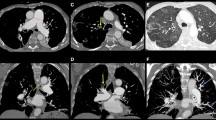
Abstract
Epoprostenol is a prostacyclin (prostaglandin I2) analog that causes vasodilation and inhibits platelet aggregation and is used in the management of severe pulmonary arterial hypertension (PAH). We herein report a patient with PAH who developed pancreatic enlargement after the initiation of therapy including epoprostenol. Although it is well known that thyroid enlargement occurs in patients with PAH receiving epoprostenol therapy, the pancreatic findings associated with epoprostenol therapy have not been well described. Although the size of the pancreas was clearly increased, there was no blood data or symptoms suggestive of abnormal pancreatic function and pancreatitis, and the patient’s abdominal complaints improved quickly, despite the continuation of epoprostenol therapy. Eleven months after the start of continuous intravenous epoprostenol infusion therapy, the pancreatic enlargement was still evident on imaging, but there were no abdominal symptoms or elevated pancreatic enzymes. This case highlights the fact that epoprostenol therapy may cause pancreatic changes that mimic acute or autoimmune pancreatitis.




Similar content being viewed by others
References
McLaughlin VV, McGoon MD (2006) Pulmonary arterial hypertension. Circulation 114:1417–1431
Prins KW, Thenappan T (2016) World health organization group I pulmonary hypertension: Epidemiology and pathophysiology. Cardiol Clin 34:363–374
Galiè N, Humbert M, Vachiery J-L, et al (2015) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 46:903–975
Fukuda K, Date H, Doi S, et al (2019) Guidelines for the Treatment of Pulmonary Hypertension (JCS 2017/JPCPHS 2017). Circ J 83:842–945
Barst RJ, Rubin LJ, Long WA, et al (1996) A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med 334:296–301
Chadha C, Pritzker M, Mariash CN (2009) Effect of epoprostenol on the thyroid gland: enlargement and secretion of thyroid hormone. Endocr Pract 15:116–121
Satoh M, Aso K, Nakayama T, Saji T (2017) Effect of treatment with epoprostenol and endothelin receptor antagonists on the development of thyrotoxicosis in patients with pulmonary arterial hypertension. Endocr J 64:1173–1180
Menon AA, Sahay S, Braverman LE, Farber HW (2019) Thyroid Dysfunction in Patients with Pulmonary Artery Hypertension (PAH): The Effect of Therapies Affecting the Prostanoid Pathway. Lung 197:761–768
Saisho Y, Butler AE, Meier JJ, et al (2007) Pancreas volumes in humans from birth to age one hundred taking into account sex, obesity, and presence of type-2 diabetes. Clin Anat 20:933–942
Shirai Y, Tamura Y, Yasuoka H, et al (2014) IgG4-related disease in pulmonary arterial hypertension on long-term epoprostenol treatment. Eur Respir J 43:1516–1519
Majed BH, Khalil RA (2012) Molecular mechanisms regulating the vascular prostacyclin pathways and their adaptation during pregnancy and in the newborn. Pharmacol Rev 64:540–582
Beswick IP, Pirola RC, Bouchier IA (1971) The cause of pancreatic enlargement in rats fed raw soybean. Br J Exp Pathol 52:252–255
Kato M, Ohkuma S, Kataoka K, et al (1994) Mechanisms for pancreatic hypertrophy induced by long-term administration of bethanechol. Eur J Pharmacol (Environ Toxicol Pharmacol Sect) 292:47–55
Homma T, Malik KU (1982) Effect of prostaglandins on pancreatic circulation in anesthetized dogs. J Pharmacol Exp Ther 222:623–628
Dolenšek J, Pohorec V, Rupnik MS, Stožer A (2017) Pancreas Physiology. In: Seicean A (ed) Challenges in Pancreatic Pathology. IntechOpen, Rijeka
Glasbrenner B, Adler G (1993) Pathophysiology of acute pancreatitis. Hepatogastroenterology 40:517–521
Zhang X-M, Feng Z-S, Zhao Q-H, et al (2006) Acute interstitial edematous pancreatitis: Findings on non-enhanced MR imaging. World J Gastroenterol 12:5859–5865
Notohara Kenji ZL (2013) Histology of autoimmune pancreatitis. The Pancreapedia: Exocrine Pancreas Knowledge Base
Takahashi M, Fu**aga Y, Notohara K, et al (2020) Diagnostic imaging guide for autoimmune pancreatitis. Jpn J Radiol 38:591–612
Kamisawa T, Takuma K, Anjiki H, et al (2010) Differentiation of autoimmune pancreatitis from pancreatic cancer by diffusion-weighted MRI. Am J Gastroenterol 105:1870–1875
Acknowledgements
We thank Kelly Zammit, BVSc, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was waived in this case report in accordance with the opt-out method used at our institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Someya, Y., Koyasu, S., Ohnishi, Y. et al. Pancreatic enlargement in a patient receiving therapy with vasodilators for pulmonary arterial hypertension: a case report. Abdom Radiol 47, 1948–1953 (2022). https://doi.org/10.1007/s00261-022-03458-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03458-9