Abstract
Purpose
Slipped capital femoral epiphysis (SCFE) represents the preliminary stage of osteoarthritis. Reliable tools for outcome evaluation should be developed to prevent persisting defects. The functional outcome of SCFE-patients after growth arrest is analysed by instrumented 3D-gait analysis (GA). The results are matched to the clinical examination findings.
Methods
A total of 39 SCFE patients after growth arrest (18.8 years; BMI 26.5 kg/m²) with unilateral affection were included. The clinical results were classified according to Harris hip and clinical Heyman Herndon scores. 3D-GA-parameters were evaluated and compared to the sound side and a group of 40 healthy adults (28.0 years; 21.9 kg/m²). The subgroup analysis was performed according to clinical results.
Results
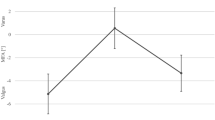
The clinical examination revealed very good results. GA could detect even small alterations. Some parameters indicated sustained functional impairments: Compared to the control group patients' walking speed (p = 0.022), step frequency (p < 0.001) and single support of the slip side (p < 0.001) decreased, while step width (p = 0.014), double support (p = 0.004) and stance time of sound side increased (p = 0.001). For kinematics patients, the sagittal range of motion (ROM) of pelvis (p < 0.001) and the external rotation of the ankle on both sides increased (p = 0.011) and sagittal ROM of hip (p = 0.002) and knee flexion of slip side (p < 0.001) decreased. The sagittal ROM of the ankle on the slip side decreased compared to the sound side (p = 0.003). Subgroup analysis revealed a positive correlation between clinically unsatisfying results and GA parameters.
Conclusions
Functional impairments in SCFE-patients can be found even after growth arrest. Alterations are explained partly by the disease and partly by patients' constitution. BMI-matched controls and long-term follow-up are needed.





Similar content being viewed by others
References
Rostoucher P, Bensahel H, Pennecot GF, Kaewpornsawan K, Mazda K (1996) Slipped capital femoral epiphysis: evaluation of different modes of treatment. J Pediatr Orthop B 5(2):96–101
Seller K, Raab P, Wild A, Krauspe R (2001) Risk-benefit analysis of prophylactic pinning in slipped capital femoral epiphysis. J Pediatr Orthop B 10(3):192–196
Zilkens C, Jäger M, Bittersohl B, Kim Y-J, Millis MB, Krauspe R (2009) Slipped capital femoral epiphysis, vol 9. European Instructional Lectures Springer, Dordrecht Heidelberg London New York. doi:10.1007978-3-642-00966-22
Bühligen U, Wojan M, Müller W, Salis-Soglio v. G, Sorge I, Till H (2007) Die Epiphyseolysis capitis femoris (ECF) des Jugendalters. Kinder- und Jugendmedizin 2:95–99
Milz S, Boszcyk A, Putz R (2002) Entwicklung und funktionelle Struktur der Epiphysenfugen. Der Orthopäde 9:835–840
Loder RT (1998) Slipped capital femoral epiphysis. Am Fam Physician 57(9):2135–2142
Westhoff B, Jäger M, Krauspe R (2007) Kindliche Beinachsen. Der Orthopäde 36:485–500
Zahrawi FB, Stephens TL, Spencer GEJ, Clough JM (1983) Comparative study of pinning in situ and open epiphysiodesis in 105 patients with slipped capital femoral epiphyses. Clin Orthop Relat Res 177:160–168. doi:0009-921X/83/0800/160
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(51):737–755
Kabada MP, Ramakrishnan HK, Wootten ME (1990) Measurement of lower extremity kinematics during level walking. J Orthop Res 8:383–392
Ounpuu S, Gage JR, Davis RB (1991) Three-dimensional lower extremity joint kinetics in normal pediatric gait. J Pediatr Orthop 11(3):341–349
Winter DA (1983) Energy generation and absorption at the ankle and knee during fast, natural, and slow cadences. Clin Orthop Relat Res 175:147–154. doi:0009-921X/83/0500/14
Seller K, Wild A, Westhoff B, Raab P, Krauspe R (2006) Clinical outcome after transfixation of the epiphysis with Kirschner wires in unstable slipped capital femoral epiphysis. Int Orthop 30(5):342–347. doi:10.1007/s00264-006-0110-2
Seller K, Wild A, Westhoff B, Raab P, Krauspe R (2006) Radiological evaluation of unstable (acute) slipped capital femoral epiphysis treated by pinning with Kirschner wires. J Pediatr Orthop B 15(5):328–334
Lehmann TG, Engesæter I, Laborie LB, Rosendahl K, Lie SA, Engesaeter LB (2011) In situ fixation of slipped capital femoral epiphysis with Steinmann pins- 67 patients followed for 2–16 years. Acta Orthop 82(3):333–338. doi:10.3109/17453674.2011.579520
Song KM, Halliday S, Reilly C, Keezel W (2004) Gait abnormalities following slipped capital femoral epiphysis. J Pediatric Orthop 24(2):148–155
Lai P, Leung A, Li A, Zhang M (2008) Three-dimensional gait analysis of obese adults. Clin Biomech 23:S2–S6. doi:10.1016/j.clinbiomech.2008.02.004
Bejek Z, Paroczai R, Illyes A, Kiss RM (2005) The influence of walking speed on gait parameters in healthy people and in patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 14:612–622. doi:10.1007/s00167-005-0005-6
Kirtley C, Whittle MW, Jefferson RJ (1985) Influence of walking speed on gait parameters. J Biomed Eng 7(4):282–288
Morrison S, Durward B, Watt G, Donaldson M (2008) The influence of body mass on the temporal parameters of peripubescent gait. Gait Posture 27(4):719–721. doi:10.1016/j.gaitpost.2007.09.003
Watelain E, Dujardin F, Babier F, Dubois D, Allard P (2001) Pelvic and lower limb compensatory actions of subjects in an early stage of hip osteoarthritis. Arch Phys Med Rehabil 82(12):1705–1711. doi:10.1053/apmr.2001.26812
Kiss RM (2010) Effect of walking speed and severity of hip osteoarthritis on gait variability. J Electromyogr Kinesiol 20(6):1044–1051
Stoquart G, Detrembleur C, Lejeune T (2008) Effect of speed on kinematic, kinetic, electromyographic and energetic reference values during treadmill walking. Neurophysiol Clin 38(2):105–116. doi:10.1016/j.neucli.2008.02.002
Teixeira-Salmela LF, Nadeau S, Milot M-H, Gravel D, Requiao LF (2008) Effects of cadence on energy generation and absorption at lower extremity joints during gait. Clin Biomech 23(6):769–778. doi:10.1016/j.clinbiomech.2008.02.007
Nantel J, Brochu M, Prince F (2006) Locomotor strategies in obese and non-obese children. Obesity (Silver Spring) 14(10):1789–1794
Acknowledgments
We thank Mrs. I. Kamps for assistance in performing the gait analysis and preparing the data for further analysis.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Westhoff, B., Ruhe, K., Weimann-Stahlschmidt, K. et al. The gait function of slipped capital femoral epiphysis in patients after growth arrest and its correlation with the clinical outcome. International Orthopaedics (SICOT) 36, 1031–1038 (2012). https://doi.org/10.1007/s00264-011-1409-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1409-1