Abstract
Purpose
Atherosclerotic cardiovascular disease (ASCVD) is a leading cause of mortality worldwide. Statins, which are effective in preventing ASCVD, are underused, particularly for primary prevention. This study examined trends in statin use for primary ASCVD prevention from 1999 to 2020, focusing on demographic variations.
Methods
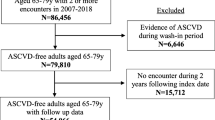
Utilizing data from the National Health and Nutrition Examination Survey, the present study includes individuals aged 18 years and older who had a greater than 10% risk of ASCVD over 10 years, and excluded patients with existing ASCVD. Subgroup analyses by demographic categories were performed. We calculated the changes in statin usage and used linear and quadratic tests to assess the linear and nonlinear trends in those changes.
Results
A total of 10,037 participants were included. Statin usage increased from 16.16% in 1999 to 36.24% in 2010, and 41.74% in 2020 (quadratic P-value < 0.001). In the 18–44 years age group, statin usage increased from 2.52% in 1999 to 8.14% in 2020 (linear P-value = 0.322), showing no significant linear trend. In the “never-married” group, statin usage increased from 19.16% in 1999 to 30.05% in 2020 (linear P-value = 0.256).
Conclusion
Statin usage has shown a positive trend among populations requiring primary prevention for ASCVD. Currently, health policies are proving effective. However, the overall statin usage rate remains less than 50%. Additionally, young and never-married individuals should also receive special attention regarding statin usage as primary treatment for ASCVD.


Similar content being viewed by others
Code availability
Code sharing is not applicable to this article as no codes were generated or analyzed during the current study.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
GBD 2017 Causes of Death Collaborators (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England) 392(10159):1736–1788. https://doi.org/10.1016/s0140-6736(18)32203-7
D’Agostino R, Vasan R, Pencina M et al (2008) General cardiovascular risk profile for use in primary care: the Framingham Heart Study. 117(6):743–753. https://doi.org/10.1161/circulationaha.107.699579
Perk J, Graham I, De Backer GJH (2014) Prevention of cardiovascular disease: new guidelines, new tools, but challenges remain. 2014; 100(9):675–677. https://doi.org/10.1136/heartjnl-2014-305650
Kantor E, Rehm C, Haas J, Chan A, Giovannucci EJJ (2015) Trends in prescription drug use among adults in the United States from 1999–2012. 314(17):1818–1831. https://doi.org/10.1001/jama.2015.13766
Pedersen T, Kjekshus J, Berg K et al (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). 2004;5(3):81 – 7. https://doi.org/10.1016/j.atherosclerosissup.2004.08.027
Mihaylova B, Emberson J, Blackwell L et al (2012) The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. 380(9841):581–590. https://doi.org/10.1016/s0140-6736(12)60367-5
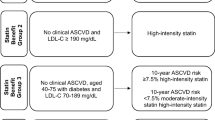
Stone N, Robinson J, Lichtenstein A et al (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. 63:2889–2934. https://doi.org/10.1016/j.jacc.2013.11.002
Grundy SM, Stone NJ, Bailey AL et al (2019) AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 139(25):e1082–e143. https://doi.org/10.1161/cir.0000000000000625
Mehra VM, Gaalema DE, Pakosh M, Grace SL (2020) Systematic review of cardiac rehabilitation guidelines: quality and scope. Eur J Prev Cardiol 27(9):912–928. https://doi.org/10.1177/2047487319878958
Chou R, Cantor A, Dana T et al (2022) Statin use for the primary prevention of cardiovascular disease in adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 328(8):754–771. https://doi.org/10.1001/jama.2022.12138
Schonberger RB, Vallurupalli V, Matlin H et al (2020) Underuse of statins for secondary prevention of atherosclerotic cardiovascular disease events among ambulatory surgical patients. Prev Med Rep 18:101085. https://doi.org/10.1016/j.pmedr.2020.101085
Onaisi R, Dumont R, Hasselgard-Rowe J et al (2022) Multimorbidity and statin prescription for primary prevention of cardiovascular diseases: a cross-sectional study in general practice in France. Front Med 9:1089050. https://doi.org/10.3389/fmed.2022.1089050
Metser G, Bradley C, Moise N et al (2021) Gaps and disparities in primary prevention statin prescription during outpatient care. Am J Cardiol 161:36–41. https://doi.org/10.1016/j.amjcard.2021.08.070
Zipf G, Chiappa M, Porter K et al National health and nutrition examination survey: plan and operations, 1999–2010. 2013(56):1–37
Schwartz G, Olsson A, Ezekowitz M et al (2001) Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. 285(13):1711–1718. https://doi.org/10.1001/jama.285.13.1711
Serruys P, de Feyter P, Macaya C et al (2002) Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. 287(24):3215–3222. https://doi.org/10.1001/jama.287.24.3215
Shepherd J, Cobbe S, Ford I et al (1995) Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West Scotl Coron Prev Study Group 333(20):1301–1307. https://doi.org/10.1056/nejm199511163332001
Colhoun H, Betteridge D, Durrington P et al (2004) Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the collaborative atorvastatin diabetes study (CARDS): multicentre randomised placebo-controlled trial. 364(9435):685–696. https://doi.org/10.1016/s0140-6736(04)16895-5
Byrne P, Demasi M, Jones M et al (2022) Evaluating the association between low-density lipoprotein cholesterol reduction and relative and absolute effects of statin treatment: a systematic review and meta-analysis. 182(5):474–481. https://doi.org/10.1001/jamainternmed.2022.0134
Weintraub W, Lüscher T, Pocock SJE (2015) The perils of surrogate endpoints. 36(33):2212–2218. https://doi.org/10.1093/eurheartj/ehv164
Silverman M, Ference B, Im K et al (2016) Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. 316(12):1289–1297. https://doi.org/10.1001/jama.2016.13985
Savelieva I, Kourliouros A, Camm J (2010) Primary and secondary prevention of atrial fibrillation with statins and polyunsaturated fatty acids: review of evidence and clinical relevance. Naunyn Schmiedebergs Arch Pharmacol 381(3):1–13. https://doi.org/10.1007/s00210-009-0468-y
JA (2019) ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. 2019;290:140–205. https://doi.org/10.1016/j.atherosclerosis.2019.08.014
Rosengren AJEhj (2012) Better treatment and improved prognosis in elderly patients with AMI: but do registers tell the whole truth? 33(5):562–563. https://doi.org/10.1093/eurheartj/ehr364
Wessel A, Gravenhorst V, Buchhorn R et al (2004) Risk of sudden death in the Williams-Beuren syndrome. Am J Med Genet Part A 127a(3):234–237. https://doi.org/10.1002/ajmg.a.30012
Lewington S, Whitlock G, Clarke R et al (2007) Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. 370(9602):1829–1839. https://doi.org/10.1016/s0140-6736(07)61778-4
Grundy S, Stone N, Bailey A, NLA/PCNA Guideline on the Management of Blood Cholesterol (2019) A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. 139(25):e1082–e143. https://doi.org/10.1161/cir.0000000000000625. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/
Fulcher J, O’Connell R, Voysey M et al (2015) Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. 385(9976):1397–1405. https://doi.org/10.1016/s0140-6736(14)61368-4
Antza C, Gallo A, Boutari C et al (2023) Prevention of cardiovascular disease in young adults: focus on gender differences. A collaborative review from the EAS Young fellows. Atherosclerosis 384:117272. https://doi.org/10.1016/j.atherosclerosis.2023.117272
Holven KB, van Roeters J (2023) Sex differences in lipids: a life course approach. Atherosclerosis 384:117270. https://doi.org/10.1016/j.atherosclerosis.2023.117270
Bosco G, Di Giacomo Barbagallo F, Di Marco M et al (2024) The impact of SLCO1B1 rs4149056 on LDL-C target achievement after lipid lowering therapy optimization in men and women with familial hypercholesterolemia. Front Endocrinol 15:1346152. https://doi.org/10.3389/fendo.2024.1346152
Carnethon M, Pu J, Howard G et al (2017) Cardiovascular health in African Americans: a scientific statement. Am Heart Association 136(21):e393–e423. https://doi.org/10.1161/cir.0000000000000534
Gujral U, Vittinghoff E, Mongraw-Chaffin M et al (2017) Cardiometabolic abnormalities among normal-weight persons from five racial/ethnic groups in the United States: a cross-sectional analysis of two cohort studies. 166(9):628–636. https://doi.org/10.7326/m16-1895
Benner J, Glynn R, Mogun H et al (2002) Long-term persistence in use of statin therapy in elderly patients. 288(4):455–461. https://doi.org/10.1001/jama.288.4.455
Global regional et al (2016) and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England). ;388(10053):1659 – 724. https://doi.org/10.1016/s0140-6736(16)31679-8
Roelfs DJ, Shor E, Kalish R, Yogev T (2011) The rising relative risk of mortality for singles: meta-analysis and meta-regression. Am J Epidemiol 174(4):379–389. https://doi.org/10.1093/aje/kwr111
Acknowledgements
We express our gratitude to the staff at the National Center for Health Statistics at the CDC for their diligence in data collection and release.
Funding
This study was supported by Sichuan Provincial Cadre Health Research Project, China (Sichuan Ganyan ZH2024-101), and by 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (Grant number: 2021HXFH061, Sichuan, China).
Author information
Authors and Affiliations
Contributions
WJW and PY were responsible for study concept and design, statistical analysis and interpretation of the data, and drafting and redrafting of the manuscript. WJW and YYY were responsible for statistical analysis. WJW and CXF were responsible for data acquisition. WJW and PY contributed to critical revision of the manuscript. WJW, HXR, and PY prepared Figs. 1, 2, and 3. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of the National Center for Health Statistics approved this study. All participants provided written informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• The utilization rate of statins among individuals needing primary prevention of ASCVD has significantly increased.
• There was no notable improvement trend among never-married individuals or those aged 18–44 years.
• Current health policies have been effective at increasing statin use for primary prevention in patients at risk for ASCVD, but the overall usage rate remains below 50%.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Ye, Y., Chen, X. et al. Trends in statin use for the primary prevention of atherosclerotic cardiovascular disease among US adults by demographic characteristics, 1999–2020. Eur J Clin Pharmacol (2024). https://doi.org/10.1007/s00228-024-03699-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00228-024-03699-1