Abstract
Appropriate use criteria (AUC) for the performance of outpatient transthoracic echocardiography are based on history, physical examination and electrocardiograms. Telehealth provides access to clinical care in the absence of a physical examination. We assessed application of AUC for performance of echocardiography following a telehealth visit. In this single center study, we retrospectively reviewed the charts of pediatric patients whose originally scheduled in person visits were converted to telehealth visits between March and May 2020. Patients were referred for echocardiogram by the telehealth cardiologist. Echocardiograms requested during the telehealth visit were retrospectively classified as appropriate [A], may be appropriate [M], or rarely appropriate [R] by two independent reviewers. Findings from the echocardiogram were classified as normal, abnormal, or abnormal and motivating treatment by the same two independent reviewers based upon results from the echocardiogram report and physician office visit note. Of the 441 patients seen by telehealth, interquartile range of 1.9–15.3 years, 114 (26%) patients were referred for an echocardiogram. Of the patients for whom echocardiograms were requested, 56/114 (49%) were new to cardiology. Echocardiograms were rated: A-85 (75%), M-5 (4%), and R-24 (21%). Of the 108 completed studies, 61 (56%) were normal, 44 (41%) were abnormal, and three (3%) were abnormal motivating treatment. Abnormal TTE findings were not detected in the R encounters compared with abnormal findings in 46/82 (56%) of the A completed studies. Seventy-one percent (15/21) of the R-rated studies were performed for murmur evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transthoracic echocardiography (TTE) is a powerful imaging tool with widespread use in pediatric cardiology. TTE is a safe and cost-effective noninvasive modality when used appropriately. Appropriate use criteria (AUC) designed to provide best practices for incorporating echocardiography into clinical care have been published [1,2,3]. Validation and implementation studies of AUC for transthoracic echocardiography provide insight into the factors influencing resource utilization and have assisted in creating the framework for designing quality improvement initiatives [4]. Since the beginning of the COVID-19 pandemic, changes in healthcare delivery have led to more widespread changes in the care delivery model, including more widespread adoption of telehealth [5].
Telehealth is defined by the National Institutes of Health as the use of technology and telecommunications to provide medical information and services at a distance. It involves the establishment of a connection between physicians and patients, and for pediatric cardiology, includes consultation of the newborn with suspected congenial heart disease, the care of pediatric patients presenting for initial and follow-up care, and providing expertise in the management of the adult congenital patient [6, 7]. While the established AUC documents help to guide decision making on imaging to avoid performing rarely appropriate echocardiograms, there are currently no standards or recommendations for how best to determine the need for echocardiogram during a telehealth visit. One of the largest series to evaluate the impact of telehealth on delivery of pediatric cardiac care in community hospitals found a positive impact on referral patterns and time management without increasing the utilization of echocardiography [6]. However, this study was published before the guidelines for AUC were established and only included patients admitted in the nursery. Implementation studies evaluating the use of AUC in pediatric and adult cardiology have been instrumental in recognizing the appropriateness of the imaging studies and identifying any deficiencies. In this study, we determine the clinical applicability of existing AUC in telehealth evaluations. The primary outcome measure was the number of studies ordered for appropriate [A], maybe appropriate [M] and rarely [R] appropriate indications. We also report the findings from these studies. Secondary outcome measures were the yield of the findings for the various AUC indications and the influence of age and visit diagnosis on the diagnostic yield of TTE.
Materials and Methods
This single health system study was approved by the Nemours-Delaware Institutional Review Board.
Patient Selection
We included all Nemours-Delaware pediatric patients whose outpatient pediatric cardiology visits had been converted to a telehealth format between March and May 2020. Patients included follow-up as well as new referrals. Documentation from each telehealth visit was retrospectively assessed by 2 independent reviewers (DK, PN). Extracted data included date of birth, biologic-sex, demographic data (e.g., state residence), reason for telehealth visit (e.g., primary diagnosis), insurance type, whether an echocardiogram was ordered, and whether the patient was new (versus return patient). Reasons for echocardiography were simplified to the following 11 categories for analysis: abnormal ECG/syncope, abnormal prenatal ultrasound, cardiomyopathy/screening for cardiac target organ damage secondary to systemic hypertension, chest pain, family history of heart disease, murmur, palpitations/arrhythmia, systemic/genetic predisposition disorders, unrepaired congenital heart disease (CHD), repaired CHD, and other (e.g., dizziness, shortness of breath).
Appropriate Use Criteria
The 2 independent reviewers utilized ACC AUC criteria to rate each echocardiogram indication as appropriate (A), may be appropriate (M), or rarely appropriate (R) based upon existing guidelines. According to ACC AUC, appropriate [A] rating is defined as “generally acceptable and a reasonable approach for the indication”; [M] rating is “defined as may be generally acceptable and may be a reasonable approach for the indication”; and [R] rating as “not indicated” (Fig. 1).
Echocardiogram Findings
Echocardiogram results were classified as normal (N), abnormal (AB), or abnormal and motivating treatment (ABMT). Normal results required no intervention, cardiology follow-up, or change in management. Normal results also included incidental findings such as patent foramen ovale and aortic arch branching variants not associated with a vascular ring. New visits for a heart murmur were deemed appropriate if age at referral was less than 1 year or if greater than 1 year and the description of the murmur provided by the pediatrician was suggestive of a potentially pathologic murmur (e.g., diastolic murmur, murmur grade > II/VI, etc.). Abnormal TTE findings were further categorized as ABMT if they were followed by interventional cardiac catheterization, cardiac surgery, ablation, device implantation, or treatment with a newly prescribed cardiac medication.
Statistical Approach
Descriptive statistics were performed for all variables of interest. Count, median, and interquartile range were calculated. Univariate analyses of continuous data were carried out via Mann Whitney rank test for comparison of medians. Univariate analysis of categorical data was carried out using chi-square test or Fisher’s exact test. All statistical analyses were carried out using SAS 9.4 (Chapel Hill, North Carolina). Significance level of p < 0.05.
Results
Demographics
There were 441 patients with a median age of 9.8 years and interquartile range of 1.9–15.3, of whom 210/441 (48%) were female. Telehealth participants were from Delaware 223/441 (51%), Pennsylvania 144/441 (33%), New Jersey 52/441 (12%), and Maryland 21/441 (5%) (data not shown).
Transthoracic Echocardiogram Studies
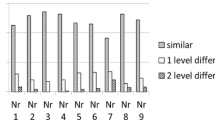
There were 114 (26%) echocardiograms ordered by the telehealth physician. Of the 114 echocardiograms ordered, 108 (95%) were completed by the time of this review (June 15, 2022). The median number of days between the telehealth visit and echocardiogram completion was 41.5 days with an interquartile range of 15.5–94 days. Of the patients who had an echocardiogram ordered, 56/114 (49%) were new to cardiology and 52/114 (46%) were first-time studies. There were significantly higher proportions of new patients and first-time echocardiograms, 88% and 92%, respectively in the R studies (Table 1). Appropriateness ratings were as follows: A, in 85/114 studies (75%), M in 5/114 studies (4%), and R in 24/114 studies (21%) (Fig. 2). The majority of patients in the A, M, and R groups were between 1 month and 10 years of age (54%, 80%, and 67%, respectively) (Fig. 3).
Visit Diagnoses
Echocardiograms were ordered by the TH pediatric cardiologist for the following reasons: unrepaired CHD (23.7%), repaired CHD (11.4%), murmur (18.4%), and abnormal electrocardiogram/syncope (8.8%). Most common indications for ordering a TTE in the A group were known congenital heart disease (repaired (14%) and unrepaired (31%)); systemic/genetic predisposition including history of Kawasaki (11%), abnormal ECG/syncope (9.4%) and exertional chest pain (7.1%). In the M group, the most common indications for ordering an echocardiogram was a systemic abnormality (40%) (e.g., history of pectus excavatum, remote history of myocarditis), followed by abnormal prenatal ultrasound (e.g., echogenic focus) (20%), family history of heart disease (20%), and unrepaired CHD (20%) (e.g., very mild pulmonary valve stenosis based upon a prior echocardiogram obtained 2 years prior). In the R group, the most common indication was cardiac murmur, which made up 71% of the R studies (Fig. 3).
Echocardiogram Results
Echocardiogram results were normal in 61/108 (56%), abnormal in 44/108 (41%), and abnormal motivating treatment in 3/108 (3%) patients. Of the abnormal or abnormal motivating treatment studies 9/47 (19%) were new patients of which 4/9 (44%) were patients older than 10 years of age, 3/9 (33%) were patients 1 month–10 years of age, and 2/9 (22%) were patients less than 1 month of age. In the A group, of the 82 echocardiograms that were completed, 43 (52%) were abnormal and 3(4%) were abnormal motivating treatment which was significantly higher than the M or R groups (p < 0.0001) (data not shown). Regarding the three echocardiograms classified as ABMT, the first was a 7 month-old follow-up patient with a history of coarctation presenting with re-coarctation requiring intervention. The second, a 7 month-old follow-up patient with unrepaired Ebstein’s anomaly with new history of cyanosis who was referred for surgery. The third, a 12 year-old new patient with an unusual history of syncope who was found to have non compaction cardiomyopathy and a coronary abnormality which prompted further imaging, testing, and management. In the A group, 18/43(42%) of the abnormal studies were found in patients older than 10 years of age. In the M group, 1 of 5 (20%) had abnormal echocardiograms and were between 1 month and 10 years of age and 4/5 (80%) had normal echocardiograms and 3 out of 4 (75%) were between 1 month and 10 years of age. In the R group, of the 21 echocardiograms that were completed, none were abnormal or motivated intervention. Of the abnormal or abnormal motivating treatment studies only 9/47 (19%) were new patients all of which were rated A and 7/9 (78%) were patients older than 1 month of age while 2/9 (22%) were less than 1 month of age (Fig. 4).
Discussion
This study highlights TTE utilization and appropriateness of echocardiogram in the absence of auscultation, vitals, and ECG using telehealth visits during the early phase of the COVID-19 pandemic. We found that most TTEs ordered by pediatric cardiologists, when using telehealth for outpatient visits, were for indications rated A, and that the most common indication for R-rated studies was for the evaluation of cardiac murmurs that were determined to be innocent based upon normal echocardiogram findings. We demonstrated that appropriate indications for TTE were associated with a higher yield of abnormal findings, consistent with previous studies, however, our overall yield of R echocardiograms was higher than that seen in several recent studies prior to the COVID-19 pandemic, and the use of telehealth likely due to the inability to perform physical examinations. However, these numbers were also influenced by a pre-determination that all infants with murmurs would be referred for TTE, regardless of the murmur description provided by the pediatrician. The authors note, however, that prescribing appropriateness to findings of a murmur alone based on age and described quality did not yield any significant abnormality on echocardiograms (Fig. 5).
Normal versus abnormal echocardiogram findings by appropriate use criteria. Absolute counts. Echocardiographic findings reflecting the proportion of N normal, AB abnormal, and ABMT abnormal motivating treatment within each appropriateness category. p < 0.0001. A total of N = 6 requested echocardiograms were not performed, three in the appropriate category and three in the rarely appropriate category
In 2015, Sachdeva et al. published a study focusing on the use of TTE at initial outpatient visits. This study was done before the release of the AUC document; however, the authors evaluated 2655 studies and showed that 12% of patients were included in the R group. The most common R indications included innocent murmurs and syncope or palpitations with no other indications of cardiovascular disease, benign family history, and normal ECG [4]. Similar R indications were also demonstrated by Cartoski et al. in 2018. The authors evaluated 1383 TTEs done at the initial outpatient visit and found 16.4% of patients met criteria for the R group. They noted that the most common R indications included innocent murmurs; palpitations without additional symptoms with a benign history and ECG; and syncope with no significant family history, normal ECG, and no other symptoms [8]. Our study is among the first to assess adherence to AUC in telehealth visits, and the consistent over utilization of echocardiography in patients with cardiac murmurs highlights a gap in our current practices. Additionally, given the higher percentage of R-rated TTE’s compared to pre-pandemic studies, we have demonstrated the importance of identifying appropriate patient populations, age groups and specific diagnoses best suited for telehealth. One method proposed to enhance identification of individuals most in need of an echocardiogram would be to use remote auscultation devices. To date, there have been limited studies demonstrating the utility of real-time remote auscultation devices; however, our study suggests a need for additional studies assessing the use of such devices during telehealth visits in order to reduce the number of inappropriate echocardiograms requested (Table 2).
Limitations
This study is a retrospective single center study, with all associated limitations. Patients referred for a murmur were not chosen for telehealth visits over an in person visit but rather those visits were all converted to telehealth visits and only follow-up patients or non-urgent referrals deferred to be seen at a later time. Thus, some selection bias may be present since pediatric cardiologists at our institution selected which patients from their panel required in person visits at a later time and which could be converted to telehealth. We acknowledge the limitation of this study to perform a physical exam in the evaluation of a murmur and determination of appropriate use of echocardiography at a distance which is inherent to the nature of this study.
Conclusion
The increase in use of telehealth in pediatric cardiology due to the COVID-19 pandemic will have a lasting impact on our daily practice. Several studies have shown improvement in providing high quality care to a greater number of patients and improvement in prompt and accurate diagnoses with its utilization. Our study is unique in highlighting a significant change in practice with adoption of telehealth at the onset of the COVID-19 pandemic at our institution. The use of telehealth, however, must include identifying appropriate patient populations and specific diagnoses best suited for telehealth as well as abiding by appropriate use criteria when ordering diagnostic testing. Telehealth has limited assessment of appropriateness in those with primary diagnoses of cardiac murmurs and this study emphasizes the need for development of telehealth-targeted guidelines based on history that can help guide resource utilization for outpatient cardiac evaluations. On the other hand- it validates almost all other AUC categories. Presence of a murmur and age along may not be sufficient to merit an echocardiogram—and need for expert clinical auscultation and perhaps utilization of tele-auscultation tools may be of utility in these patients. And encourages exploring the utility of remote tele-auscultation devices and technology to assist in abiding by AUC when ordering diagnostic testing.
Abbreviations
- AUC:
-
Appropriate use criteria
- TTE:
-
Transthoracic echocardiography
- A:
-
Appropriate
- M:
-
May be appropriate
- R:
-
Rarely appropriate
- N:
-
Normal echocardiogram
- AB:
-
Abnormal echocardiogram
- ABMT:
-
Abnormal echocardiogram motivating treatment
References
Campbell RM, Douglas PS, Eidem BW, Lai WW, Lopez L, Sachdeva R (2014) ACC/AAP/AHA/ASE/HRS/SCAI/SCCT/SCMR/SOPE 2014 appropriate use criteria for initial transthoracic echocardiography in outpatient pediatric cardiology: a report of the American College of Cardiology Appropriate use task force, American Academy of Pediatrics, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. J Am Coll Cardiol 64:2039–2060. https://doi.org/10.1016/j.jacc.2014.08.003
American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society (2011) ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropriate use criteria for echocardiography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American College of Chest Physicians. J Am Soc Echocardiogr 24:229–267. https://doi.org/10.1016/j.echo.2010.12.008
Writing Group, Sachdeva R, Valente AM, Armstrong AK, Cook SC, Han BK et al (2020) ACC/AHA/ASE/HRS/ISACHD/SCAI/SCCT/SCMR/SOPE 2020 appropriate use criteria for multimodality imaging during the follow-up care of patients with congenital heart disease: a report of the American College of Cardiology Solution Set Oversight Committee and Appropriate Use Criteria Task Force, American Heart Association, American Society for Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. J Am Coll Cardiol 33:e1–e48. https://doi.org/10.1016/j.echo.2020.04.026
Sachdeva R, Allen J, Benavidez OJ, Campbell RM, Douglas PS, Eidem BW et al (2015) Pediatric appropriate use criteria implementation project: a multicenter outpatient echocardiography quality initiative. J Am Coll Cardiol 66:1132–1140. https://doi.org/10.1016/j.jacc.2015.06.1327
Monaghesh E, Hajizadeh A (2020) The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20:1193. https://doi.org/10.1186/s12889-020-09301-4
Sable CA, Cummings SD, Pearson GD, Schratz LM, Cross RC, Quivers ES et al (2002) Impact of telemedicine on the practice of pediatric cardiology in community hospitals. Pediatrics 109:e3
Satou GM, Rheuban K, Alverson D, Lewin M, Mahnke C, Marcin J et al (2017) Telemedicine in pediatric cardiology: a scientific statement from the American Heart Association. Circulation 135:e648–e678. https://doi.org/10.1161/CIR.0000000000000478
Cartoski MJ, Kiley M, Spevak PJ (2018) Appropriate use criteria for paediatric echocardiography in an outpatient practice: a validation study. Cardiol Young 28:862–867. https://doi.org/10.1017/S1047951118000513
Funding
Funded by the Delaware ACCEL COVID-19 Rapid Pilot Award; the DE ACCEL pilot program is supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (U54GM104941) and the State of Delaware. Funding for this project was provided by Delaware ACCEL Rapid COVID-19 grant (PI- C. Baker-Smith).
Author information
Authors and Affiliations
Contributions
SS contributed to the conception of the study. DK, CBS, and SS contributed to the design of the study. Coauthors DK, PN, EMG, and Baker-Smith contributed to the acquisition of the data. DK and CBS contributed to the analysis of the data. CBS completed statistical analysis in SAS. All authors contributed to the interpretation of the data. DK, PN, and CBS drafted the article. All authors critically reviewed the document for intellectual content. Final approval of the submitted version was obtained from all coauthors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The following authors report no actual or potential conflicts of interest related to this document: Daphney Kernizan, DO; Carissa M. Baker-Smith, MD MPH; Priya Nigam, MD; Elaine M. Geary, ARNP; Shubhika Srivastava, MBBS FASE. No potential conflicts of interest exist with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kernizan, D., Srivastava, S., Nigam, P. et al. Telehealth and Application of Appropriate Use Criteria for Pediatric Transthoracic Echocardiography. Pediatr Cardiol 44, 640–646 (2023). https://doi.org/10.1007/s00246-022-02985-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02985-y