Abstract
Objective
To define the clinical importance of various pediatric musculoskeletal diagnoses, determine preferred communication methods based on the acuity level of findings, and investigate differences between specialties utilizing the Delphi methodology.
Methods
Radiologists, orthopedic surgeons, and sports-medicine pediatricians at a tertiary children’s hospital were surveyed (n = 79) twice using REDCap (Research Electronic Data Capture). Surveys were conducted anonymously and at least 1 year apart, first eliciting all potentially non-routine findings and various communication methods (round 1), and later categorizing the acuity (emergent, urgent, or non-urgent) of different diagnosis categories and selecting the preferred communication method (verbal, written electronic messages, and report) and timeframe (round 2). Chi-square, Fisher’s exact, and Kruskal–Wallis H tests were used to compare variables between specialties.
Results
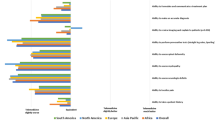
Round 1 produced 267 entries for non-routine findings (grouped into 19 diagnoses) and 71 for communication methods (grouped into 3 categories). Round 2 found no significant difference in the acuity assignments for the 19 predetermined diagnoses (p = 0.66) between the 3 specialties; however, there was reduced agreement for the top urgent diagnoses within and between specialties. Most pediatricians preferred written electronic messages. The preferred communication timeframe for urgent diagnoses was significantly different (< 2 h for pediatricians, < 4 h for radiologists, and < 8 h for surgeons; p = 0.003) between specialties whereas no difference was found for emergent (p = 1) and non-urgent diagnoses (p = 0.80).
Conclusion
Acuity assignment for the 19 pediatric-specific musculoskeletal diagnoses was not significantly different between specialties, but the preferred communication timeframe for urgent diagnoses was significantly different, ranging between 2 and 8 h.



Similar content being viewed by others
Change history
12 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00256-022-03991-0
References
Siewert B, Brook OR, Hochman M, Eisenberg RL. Impact of communication errors in radiology on patient care, customer satisfaction, and work-flow efficiency. AJR Am J Roentgenol. 2016;206:573–9.
Berlin L. Communicating nonroutine radiologic findings to the ordering physician: will (should) information technology-assisted communication replace direct voice contact? Radiology. 2015;277:332–6.
Larson PA, Berland LL, Griffith B, Kahn CE Jr, Liebscher LA. Actionable findings and the role of IT support: report of the ACR Actionable Reporting Work Group. J Am Coll Radiol. 2014;11:552–8.
ESR communication guidelines for radiologists. Insights Imaging. 2013;4(2):143–6.
Fritzsche PJ. Communication: the key to improved patient care. Radiology. 2005;234:13–4.
Kushner DC, Lucey LL. Diagnostic radiology reporting and communication: the ACR guideline. J Am Coll Radiol. 2005;2:15–21.
American College of Radiology (ACR). ACR practice parameters for communication of diagnostic imaging findings (revised 2020). [Internet]. ACR. ACR; 2020 [cited 2021 Feb 27]. Available from: ACR website. www.acr.org/~/media/C5D1443C9EA4424AA12477D1AD1D927D.pdf. Published 1991. Updated 2020.
Harvey HB, Alkasab TK, Pandharipande PV, et al. Radiologist compliance with institutional guidelines for use of nonroutine communication of diagnostic imaging results. J Am Coll Radiol. 2015;12:376–84.
Nguyen JC, Markhardt BK, Merrow AC, Dwek JR. Imaging of pediatric growth plate disturbances. Radiographics. 2017;37:1791–812.
Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Manage Sci. 1963;9:458–67.
Hsu C-C, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12:10.
Zha N, Alabousi M, Katz DS, Su J, Patlas M. Factors affecting response rates in medical imaging survey studies. Acad Radiol. 2020;27:421–7.
Acknowledgements
We would like to thank Maya Patel, B.S. and Michael K. Nguyen, B.A. for their assistance in creating the RedCap surveys. We also would like to acknowledge the Department of Radiology and Division of Orthopedics at the Children’s Hospital of Philadelphia for their support of this project and multiple members from both specialties who provided their perspective, expertise, and insightful feedback on this project, particularly Matthew F. Grady, M.D. from Orthopedics and Ann M. Johnson, M.D. from Radiology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AA receives research grant support from the Radiology Society of North America (RSNA) and the Children’s Cancer Research Fund (CCRF), unrelated to this project. JCN receives research grant support from the Radiology Society of North America (RSNA) and the Children’s Cancer Research Fund (CCRF), unrelated to this project. The rest of the authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised. The name of Marian Gaballah is corrected.
Rights and permissions
About this article
Cite this article
Hussaini, S.H., Gaballah, M., Baghdadi, S. et al. Pediatric musculoskeletal pathologies: are there differences in triage of diagnoses and preferences for communication between radiology and orthopedics?. Skeletal Radiol 51, 863–871 (2022). https://doi.org/10.1007/s00256-021-03961-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03961-y