Abstract
Objective
The aim is to stabilize the thoracolumbar spine with a thoracoscopically implanted vertebral body replacement (VBR). To improve intraoperative depth perception and orientation, implantation is performed under three-dimensional (3D) thoracoscopic vision.
Indications
Vertebral burst fractures at the thoracolumbar junction (A4 AOSpine classification), pseudarthrosis, and posttraumatic instability with increasing kyphosis.
Contraindications
Severe pulmonary dysfunctions, pulmonary or thoracic infections, previous thoracic surgery, and pulmonary adhesions.
Surgical technique
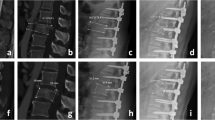
The patient is lying in a right lateral decubitus position. Localization of the fractured vertebra. Minimally invasive transthoracic approach. Perform single lung ventilation and insert the 3D thoracoscope two intercostal spaces above the working portal. Utilization of special binocular glasses for 3D vision of the operation field and secure resection of the fractured vertebra.
Measurement of the bony defect and insertion of the expandable cage. Control of correct cage position under fluoroscopy. Insertion of a chest tube and inflate the left lung.
Postoperative management
Chest × ray
Remove chest tube when output is <500 ml/24 h
Early mobilization on the ward
6 weeks no weight-bearing >5 kg
Results
Between 2012 and 2017, 12 patients received a VBR under 3D thoracoscopic vision. After a mean follow up of 26 months, no cage dislocation was noticed and all patients recovered from the initial back pain. Complications were notable in two cases (17%) with a small pneumothorax after removal of the chest tube and postoperative pneumonia in one patient (8%). All responded to conservative treatment. Revision surgery was not necessary.
Zusammenfassung
Operationsziel
Wiederherstellung einer belastungsstabilen Wirbelsäule durch thorakoskopische Implantation eines Wirbelkörperersatzes. Zur Verbesserung der intraoperativen Tiefenwahrnehmung und Orientierung erfolgt die Implantation unter 3‑dimensionaler (3-D) Thorakoskopie.
Indikationen
Thorakolumbale Berstungsfrakturen (A4 nach AOSpine-Klassifikation), Pseudarthrose, posttraumatische Instabilität mit zunehmender Kyphose
Kontraindikationen
Schwere pulmonale Dysfunktion, pulmonale oder thorakale Infektionen, thorakale Voroperationen, pulmonale Adhäsionen
Operationstechnik
Lagerung in Rechtsseitenlage auf der Vakuummatratze. Lokalisation des frakturierten Wirbelkörpers. Minimalinvasiver transthorakaler Zugang. Einlungenventilation und Einbringen des Thorakoskops 2 Interkostalräume kranial des Arbeitsportals. Nach Aufsetzen der 3‑D-Brillen entsteht ein 3‑D-Bild des Operationsgebiets und eine sichere Resektion des frakturierten Wirbelkörpers ist möglich. Ausmessen des knöchernen Defekts und Einsetzen des expandierbaren Cage. Lagekontrolle unter Bildwandler. Einlage einer Thoraxdrainage und Entfalten der linken Lunge.
Weiterbehandlung
Röntgenuntersuchung des Thorax a.-p.; Entfernung der Thoraxdrainage bei Fördermenge <500 ml/24 h; frühzeitige Mobilisation auf Stationsebene; 6 Wochen postoperativ kein Heben und Tragen >5 kg
Ergebnisse
Zwischen 2012 und 2017 wurde bei 12 Patienten ein Wirbelkörperersatz in 3‑D-thorakoskopischer Technik durchgeführt. Während einer durchschnittlichen Follow-up-Zeit von 26 Monaten wurde keine Implantatdislokation festgestellt. Alle Patienten beschrieben eine wesentliche Linderung der initialen Rückenschmerzen. Als Komplikation wurde bei 2 Patienten (17 %) ein schmaler Pneumothorax nach Entfernung der Thoraxdrainage festgestellt, bei einem Patienten (8 %) eine Pneumonie. Alle Komplikationen wurden erfolgreich konservativ behandelt. Revisionsoperationen waren nicht erforderlich.
















Similar content being viewed by others
Change history
14 September 2018
Erratum to:
Oper Orthop Traumatol 2018
https://doi.org/10.1007/s00064-018-0559-3
The article was wrongly published under the article type “Review”. Please note that the article is an “Original Paper”.
The publisher apologizes to authors and …
References
Alaraimi B, El Bakbak W, Sarker S et al (2014) A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) vs. two-dimensional (2D) laparoscopy. World J Surg 38:2746–2752. https://doi.org/10.1007/s00268-014-2674-0
Beisse R (2007) Endoscopic treatment of spinal trauma at the thoracolumbar junction. Indian J Orthop 41:277–285. https://doi.org/10.4103/0019-5413.36987
Buia A, Stockhausen F, Filmann N, Hanisch E (2017) 2D vs. 3D imaging in laparoscopic surgery-results of a prospective randomized trial. Langenbecks Arch Surg 402:1241–1253. https://doi.org/10.1007/s00423-017-1629-y
Chan AC, Chung SC, Yim AP et al (1997) Comparison of two-dimensional vs three-dimensional camera systems in laparoscopic surgery. Surg Endosc 11:438–440
Hodgoson AR, Stock FE, Fang HS, Ong GB (1960) Anterior spinal fusion. The operative approach and pathological findings in 412 patients with Pott’s disease of the spine. Br J Surg 48:172–178
Knop C, Blauth M, Bastian L et al (1997) Fractures of the thoracolumbar spine. Unfallchirurg 100:630–639. https://doi.org/10.1007/s001130050168
McLachlan G (2011) From 2D to 3D: the future of surgery? Lancet 378:1368
Ragel BT, Amini A, Schmidt MH (2007) Thoracoscopic vertebral body replacement with an expandable cage after ventral spinal canal decompression. Neurosurgery 61:317–322. https://doi.org/10.1227/01.neu.0000303988.57493.b6 (discussion 322–3)
Romero-Loera S, Cárdenas-Lailson LE, la de Concha-Bermejillo F et al (2016) Skills comparison using a 2D vs. 3D laparoscopic simulator. Cir Cir 84:37–44. https://doi.org/10.1016/j.circir.2015.06.032
Smith R, Day A, Rockall T et al (2012) Advanced stereoscopic projection technology significantly improves novice performance of minimally invasive surgical skills. Surg Endosc 26:1522–1527. https://doi.org/10.1007/s00464-011-2080-8
Vaccaro AR, Oner C, Kepler CK et al (2013) AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine 38:2028–2037. https://doi.org/10.1097/BRS.0b013e3182a8a381
Wenzl R, Lehner R, Vry U et al (1994) Three-dimensional video-endoscopy: clinical use in gynaecological laparoscopy. Lancet 344:1621–1622. https://doi.org/10.1016/S0140-6736(94)90412-X
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. Jacobs, M.M. Plöger, S. Scheidt, P.P. Roessler, S. Koob, K. Kabir, C. Jacobs, D.C. Wirtz, C. Burger, R. Pflugmacher, and F. Trommer declare that they have no competing interests.
Data for this retrospective study were gathered after approval by the appropriate ethics commission of the University of Bonn (IRB 193/17) and in accordance with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Editor
M. Mayer, München
Illustrator
J. Kühn, Heuchelheim-Klingen
C. Jacobs and M.M. Plöger contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Jacobs, C., Plöger, M.M., Scheidt, S. et al. Three-dimensional thoracoscopic vertebral body replacement at the thoracolumbar junction. Oper Orthop Traumatol 30, 369–378 (2018). https://doi.org/10.1007/s00064-018-0559-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00064-018-0559-3