for the left ovary. A common iliac involvement was observed in only 10% of cases. In 57% of cases, the staining of the lumbo-aortic territory was associated with a staining of the suspensory ligament. The pelvic territory was involved in 50% of cases, with an external iliac staining in 25% of cases and internal in 20%.
Conclusion
Our study provides for a better understanding of lymphatic drainage of the ovary using a new detection method, and allows the possibility of improving the teaching for operators with a realistic model. Continuation of this work could lead to considering more targeted and thus less morbid lymph node sampling for lymph node staging in early-stage ovarian cancer.











Similar content being viewed by others
Data availability
The data is stored in a database belonging to the main author.
References
Angelucci M, Corrado G, Mancini E (2016) Laparoscopic indocyanine green sentinel lymph node map** in early ovarian cancer. A pilot study and review of the literature. It J Gynecol Obstet 23–28. https://doi.org/10.14660/2385-0868-56
Benedetti Panici P, Angioli R (2002) Role of lymphadenectomy in ovarian cancer. Best Pract Res Clin Obstet Gynecol 16:529–551. https://doi.org/10.1053/beog.2002.0301
Benedetti-Panici P, Greggi S, Maneschi F, Scambia G, Amoroso M, Rabitti C, Mancuso S (1993) Anatomical and pathological study of retroperitoneal nodes in epithelial ovarian Cancer. Gynecol Oncol 51:150–154. https://doi.org/10.1006/gyno.1993.1263
Cartron G, Leblanc E, Ferron G, Martel P, Narducci F, Querleu D (2005) Complications des lymphadénectomies cœlioscopiques en oncologie gynécologique: 1102 interventions chez 915 patientes. Gynecol Obstet Fertil 33:304–314. https://doi.org/10.1016/j.gyobfe.2005.04.002
Colombo N, Sessa C, du Bois A, Ledermann J, McCluggage WG, McNeish I, Morice P, Pignata S, Ray-Coquard I, Vergote I, Baert T, Belaroussi I, Dashora A, Olbrecht S, Planchamp F, Querleu D, Baert T, Banerjee S, Belaroussi I, Blecharz P, Bruchim I, Cibula D, Colombo N, Concin N, Davidson B, Dashora A, Devouassoux-Shisheboran M, du Bois A, Ferrero A, Glasspool R, González-Martin A, Heinzelmann-Schwarz V, Joly F, Kim JW, Kridelka F, Ledermann J, Lorusso D, Mahner S, McCluggage WG, McNeish I, Mikami M, Mirza MR, Morice P, Nicum S, Olbrecht S, O’Donnell DM, Pautier P, Planchamp F, Pignata S, Querleu D, Ray-Coquard I, Rodolakis A, Sehouli J, Selcukbiricik F, Sessa C, Singh N, Tan DSP, Timmerman D, Tognon G, van der Velden J, Vergote I, Witteveen PO, Zeimet AG (2019) ESMO–ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Ann of Oncol. 30:672–705. https://doi.org/10.1093/annonc/mdz062
Cunéo B, Marcille M. Topographie des ganglions ilio-pelviens. Bull. Mem. Soc. Anat., Paris G (1901) Steinheil, : 653–663
Di Re F, Baiocchi G (2000) Value of lymph node assessment in ovarian cancer: Status of the art at the end of the second millennium. Int J Gynecol Cancer 10:435–442. https://doi.org/10.1046/j.1525-1438.2000.00053.x
Eichner E, Bove ER (1954) In vivo studies on the lymphatic drainage of the human ovary. Obstet Gynecol 3:287–297
Fichez A, Lamblin G, Mathevet P (2007) Lymphadénectomie lombo-aortique cœlioscopique par voie extrapéritonéale gauche: morbidité et apprentissage de la technique. Gynecol Obstet Fertil 35:990–996. https://doi.org/10.1016/j.gyobfe.2007.08.011
Harter P, Gnauert K, Hils R, Lehmann TG, Fisseler-Eckhoff A, Traut A, Bois AD (2007) Pattern and clinical predictors of lymph node metastases in epithelial ovarian cancer. Int J Gynecol Cancer 17. https://doi.org/10.1111/j.1525-1438.2007.00931.x
Harter P, Sehouli J, Lorusso D, Reuss A, Vergote I, Marth C, Kim J-W, Raspagliesi F, Lampe B, Aletti G, Meier W, Cibula D, Mustea A, Mahner S, Runnebaum IB, Schmalfeldt B, Burges A, Kimmig R, Scambia G, Greggi S, Hilpert F, Hasenburg A, Hillemanns P, Giorda G, von Leffern I, Schade-Brittinger C, Wagner U, du Bois A (2019) A Randomized Trial of Lymphadenectomy in patients with Advanced Ovarian neoplasms. N Engl J Med 380:822–832. https://doi.org/10.1056/NEJMoa1808424
Kleppe M, Wang T, Van Gorp T, Slangen BFM, Kruse AJ, Kruitwagen RFPM (2011) Lymph node metastasis in stages I and II ovarian cancer: a review. Gynecol Oncol 123:610–614. https://doi.org/10.1016/j.ygyno.2011.09.013
Kleppe M, Kraima AC, Kruitwagen RFPM, Van Gorp T, Smit NN, van Munsteren JC, DeRuiter MC (2015) Understanding lymphatic drainage pathways of the ovaries to Predict sites for Sentinel nodes in Ovarian Cancer. Int J Gynecol Cancer 25:1405–1414. https://doi.org/10.1097/IGC.0000000000000514
Maggioni A, Benedetti Panici P, Dell’Anna T, Landoni F, Lissoni A, Pellegrino A, Rossi RS, Chiari S, Campagnutta E, Greggi S, Angioli R, Manci N, Calcagno M, Scambia G, Fossati R, Floriani I, Torri V, Grassi R, Mangioni C (2006) Randomised study of systematic lymphadenectomy in patients with epithelial ovarian cancer macroscopically confined to the pelvis. Br J Cancer 95:699–704. https://doi.org/10.1038/sj.bjc.6603323
Mascagni P (1787) Vasorum Lymphaticorum Corporis Humani; Historia E Iconographia. Ex Typographia Pazzini Carli, Senis
Morice P, Joulie F, Camatte S, Atallah D, Rouzier R, Pautier P, Pomel C, Lhommé C, Duvillard P, Castaigne D (2003) Lymph node involvement in epithelial ovarian cancer: analysis of 276 pelvic and paraaortic lymphadenectomies and surgical implications. J Am Coll Surg 197:198–205. https://doi.org/10.1016/S1072-7515(03)00234-5
Musumeci R, Banfi A, Bolis G, Candiani GB, de Palo G, Dire F, Luciani L, Lattuada A, Mangioni C, Mattioli G, Natale N (1977) Lymphangiography in patients with ovarian epithelial cancer.An evaluation of 289 consecutive cases. Cancer 40:1444–1449. https://doi.org/10.1002/1097-0142(197710)40:4%3C1444::AID-CNCR2820400414%3E3.0.CO;2-I
Nam EJ, Yun MJ, Oh YT, Kim JW, Kim JH, Kim S, Jung YW, Kim SW, Kim YT (2010) Diagnosis and staging of primary ovarian cancer: correlation between PET/CT, Doppler US, and CT or MRI. Gynecol Oncol 116:389–394. https://doi.org/10.1016/j.ygyno.2009.10.059
Negishi H, Takeda M, Fujimoto T, Todo Y, Ebina Y, Watari H, Yamamoto R, Minakami H, Sakuragi N (2004) Lymphatic map** and sentinel node identification as related to the primary sites of lymph node metastasis in early stage ovarian cancer. Gynecol Oncol 94:161–166. https://doi.org/10.1016/j.ygyno.2004.04.023
Nyberg RH, Korkola P, Mäenpää JU (2017) Sentinel Node and ovarian tumors: a Series of 20 patients. Int J Gynecol Cancer 27:684–689. https://doi.org/10.1097/IGC.0000000000000948
Onda T, Yoshikawa H, Yokota H, Yasugi T, Taketani Y (1996) Assessment of metastases to aortic and pelvic lymph nodes in epithelial ovarian carcinoma. A proposal for essential sites for lymph node biopsy. Cancer 78:803–808. https://doi.org/10.1002/(SICI)1097-0142(19960815)78:4%3C803::AID-CNCR17%3E3.0.CO;2-Z
Pereira A, Magrina JF, Rey V, Cortes M, Magtibay PM (2007) Pelvic and aortic lymph node metastasis in epithelial ovarian cancer. Gynecol Oncol 105:604–608. https://doi.org/10.1016/j.ygyno.2007.01.028
Powless CA, Aletti GD, Bakkum-Gamez JN, Cliby WA (2011) Risk factors for lymph node metastasis in apparent early-stage epithelial ovarian cancer: implications for surgical staging. Gynecol Oncol 122:536–540. https://doi.org/10.1016/j.ygyno.2011.05.001
Querleu D, Lanvin D, Elhage A, Henry-Buisson B, Leblanc E (1998) An objective experimental assessment of the learning curve for laparoscopic surgery: the example of pelvic and para-aortic lymph node dissection. Eur J Obstet Gynecol Reprod Biology 81:55–58. https://doi.org/10.1016/S0301-2115(98)00155-9
Rouvière H (1932) Anatomie Des Lymphatiques De l’Homme. Masson, Paris
Suzuki M, Ohwada M, Yamada T, Kohno T, Sekiguchi I, Sato I (2000) Lymph Node Metastasis in Stage I epithelial ovarian Cancer. Gynecol Oncol 79:305–308. https://doi.org/10.1006/gyno.2000.5951
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, Gaudet MM, Jemal A, Siegel RL (2018) Ovarian cancer statistics, 2018. CA: A Cancer. J Clin 68:284–296. https://doi.org/10.3322/caac.21456
Van N-T, Nguyen-Xuan H-T, Koual M, Bentivegna E, Bats A-S, Azaïs H (2022) Place Du ganglion sentinelle dans la prise en charge Du cancer de l’ovaire de stade précoce: revue de la littérature. Gynecol Obstet Fertil Senol 50:75–81. https://doi.org/10.1016/j.gofs.2021.09.011
Vanneuville G, Mestas D, Le Bouedec G, Veyre A, Dauplat J, Escande G, Guillot M (1991) The lymphatic drainage of the human ovary in vivo investigated by isotopic lymphography before and after the menopause. Surg Radiol Anat 13:221–226. https://doi.org/10.1007/BF01627990
Wu P-C, Lang J-H, Huang R-L, Qu J-Y, Wang H, Tang M-Y, Zhao R-G, Lian L-J (1989) 14 lymph node metastasis and retroperitoneal lymphadenectomy in ovarian cancer. Baillieres Clin Obstet Gynaecol 3:143–155. https://doi.org/10.1016/S0950-3552(89)80049-5
Yuan Y, Gu Z-X, Tao X-F, Liu S-Y (2012) Computer tomography, magnetic resonance imaging, and positron emission tomography or positron emission tomography/computer tomography for detection of metastatic lymph nodes in patients with ovarian cancer: a meta-analysis. Eur J Radiol 81:1002–1006. https://doi.org/10.1016/j.ejrad.2011.01.112
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
FM, AW and EC wrote the main manuscript text and prepared all the figures AM, GF and LO gave their opinion on the clinical application and revised it critically for important intellectual contentJD, JL, CC, AB approved the version to be publishedAll authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The bodies had been donated to science, in accordance with current legislation.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Murris, F., Weyl, A., Ouldamer, L. et al. Contribution of the cadaveric recirculation system in the anatomical study of lymphatic drainage of the ovary: applications in the management of ovarian cancer. Surg Radiol Anat (2024). https://doi.org/10.1007/s00276-024-03406-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00276-024-03406-w