Abstract
Background
Over the last two decades, fetal imaging has greatly improved, and new prenatal imaging measurements have been developed to characterize congenital diaphragmatic hernia (CDH) severity.
Objective
To determine the best prenatal imaging predictor of postnatal CDH outcomes, including use of extracorporeal membrane oxygenation (ECMO) and in-hospital mortality, with particular attention to the percentage of liver herniation (%LH) as a predictor. Additionally, we sought to guide best practices across hospital systems including improved models of prenatal risk assessment.
Materials and methods
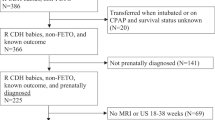
We conducted a retrospective review of infants with left CDH who were prenatally diagnosed. We analyzed prenatal imaging measurements including observed-to-expected (O/E) lung-to-head ratio (LHR) on US, percentage predicted lung volume (PPLV) on MRI, and O/E total fetal lung volume (TFLV) and %LH on MRI. We compared prenatal imaging characteristics for infants with (1) in-hospital postnatal mortality and (2) use of ECMO. Then we performed multivariate logistic regression to determine independent predictors of postnatal outcomes.
Results
We included 63 infants with a median gestation of 34 weeks at the time of prenatal MRI. Low O/E LHR (31.2 vs. 50, P < 0.0001), PPLV (14.7 vs. 22.6, P < 0.0001) and O/E TLFV (24.6 vs. 38.3, P < 0.0001) and high %LH (15.1 vs. 2.1, P = 0.0006) were associated with worse postnatal outcomes; however, only PPLV was predictive of survival and need for ECMO on multivariable analysis. PPLV survival to discharge model showed an area under the curve (AUC) of 0.93 (95% confidence interval [CI]: 0.86, 0.99), P < 0.0001; and an odds ratio of 68.7 (95% CI: 6.5–2,302), P = 0.003. PPLV need for ECMO model showed AUC = 0.87 (95% CI: 0.78, 0.96), P < 0.0001; and odds ratio = 20.1 (95% CI: 3.1–226.3), P = 0.011.
Conclusion
Low O/E LHR, PPLV and O/E TFLV and high %LH in the third trimester are associated with worse postnatal outcomes. PPLV most strongly predicted outcome using a logistic regression model. Percentage of liver herniation was not an independent predictor of outcomes.




Similar content being viewed by others
References
Keijzer R, Puri P (2010) Congenital diaphragmatic hernia. Semin Pediatr Surg 19:180–185
Kosiński P, Wielgoś M (2017) Congenital diaphragmatic hernia: pathogenesis, prenatal diagnosis and management — literature review. Ginekol Pol 88:24–30
Mesas Burgos C, Hammarqvist-Vejde J, Frenckner B, Conner P (2016) Differences in outcomes in prenatally diagnosed congenital diaphragmatic hernia compared to postnatal detection: a single-center experience. Fetal Diagn Ther 39:241–247
Oluyomi-Obi T, Kuret V, Puligandla P et al (2017) Antenatal predictors of outcome in prenatally diagnosed congenital diaphragmatic hernia (CDH). J Pediatr Surg 52:881–888
Shieh HF, Barnewolt CE, Wilson JM et al (2017) Percent predicted lung volume changes on fetal magnetic resonance imaging throughout gestation in congenital diaphragmatic hernia. J Pediatr Surg 52:933–937
Rypens F, Metens T, Rocourt N et al (2001) Fetal lung volume: estimation at MR imaging — initial results. Radiology 219:236–241
Albanese CT, Lopoo J, Goldstein RB et al (1998) Fetal liver position and perinatal outcome for congenital diaphragmatic hernia. Prenat Diagn 18:1138–1142
Zamora IJ, Oluyinka OO, Cass DL et al (2014) Prenatal MRI fetal lung volumes and percent liver herniation predict pulmonary morbidity in congenital diaphragmatic hernia (CDH). J Pediatr Surg 49:688–693
Akinkuotu AC, Cruz SM, Abbas P et al (2016) Risk-stratification of severity for infants with CDH: prenatal versus postnatal predictors of outcome. J Pediatr Surg 51:44–48
Worley KC, Dashe JS, Barber RG et al (2009) Fetal magnetic resonance imaging in isolated diaphragmatic hernia: volume of herniated liver and neonatal outcome. Am J Obstet Gynecol 200:318.e311–318.e316
Cannie M, Jani J, Chaffiotte C et al (2008) Quantification of intrathoracic liver herniation by magnetic resonance imaging and prediction of postnatal survival in fetuses with congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 32:627–632
Gien J, Kinsella JP (2016) Differences in preductal and postductal arterial blood gas measurements in infants with severe congenital diaphragmatic hernia. Arch Dis Child Fetal Neonatal Ed 101:F314–318
Phillips R, Shahi N, Meier M et al (2021) The novel fetal MRI O/E CLV versus O/E LHR in predicting prognosis in congenital diaphragmatic hernias: can we teach an old dog new tricks? Pediatr Surg Int 37:1499–1504
Meyers ML, Garcia JR, Blough KL et al (2018) Fetal lung volumes by MRI: normal weekly values from 18 through 38 weeks’ gestation. AJR Am J Roentgenol 211:432–438
Phillips RC, Shahi N, Leopold D et al (2020) Thromboelastography-guided management of coagulopathy in neonates with congenital diaphragmatic hernia supported by extracorporeal membrane oxygenation. Pediatr Surg Int 36:1027–1033
Metkus AP, Filly RA, Stringer MD et al (1996) Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg 31:148–151
Jani J, Nicolaides KH, Keller RL et al (2007) Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol 30:67–71
Barnewolt CE, Kunisaki SM, Fauza DO et al (2007) Percent predicted lung volumes as measured on fetal magnetic resonance imaging: a useful biometric parameter for risk stratification in congenital diaphragmatic hernia. J Pediatr Surg 42:193–197
Hedrick HL (2010) Management of prenatally diagnosed congenital diaphragmatic hernia. Semin Fetal Neonatal Med 15:21–27
Perrone EE, Abbasi N, Sanz Cortes M et al (2021) Prenatal assessment of congenital diaphragmatic hernia at North American fetal therapy network centers: a continued plea for standardization. Prenat Diagn 41:200–206
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Niemiec, S.M., Louiselle, A.E., Phillips, R. et al. Third-trimester percentage predicted lung volume and percentage liver herniation as prognostic indicators in congenital diaphragmatic hernia. Pediatr Radiol 53, 479–486 (2023). https://doi.org/10.1007/s00247-022-05538-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05538-w