Abstract
The risk factors of complications after SWL are not well characterized. Therefore, based on a large prospective cohort, we aimed to develop and validate a nomogram for predicting major complications after extracorporeal shockwave lithotripsy (SWL) in patients with ureteral stones. The development cohort included 1522 patients with ureteral stones who underwent SWL between June 2020 and August 2021 in our hospital. Five hundred and fifty-three patients with ureteral stones participated in the validation cohort from September 2020 to April 2022. The data were prospectively recorded. Backward stepwise selection was applied using the likelihood ratio test with Akaike’s information criterion as the stop** rule. The efficacy of this predictive model was assessed concerning its clinical usefulness, calibration, and discrimination. Finally, 7.2% (110/1522) of patients in the development cohort and 8.7% (48/553) of those in the validation cohort suffered from major complications. We identified five predictive factors for major complications: age, gender, stone size, Hounsfield unit of stone, and hydronephrosis. This model showed good discrimination with an area under the receiver operating characteristic curves of 0.885 (0.872–0.940) and good calibration (P = 0.139). The decision curve analysis showed that the model was clinically valuable. In this large prospective cohort, we found that older age, female gender, higher Hounsfield unit, size, and grade of hydronephrosis were risk predictors of major complications after SWL. This nomogram will be helpful in preoperative risk stratification to provide individualized treatment recommendations for each patient. Furthermore, early identification and appropriate management of high-risk patients may decrease postoperative morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of urolithiasis ranges from 1 to 13% worldwide, about 50% of patients experienced at least one stone recurrence during their lifetime [1]. Urolithiasis may accompany significant complications, including colic episodes, infection, hydronephrosis, and even impairment of renal function [2], which commonly occur in ureteral stones. Extracorporeal shock wave lithotripsy (SWL) is currently one of the preferred treatment options for ureteral stones [3, 4]. It has the advantages of relative non-invasiveness, low morbidity, having no anesthesia requirement, and being an outpatient procedure. Although SWL is considered a safe and well-tolerated procedure, it is not without its dangers and can be accompanied by certain complications that need to be managed [5], such as infection, steinstrasse, renal colic, and renal hematoma. These complications require accurate evaluation because every possible preventive measure should be implemented.
The coronavirus disease 2019 (COVID-19) pandemic has presented urologists with previously unknown challenges [6]. Along with social restrictions and lockdowns, entire hospitals were turned into treatment facilities for COVID-19-infected patients. Due to the unavoidable increase in virus transmission risk, surgical activity had to be reduced [7]. SWL is a good option for patients with stone disease because it does not require anesthesia or intubation, which significantly increase the risk of transmission, requires no hospital stay, and is associated with fewer emergency room visits [8]. Therefore, it is even more essential to be informed about the associated complications and to systematically counsel eligible patients for SWL during this pandemic.
Many studies have explored the risk factors of complications after endoscopic surgery, such as percutaneous or ureteroscopic surgery. However, only several retrospective studies have addressed this issue in SWL, and they were published two decades ago. In a retrospective study that included 4,634 patients with upper urinary stones and treated with SWL, Madbouly et al. [9] found that steinstrasse was recorded in 3.97% (184/4634) of patients and was significantly correlated with stone size and renal morphology (hydronephrosis). In another retrospective study that included 1427 patients with ureteral stones treated with SWL using electromagnetic generator, Tan et al. [10] reported that the morbidity rate requiring hospital admission was 2.9%. The most common cause was for pain control (1.8%), predominantly in cases of larger stones. In addition, the incidence of febrile urinary tract infection and urosepsis after SWL is relatively low, around 1% of cases. The risk of infection increases when urinary culture is positive and with presence of urinary obstruction before SWL [11]. The previous studies were very limited and used a retrospective study design, and the conclusions were also controversial. Furthermore, none have been validated. As a result, no reliable recommendation could be provided. Therefore, we aimed to develop and validate a nomogram for predicting major complications after SWL in patients with ureteral stone based on a large prospective cohort.
Methods
Study design
This prospective study was done between June 2020 and April 2022 at Sheng**g Hospital of China Medical University. This study’s development cohort included 1522 patients who underwent SWL for ureteral stone treatment between June 2020 and August 2021. Using the same inclusion and exclusion criteria, the validation cohort comprised 553 patients between 1 September 2021 and April 2022 (Supplementary Fig. 1).
Institutional Research and Ethics Committee of Sheng**g Hospital Affiliated China Medical University granted ethical approval (No. 2020PS520K). All eligible participants provided their informed consent. The UIN for the registry of clinical research is ChiCTR2000033789. The study procedure adhered to the ethical principles of the Helsinki Declaration of 1975.
Inclusion and exclusion criteria
Inclusion criteria: ureteral stone greater than 6 mm in diameter, age ≥ 18 years, body mass index (BMI) < 30 kg/m2, ureteral stone density < 1000 Hounsfield’s units (HU), and skin-to-stone distance 11 cm. Stones with a poor probability of spontaneous passage, chronic pain despite adequate analgesia, persistent obstruction or stone development, recurrent or first-time stone formers were both eligible, and urine cultures were negative.
Exclusion criteria: pregnancy; uncontrolled urinary tract infection; coagulopathy; arterial aneurysm in the vicinity of the stone; severe skeletal malformations, which prevent targeting of the stone; patients with JJ-stent/nephrostomy insertion before treatment for the resolution of urinary tract obstruction; multiple or bilateral ureteral stones; solitary kidney; anatomical obstruction distal to the stone or congenital genitourinary anomaly (such as horseshoe kidney or ileal conduit); transplanted kidney; renal insufficiency (elevated creatinine).
After counseling the patients about the benefits and drawbacks of SWL, the decision was made based on their preferences. After the patients gave their informed consent, it was carried out by senior, experienced doctors.
The technique of shock wave lithotripsy (SWL)
A third-generation electromagnetic lithotripter was used to perform extracorporeal shock wave lithotripsy (XYS.SUI-6B, Shenzhen New Element Medical Equipment Technology Development Co., Ltd, Shenzhen, China). 11 cm served as the focal depth, 7 mm served as the focus area, 45–50 mm served as the focal area, and 6–30 MPa served as the focal pressure. Without the need for anesthesia or sedation, the procedure was carried out while the patient was lying supine (for proximal ureteral stones) or prone (for middle or distal ureteral stones). Ultrasound was used for stone location and in-process monitoring during the surgery (DC40, Shenzhen Mindray Bio-Medical Electronic Co. Ltd., Shenzhen, China). It was between 60 and 90 shock waves per minute. Between 1500 and 2500 shock waves were applied in total during one session, or the session was terminated when a sizable stone fragmentation was found. Stepwise power ram** was used to apply voltage that ranged from 10 to 16 kV throughout each session (power ram** was conducted during the first 200 shock waves). The SWL group underwent only outpatient operations.
Prior to the treatment, it was necessary to carefully manage pain to prevent significant respiratory excursions and pain-induced movements. When a urinary infection was either suspected or confirmed, an antibiotic was administered (bacteriuria). If it was difficult to identify a stone because of intestinal hindrance, a moderate laxative was used prior to the treatment. All patients received post-procedure instructions to strengthen their physical activity levels, drink more fluids, and take frequent ɑ-blockers.
Baseline characteristics and follow-up
Age, gender, and body mass index (BMI) of the patient; comorbidities (hypertension, diabetes, and coronary heart disease); prior history of urinary stones; characteristics of the stones (stone side, location, size, Hounsfield unit of the stone, skin-to-stone distance (SSD), and grade of hydronephrosis); and complications (including febrile urinary tract infection [UTI], sepsis, steinstrasse, renal colic need analgesic requirement, and renal hematoma) were recorded.
A stone between the pelvic-ureteric junction and the upper border of the sacro-iliac junction was referred to as a proximal ureteral stone. A middle ureteric stone was described as one that was between the upper and lower borders of the sacro-iliac junction (iliac vessel crossing). A stone between the lower edge of the sacro-iliac junction and the bladder’s ureter opening is referred to as a distal ureteral stone. The stone’s biggest diameter, as determined by computed tomography, was used to estimate its size (CT). When SWL was taking place, a real-time ultrasound monitor monitored the skin-to-stone distance (SSD). Using a CT scan, the degree of hydronephrosis was determined and graded from 0 to 4. Grade 0 kidneys were those without either calix or pelvic dilation; grade 1 kidneys had only pelvic dilation; grade 2 kidneys had mild calix dilation alongside; grade 3 kidneys had severe calix dilation; and grade 4 kidneys had calix dilation along with renal parenchyma atrophy. Hounsfield units were used to measure the CT attenuation value (the stone in the maximal diameter, where the elliptical region of interest incorporated the largest cross-sectional area of stone without including adjacent soft tissue).
Data on complications were classified according to the Clavien–Dindo classification [12], with Clavien II and above indicating major morbidity. Renal colic was defined as the patients who reported colic and who needed analgesic (opioids or nonsteroidal anti-inflammatory drugs) to control it. Steinstrasse were confirmed by KUB or CT after SWL, either requiring intervention or not (such as SWL retreatment, double J placement, and so on). A febrile urinary tract infection (fUTI) was defined as a body temperature higher than 38 ℃ with pyuria or bacteriuria [13]. Sepsis was defined based on the criteria set by the sepsis definitions conference [14]. Follow-up visits were performed at one month after SWL, to see if there were any complications.
Statistical analysis
IBM SPSS Statistics for Windows, version 22.0 (IBM Corporation), STATA 15.0 (Stata Corp., College Station, TX, USA), and R software (version 3.0.1; https://r-project.org/) were used to analyze the data. In this study, the ‘rms’ and ‘glmnet’ R packages were utilized. All levels of statistical significance stated were two-sided, with a probability (P) value of less than 0.05 deemed statistically significant.
Using the Kolmogorov–Smirnov test, the normality of continuous variables was established. Normally distributed continuous variables are reported as the mean standard deviation (SD), whereas non-normally distributed continuous variables are presented as the median (interquartile range). Student’s t-test was used to compare the means of two continuous normally distributed variables with independent samples. Two continuous, non-normally distributed variables were compared with the Mann–Whitney U test. As a count, categorical variables are reported (percentage). For comparing categorical variables, the chi-squared and Fisher’s exact tests were employed.
For the construction of a prediction nomogram with regression coefficients, multivariate unconditional logistic regression analysis was applied. Using the likelihood ratio test with Akaike’s information criteria as the stop** rule [15], backward stepwise selection was applied.
In an independent validation cohort, the performance of this model was evaluated. The logistic regression model derived from the development cohort was used to the validation cohort to compute the likelihood for each patient. The area under the receiver operating characteristic (AUROC) curve was calculated to characterize the discrimination performance of the model. A AUROC of 0.5 implies that there is no discrimination, whereas a value of 1.0 suggests that there is perfect discrimination. The calibration of the model was evaluated using calibration plots in conjunction with the unreliability test and the Hosmer–Lemeshow (H–L) chi-square statistic (P > 0.05 indicates good calibration). A slope on the 45-degree line indicated precise calibration. By estimating the net benefits at different threshold probabilities within the validation cohort, a decision curve analysis was undertaken to establish the clinical utility of the model.
Results
Finally, 1522 patients were included in the development cohort and 553 in the validation cohort. In both the development and validation cohorts, the median age of the enrolled patients was 48 years, the majority of patients were male (67.90 and 68.20%, respectively), and the median BMI values were around 24.00 kg/m2 (Table 1). Of these, 7.2% (110/1522) of patients in the development cohort and 8.7% (48/553) in the validation cohort suffered from major complications. Febrile UTI and sepsis occurred in 4.0% (61/1522) of patients in the development cohort and 5.5% (30/553) of patients in the validation cohort. In total, 1.8% (27/1522) of patients in the development cohort and 1.6% (9/53) of patients in the validation cohort experienced steinstrasse. Also, 1.4% (22/1522) patients in the development cohort and 1.6% (9/53) patients in the validation cohort experienced renal colic. No renal hematoma was observed in either group (Table 2).
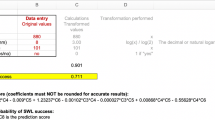
In the univariate analysis of development cohort, patients who suffered from major complications were older, had larger stone sizes, higher Hu values, were more likely to be female, and had higher grades of hydronephrosis (Table 3). The multivariate unconditional logistic regression model was used for building a predictive model with regression coefficients. Backward stepwise selection was applied using the likelihood ratio test with Akaike’s information criterion as the stop** rule. Five predictors were identified in the final model (age, gender, stone size, Hounsfield unit of stone, and grade of hydronephrosis). On the basis of these results, we built a nomogram to predict the risk of major complications after SWL (Fig. 1 and Table 4).
Nomogram to predict complications after SWL. Each clinicopathologic factor corresponds to a specific point by drawing a line straight upward to the Points axis. After summing the points located on the Total points axis, the sum represents the probability of complications after SWL by drawing a line straight down to the risk axis
The AUROC values of the development and validation cohorts were 0.887 (0.864, 0.910) and 0.885 (0.849, 0.921), respectively, and the cutoff value of risk probability in this model was 8.50% with a sensitivity of 64.58% and specificity of 75.45%. The P value of unreliability test was 0.208. The P value of H–L chi-square statistic was 0.139, which suggested good calibration. The decision curve showed that if the threshold probability of a patient ranged from 0 to 40%, the use of this nomogram to predict complications after SWL was more beneficial than either the treat-all-patients scheme or the treat-none scheme (Fig. 2).
Each clinicopathological feature corresponded to a specific point by drawing a line straight upward to the points axis. After the sum of the points was located on the total points axis, the sum representing the probability of severe morbidity was determined by drawing a line straight down to the risk axis. For example, a 60-year-old (55 points) female patient (16 points), who had a 10 mm ureteric stone (24 points) with a Hounsfield unit of 700 (64 points), presented without hydronephrosis (0 point). This patient was assigned a score of 159 points, and the suspected probability of complication after SWL was approximately 15%. This calculated outcome could be used in the decision-making regarding treatment plans (Supplementary Fig. 2).
We also produced separate results of multivariate binary logistic regression of febrile UTI, sepsis, steinstrasse and renal colic, the predictors of febrile UTI were age (P = 0.038), gender (P = 0.006), and Hounsfield unit of stone (P < 0.001); the predictors of sepsis were age (P = 0.017), gender (P = 0.006), and Hounsfield unit of stone (P < 0.001); the predictors of steinstrasse were stone size (P = 0.012), Hounsfield unit of stone (P < 0.001), and grade of hydronephrosis (P = 0.002); the predictors of renal colic were stone size (P = 0.001), and Hounsfield unit of stone (P < 0.001); see details in Supplementary Tables 1–4.
Discussion
Postoperative complications are a significant sign of the quality and safety of a procedure. Major complications after SWL are not uncommon, and because of the considerable clinical and economic burden, the identification the risk factors of complications after SWL is essential to patients, physicians, and health care policymakers. However, the risk factors for complications after SWL are not well characterized. Based on this prospective cohort, we found that the incidence of major complications after SWL was around 7.6% (158/2075), including febrile UTI, sepsis, steinstrasse, and renal colic. Furthermore, this nomogram demonstrated that age, gender, stone size, Hounsfield unit of the stone, and grade of hydronephrosis were all associated with experiencing major complications after SWL.
Most SWL-associated complications were caused by inadequate fragmentation or unsuccessful passage of stone fragments that may obstruct the ureter. In addition, there is a difference between the complications related to the administration of SWL proper (hematoma) and the complications related to stone fragmentation and fragment passage. A recent meta-analysis included 115 randomized trials, including 17,827 patients, and found that 6.63% of patients suffered from Clavien II-IV complications after SWL [16], which is in line with our findings.
This study further demonstrated that older age and female gender were both risk factors of major complications of SWL. These predictors have been reported in the stone treatment after endoscopic surgery but were first reported in the SWL procedure. In a systematic review with 13 studies and 5597 patients, Bhojani et al. [17] found that the risk of postoperative urosepsis was 5.0% among patients undergoing ureteroscopy for stone disease and that older age (P = 0.002) was statistically associated with increased postoperative urosepsis. Supporting this, the separate results of multivariate binary logistic regression of febrile UTI, and sepsis in this study were in line with previous findings. Although the chance of experiencing a postoperative complication increased with age, a clear explanation for these associations remains unavailable. One possible explanation is that the elderly were more likely to develop a postoperative complication when they had diabetes, a cardiovascular disease, or chronic obstructive pulmonary disease [18]. Ma et al. [19] performed a review with six studies and 12,357 patients, and they also identified female sex (OR = 1.82) as the key determinant of infectious complications after URS. They assumed that the short urethral length of women may cause higher possibilities of bacterial invasion from perineum to ureters when performing URS. However, this was not suitable to explain the mechanism in SWL because the procedure of SWL was non-invasive, not retrograde access. Women may have some other special characteristics (i.e., genetic differences, sex hormones) [20]. More studies are needed to further analyze the female predominance of infectious complications following SWL.
Not only the success of SWL but also the complication are associated with the stone size. Larger stones size always requires multiple treatment sessions and has a tendency to incomplete fragmentation, subsequently increasing the risk of complication due to steinstrasse development and ureter obstruction formation [21]. In line with this, we also found that larger stone size was a predictor of steinstrasse and renal colic after SWL in subgroup analysis. In a retrospective study including 885 patients with urinary stones who were treated by SWL, they found that 52 (6%) patients developed steinstrasse, and that for those with larger stones, the risk of experiencing steinstrasse will increase [22]. The optimum selection of cases and accurate stone targeting for pulverizing rather than fragmenting the stones are essential to prevent the development of steinstrasse. Complicated steinstrasse may result in ureter obstruction with renal colic and hydronephrosis. Furthermore, during stone fragmentation by shock wave, bacteria may be liberated, subsequently resulting in entry of bacteria into the blood. When urinary obstruction by fragments is added, renal colic and urosepsis could present [9]. In a retrospective research involving 1,427 ureteral stones treated with SWL, 2.9% of patients required hospitalization due to morbidity. The most common cause was medication for pain control (1.8%), which accounted for the majority of instances with larger stones [10].
This study also demonstrated that a higher Hounsfield unit of stone increased the incidence of major morbidity after SWL, which has not been reported previously. One possible reason was that the stones of struvite, uric acid, and dehydrated calcium oxalate with a lower Hu value tend to fragment into tiny fragments that may be easily passed. On the other hand, stones with higher Hu values, such as dehydrated calcium phosphate stones and monohydrate calcium oxalate stones, tend to produce larger fragments that are, hence, much harder to pass and can easily form steinstrasse [23]. In subgroup analysis, we found that high Hu values increased the incidence of steinstrasse formation and renal colic after SWL. While, low Hu values raised the incidence of febrile UTI and sepsis and renal colic after SWL. Furthermore, the predisposed factor of steinstrasse formation, including stone composition [9, 24], can be indirectly represented by the Hu value.
The grade of hydronephrosis was another contributing factor of major complications after SWL, which is rarely reported in the literature. In the subgroup analysis, we found that high grade of hydronephrosis increased the incidence of steinstrasse after SWL. Supporting this, Gad et al. also found that the effect of renal morphology on steinstrasse formation has been shown to be statistically significant in a univariate analysis [25]. In another retrospective study included 4634 patients with upper urinary stones who were treated with SWL, Madbouly et al. [9] found that steinstrasse formation was 1.8 times less in normal renal morphology than dilated renal collection system. Previous studies revealed that high intrarenal pressure is associated with reduced or absent pelvic and ureteral peristalsis. Thus, it led to less propulsive power and decreased antegrade fluid pressure with more probability of stone fragment stasis and promoted the formation of steinstrasse [9].
There were several limitations. First, a stone-free status, which may be associated with morbidity after SWL, was not included because a stone-free status and complications do not have a sequential relationship, but a synchronous relationship. Usually, a stone-free status is only confirmed when complications are already established. Second, our relatively short postoperative follow-up period could not estimate late complications, such as the regrowth of residual fragments, hypertension, or loss of renal function. Third, only Asian patients participated in this study, because variations may occur in patients with a different body habitus. The performance of this nomogram for patients of other ethnicities needs to be further assessed. Nevertheless, these results fill a gap in the literature as there is no published study predicting the complications of SWL that has been carried out in a prospective cohort with excellent validation.
Conclusion
In this large prospective cohort, we found that older age, female gender, higher Hounsfield unit, size, and grade of hydronephrosis were risk predictors of major complications after SWL. This nomogram will be helpful in preoperative risk stratification to provide individualized treatment recommendations for each patient. Furthermore, early identification and appropriate management of high-risk patients may decrease postoperative morbidity.
References
Lang J, Narendrula A, El-Zawahry A, Sindhwani P, Ekwenna O (2022) Global trends in incidence and burden of urolithiasis from 1990 to 2019: an analysis of global burden of disease study data. Eur Urol Open Sci 35:37–46
Zhe M, Hang Z (2017) Nephrolithiasis as a risk factor of chronic kidney disease: a meta-analysis of cohort studies with 4,770,691 participants. Urolithiasis 45(5):441–448
Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, Pace KT, Pais VM Jr, Pearle MS, Preminger GM, Razvi H, Shah O, Matlaga BR (2016) Surgical management of stones: American urological association/endourological society guideline PART II. J Urol 196(4):1161–1169
EAU https://uroweb.org/guidelines/urolithiasis/chapter/guidelines. Accessed 01 Feb 2023
Skolarikos A, Alivizatos G, de la Rosette J (2006) Extracorporeal shock wave lithotripsy 25 years later: complications and their prevention. Eur Urol 50(5):981–990
Somani BK (2021) After COVID-19: planning postpandemic care of patients with kidney stones. Nat Rev Urol 18(9):511–512
Lazaros L, Tzelves L, Glykas I, Berdempes M, Chatzikrachtis N, Skolarikos A, Varkarakis I (2021) “Lock-down” for COVID-19 has “locked up” Urological emergencies in Greece. El confinamiento por COVID-19 ha parado las urgencias urológicas en Grecia. Arch Esp Urol 74(2):183–184
Hiller SC, Dauw CA, Ghani KR, Collaborative MUSI (2020) Kidney stone care and the COVID-19 pandemic: challenges and opportunities. J Urol 204(6):1122–1124
Madbouly K, Sheir KZ, Elsobky E, Eraky I, Kenawy M (2002) Risk factors for the formation of a steinstrasse after extracorporeal shock wave lithotripsy: a statistical model. J Urol 167(3):1239–1242
Tan YM, Yip SK, Chong TW, Wong MY, Cheng C, Foo KT (2002) Clinical experience and results of ESWL treatment for 3093 urinary calculi with the Storz Modulith SL 20 lithotripter at the Singapore general hospital. Scand J Urol Nephrol 36(5):363–367
Müller-Mattheis VG, Schmale D, Seewald M, Rosin H, Ackermann R (1991) Bacteremia during extracorporeal shock wave lithotripsy of renal calculi. J Urol 146(3):733–736
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Hsieh CH, Yang SS, Chang SJ (2016) The effectiveness of prophylactic antibiotics with oral levofloxacin against post-shock wave lithotripsy infectious complications: a randomized controlled trial. Surg Infect 17(3):346–351
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315(8):801–810
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ (Clinical Research ed) 350:g7594
Tzelves L, Geraghty R, Mourmouris P, Chatzikrachtis N, Karavitakis M, Somani B, Skolarikos A (2022) Shockwave lithotripsy complications according to modified Clavien–Dindo grading system. A systematic review and meta-regression analysis in a sample of 115 randomized controlled trials. Eur Urol Focus 8(5):1452–1460
Bhojani N, Miller LE, Bhattacharyya S, Cutone B, Chew BH (2021) Risk factors for urosepsis after ureteroscopy for stone disease: a systematic review with meta-analysis. J Endourol 35(7):991–1000
Daels FP, Gaizauskas A, Rioja J, Varshney AK, Erkan E, Ozgok Y, Melekos M, de la Rosette JJ (2015) Age-related prevalence of diabetes mellitus, cardiovascular disease and anticoagulation therapy use in a urolithiasis population and their effect on outcomes: the clinical research office of the endourological society ureteroscopy global study. World J Urol 33(6):859–864
Ma YC, Jian ZY, Yuan C, Li H, Wang KJ (2020) Risk factors of infectious complications after ureteroscopy: a systematic review and meta-analysis based on adjusted effect estimate. Surg Infect 21(10):811–822
Robinson D, Toozs-Hobson P, Cardozo L (2013) The effect of hormones on the lower urinary tract. Menopause Int 19(4):155–162
Lingeman JE, Coury TA, Newman DM, Kahnoski RJ, Mertz JH, Mosbaugh PG, Steele RE, Woods JR (1987) Comparison of results and morbidity of percutaneous nephrostolithotomy and extracorporeal shock wave lithotripsy. J Urol 138(3):485–490
Sayed MA, el-Taher AM, Aboul-Ella HA, Shaker SE (2001) Steinstrasse after extracorporeal shockwave lithotripsy: aetiology, prevention and management. BJU Int 88(7):675–678
D’Addessi A, Vittori M, Racioppi M, Pinto F, Sacco E, Bassi P (2012) Complications of extracorporeal shock wave lithotripsy for urinary stones: to know and to manage them-a review. Sci World J 2012:619820
Abdel-Khalek M, Sheir KZ, Mokhtar AA, Eraky I, Kenawy M, Bazeed M (2004) Prediction of success rate after extracorporeal shock-wave lithotripsy of renal stones–a multivariate analysis model. Scand J Urol Nephrol 38(2):161–167
Gad HM, Sheir KZ, Sadek GH (2000) 6 Effects of SWL to one kidney on bilateral renal function. Nuclear Med Commun 21(4):370–371
Acknowledgements
We give special thanks to all the colleagues at the Department of Urology of Sheng**g Hospital for their help and support. We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript. The authors would like to thank all of the study participants.
Funding
This study was financially supported by The 345 Talent Project of Sheng**g Hospital, Natural Science Foundation of Liaoning Science and Technology Department (grant number 2020-BS-093), and Natural Science Foundation of Liaoning Education Department (grant number QN2019013). These sponsors had no role in the study design; in the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
SB had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. SB: Protocol/project development. LN, JL, CP, YZ and SB: Data collection or management. LN and SB: Data analysis. LN and SB: Manuscript writing/editing.
Corresponding authors
Ethics declarations
Conflict of interest
Song Bai certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (e.g, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Ethical approval
Ethical approval (No.2020PS520K) was provided by the Institutional Research and Ethics Committee of the Sheng**g Hospital Affiliated China Medical University. Informed consent was obtained from all eligible subjects. The clinical research registry UIN is ChiCTR2000033789. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsink.
Consent for publication
Informed consent from all eligible patients was obtained.
Availability of data and materials
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Na, L., Li, J., Pan, C. et al. Development and validation of a predictive model for major complications after extracorporeal shockwave lithotripsy in patients with ureteral stones: based on a large prospective cohort. Urolithiasis 51, 42 (2023). https://doi.org/10.1007/s00240-023-01417-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00240-023-01417-7