Abstract
Purpose
To identify the radiological predictive risk factors for anterior cruciate ligament reconstruction (ACLR) failure, compare the diagnostic accuracies of different parameters of conventional radiographs and magnetic resonance imaging (MRI), and determine the cutoff values for patients at higher risk.
Methods
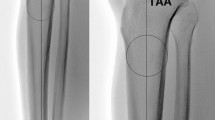
Twenty-eight patients who were diagnosed as ACLR failure via MRI or arthroscopic examination were included in the study group. They were matched to 56 patients who underwent primary ACLR with the same surgical technique and without graft failure at the minimum 24-month follow-up by age, sex, and body mass index. On true lateral whole-leg radiographs, the posterior tibial slope (PTS) referenced to the tibial mechanical axis (PTS-mechanical), PTS referenced to the tibial proximal anatomical axis (PTS-anatomical), and anterior tibial translation (ATT) were measured. On the sagittal slices of MRI, the medial tibial slope (MTS), medial tibial plateau (MTP) subluxation (MTPsublx), lateral tibial slope (LTS), and lateral tibial plateau (LTP) subluxation (LTPsublx) were obtained. Receiver operator characteristic (ROC) curves were constructed to compare the diagnostic performance and determine the cutoff values of different radiological parameters.
Results
The study group demonstrated higher values of PTS-mechanical (10.7° ± 2.9° vs 8.7° ± 1.9°, p = 0.003), PTS-anatomical (13.2° ± 2.8° vs 10.5° ± 2.5°, p < 0.001), ATT (10.7 ± 3.3 mm vs 8.9 ± 2.2 mm, p = 0.014), LTS (9.4° ± 2.1° vs 5.5° ± 2.5°, p < 0.001), and LTPsublx (8.2 ± 2.8 mm vs 6.8 ± 1.9 mm, p = 0.009) as compared with the control group. The area under the ROC curve of LTS was significantly larger than that of PTS-mechanical (p = 0.006) and PTS-anatomical (p = 0.020). Based on the maximum Youden indexes, the cutoff values of PTS-mechanical, PTS-anatomical, and LTS were 10.1° (sensitivity, 64.3%; specificity, 78.6%), 12.0° (sensitivity, 71.4%; specificity, 71.4%), and 7.7° (sensitivity, 85.7%; specificity, 80.4%), respectively.
Conclusion
Due to the morphological asymmetry of the MTP and LTP, steep LTS measured on MRI is the best radiological predictor of ACLR failure. Detailed measurement of the LTS on MRI is recommended to evaluate the risk of ACLR failure prior to the surgery.
Level of evidence
III.




Similar content being viewed by others
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACLR:
-
Anterior cruciate ligament reconstruction
- ATT:
-
Anterior tibial translation
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- FTA:
-
Femur–tibia angle
- HKA:
-
Hip–knee–ankle angle
- ICC:
-
Interclass correlation coefficient
- LARS:
-
Ligament advanced reinforcement system
- LTH:
-
Lateral tibial height
- LTP:
-
Lateral tibial plateau
- LTPsublx:
-
Lateral tibial plateau subluxation
- LTS:
-
Lateral tibial slope
- MCL:
-
Medial collateral ligament
- MRI:
-
Magnetic resonance imaging
- MRI-TA:
-
Tibial axis on magnetic resonance imaging
- MTD:
-
Medial tibial depth
- MTP:
-
Medial tibial plateau
- MTPsublx:
-
Medial tibial plateau subluxation
- MTS:
-
Medial tibial slope
- PCL:
-
Posterior cruciate ligament
- PLC:
-
Knee posterolateral corner
- PTS:
-
Posterior tibial slope
- PTS-anatomical:
-
Posterior tibial slope referenced to the tibial proximal anatomical axis
- PTS-mechanical:
-
Posterior tibial slope referenced to the tibial mechanical axis
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- TMA:
-
Tibial mechanical axis
- TPAA:
-
Tibial proximal anatomical axis
References
Balcarek P, Terwey A, Jung K, Walde TA, Frosch S, Schüttrumpf JP et al (2013) Influence of tibial slope asymmetry on femoral rotation in patients with lateral patellar instability. Knee Surg Sports Traumatol Arthrosc 21:2155–2163
Bayer S, Meredith SJ, Wilson KW, de Sa D, Pauyo T, Byrne K et al (2020) Knee morphological risk factors for anterior cruciate ligament injury: a systematic review. J Bone Jt Surg Am 102:703–718
Bernhardson AS, Aman ZS, Dornan GJ, Kemler BR, Storaci HW, Brady AW et al (2019) Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med 47:296–302
Chen JL, Allen CR, Stephens TE, Haas AK, Huston LJ, Wright RW et al (2013) Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med 41:1571–1578
Davey AP, Vacek PM, Caldwell RA, Slauterbeck JR, Gardner-Morse MG, Tourville TW et al (2019) Risk factors associated with a noncontact anterior cruciate ligament injury to the contralateral knee after unilateral anterior cruciate ligament injury in high school and college female athletes: a prospective study. Am J Sports Med 47:3347–3355
Dean RS, DePhillipo NN, Chahla J, Larson CM, LaPrade RF (2021) Posterior tibial slope measurements using the anatomic axis are significantly increased compared with those that use the mechanical axis. Arthroscopy 37:243–249
Dejour D, Saffarini M, Demey G, Baverel L (2015) Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc 23:2846–2852
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Jt Surg Br 76:745–749
Faschingbauer M, Sgroi M, Juchems M, Reichel H, Kappe T (2014) Can the tibial slope be measured on lateral knee radiographs? Knee Surg Sports Traumatol Arthrosc 22:3163–3167
Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32:376–382
Grassi A, Macchiarola L, Urrizola Barrientos F, Zicaro JP, Costa Paz M, Adravanti P et al (2019) Steep posterior tibial slope, anterior tibial subluxation, deep posterior lateral femoral condyle, and meniscal deficiency are common findings in multiple anterior cruciate ligament failures: an MRI case–control study. Am J Sports Med 47:285–295
Hodel S, Kabelitz M, Tondelli T, Vlachopoulos L, Sutter R, Fucentese SF (2019) Introducing the lateral femoral condyle index as a risk factor for anterior cruciate ligament injury. Am J Sports Med 47:2420–2426
Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP (2009) Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res 467:2066–2072
Imhoff FB, Comer B, Obopilwe E, Beitzel K, Arciero RA, Mehl JT (2021) Effect of slope and varus correction high tibial osteotomy in the ACL-deficient and ACL-reconstructed knee on kinematics and ACL graft force: a biomechanical analysis. Am J Sports Med 49:410–416
Imhoff FB, Mehl J, Comer BJ, Obopilwe E, Cote MP, Feucht MJ et al (2019) Slope-reducing tibial osteotomy decreases ACL-graft forces and anterior tibial translation under axial load. Knee Surg Sports Traumatol Arthrosc 27:3381–3389
Jahn R, Cooper JD, Juhan T, Kang HP, Bolia IK, Gamradt SC et al (2021) Reliability of plain radiographs versus magnetic resonance imaging to measure tibial slope in sports medicine patients: can they be used interchangeably? Orthop J Sports Med 9:23259671211033880
Kiapour AM, Yang DS, Badger GJ, Karamchedu NP, Murray MM, Fadale PD et al (2019) Anatomic features of the tibial plateau predict outcomes of ACL reconstruction within 7 years after surgery. Am J Sports Med 47:303–311
Leppänen M, Parkkari J, Vasankari T, Äyrämö S, Kulmala JP, Krosshaug T et al (2021) Change of direction biomechanics in a 180-degree pivot turn and the risk for noncontact knee injuries in youth basketball and floorball players. Am J Sports Med 49:2651–2658
Lindanger L, Strand T, Mølster AO, Solheim E, Inderhaug E (2019) Return to play and long-term participation in pivoting sports after anterior cruciate ligament reconstruction. Am J Sports Med 47:3339–3346
Lipps DB, Wilson AM, Ashton-Miller JA, Wojtys EM (2012) Evaluation of different methods for measuring lateral tibial slope using magnetic resonance imaging. Am J Sports Med 40:2731–2736
Meier M, Zingde S, Best R, Schroeder L, Beckmann J, Steinert AF (2020) High variability of proximal tibial asymmetry and slope: a CT data analysis of 15,807 osteoarthritic knees before TKA. Knee Surg Sports Traumatol Arthrosc 28:1105–1112
Micicoi G, Jacquet C, Khakha R, LiArno S, Faizan A, Seil R et al (2021) Femoral and tibial bony risk factors for anterior cruciate ligament injuries are present in more than 50% of healthy individuals. Am J Sports Med 49:3816–3824
Misir A, Sayer G, Uzun E, Guney B, Guney A (2022) Individual and combined anatomic risk factors for the development of an anterior cruciate ligament rupture in men: a multiple factor analysis case–control study. Am J Sports Med. https://doi.org/10.1177/036354652110625943635465211062594
Naendrup JH, Drouven SF, Shaikh HS, Jaecker V, Offerhaus C, Shafizadeh ST et al (2020) High variability of tibial slope measurement methods in daily clinical practice: comparisons between measurements on lateral radiograph, magnetic resonance imaging, and computed tomography. Knee 27:923–929
Ni QK, Song GY, Zhang ZJ, Zheng T, Feng Z, Cao YW et al (2020) Steep posterior tibial slope and excessive anterior tibial translation are predictive risk factors of primary anterior cruciate ligament reconstruction failure: a case-control study with prospectively collected data. Am J Sports Med 48:2954–2961
Øiestad BE, Holm I, Risberg MA (2018) Return to pivoting sport after ACL reconstruction: association with osteoarthritis and knee function at the 15-year follow-up. Br J Sports Med 52:1199–1204
Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA (2018) 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med 46:531–543
Shelbourne KD, Benner RW, Jones JA, Gray T (2021) Posterior tibial slope in patients undergoing anterior cruciate ligament reconstruction with patellar tendon autograft: analysis of subsequent ACL graft tear or contralateral ACL tear. Am J Sports Med 49:620–625
Song GY, Ni QK, Zheng T, Zhang ZJ, Feng H, Zhang H (2020) Slope-reducing tibial osteotomy combined with primary anterior cruciate ligament reconstruction produces improved knee stability in patients with steep posterior tibial slope, excessive anterior tibial subluxation in extension, and chronic meniscal posterior horn tears. Am J Sports Med 48:3486–3494
Sonnery-Cottet B, Mogos S, Thaunat M, Archbold P, Fayard JM, Freychet B et al (2014) Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med 42:1873–1880
Southam BR, Colosimo AJ, Grawe B (2018) Underappreciated factors to consider in revision anterior cruciate ligament reconstruction: a current concepts review. Orthop J Sports Med 6:2325967117751689
Winkler PW, Godshaw BM, Karlsson J, Getgood AMJ, Musahl V (2021) Posterior tibial slope: the fingerprint of the tibial bone. Knee Surg Sports Traumatol Arthrosc 29:1687–1689
Yamaguchi KT, Cheung EC, Markolf KL, Boguszewski DV, Mathew J, Lama CJ et al (2018) Effects of anterior closing wedge tibial osteotomy on anterior cruciate ligament force and knee kinematics. Am J Sports Med 46:370–377
Zhao J (2021) Anatomic double-bundle transtibial anterior cruciate ligament reconstruction. Arthrosc Tech 10:e683–e690
Funding
(1) National Key Research and Development Program of China (2018YFC1106200, 2018YFC1106202) [**zhong Zhao]; (2) Natural Science Foundation of Shanghai (19ZR1438500, 20S31900700) [Shikui Dong]. The funding source did not play a role in the investigation.
Author information
Authors and Affiliations
Contributions
ZY: Conceptualization; investigation; formal analysis; writing—original draft. JX and JC: Conceptualization; methodology; writing—original draft. YQ and CW: Investigation; data curation. GX and SD: Methodology; formal analysis; supervision. JZ: Conceptualization; supervision; writing—review and editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
Approved by the Ethics Committee of Shanghai Sixth People’s Hospital (Approval No: 2016-111; date of review: 2016-10-26).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ye, Z., Xu, J., Chen, J. et al. Steep lateral tibial slope measured on magnetic resonance imaging is the best radiological predictor of anterior cruciate ligament reconstruction failure. Knee Surg Sports Traumatol Arthrosc 30, 3377–3385 (2022). https://doi.org/10.1007/s00167-022-06923-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06923-6