Abstract
Background
Optimal anesthetic strategy for the endovascular treatment of stroke is still under debate. Despite scarce data concerning anesthetic management for medium and distal vessel occlusions (MeVOs) some centers empirically support a general anesthesia (GA) strategy in these patients.
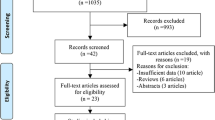
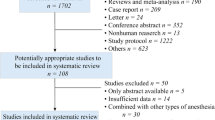
Methods
We conducted an international retrospective study of MeVO cases. A propensity score matching algorithm was used to mitigate potential differences across patients undergoing GA and conscious sedation (CS). Comparisons in clinical and safety outcomes were performed between the two study groups GA and CS. The favourable outcome was defined as a modified Rankin Scale (mRS) 0–2 at 90 days. Safety outcomes were 90-days mortality and symptomatic intracranial hemorrhage (sICH). Predictors of a favourable outcome and sICH were evaluated with backward logistic regression.
Results
After propensity score matching 668 patients were included in the CS and 264 patients in the GA group. In the matched cohort, either strategy CS or GA resulted in similar rates of good functional outcomes (50.1% vs. 48.4%), and successful recanalization (89.4% vs. 90.2%). The GA group had higher rates of 90-day mortality (22.6% vs. 16.5%, p < 0.041) and sICH (4.2% vs. 0.9%, p = 0.001) compared to the CS group. Backward logistic regression did not identify GA vs CS as a predictor of good functional outcome (OR for GA vs CS = 0.95 (0.67–1.35)), but GA remained a significant predictor of sICH (OR = 5.32, 95% CI 1.92–14.72).
Conclusion
Anaesthetic strategy in MeVOs does not influence favorable outcomes or final successful recanalization rates, however, GA may be associated with an increased risk of sICH and mortality.

Similar content being viewed by others
References
Campbell D, Butler E, Campbell RB, Ho J, Barber PA. General anesthesia compared with non-GA in endovascular thrombectomy for Ischemic stroke. Neurology. 2023;100(16):e1655. http://n.neurology.org/content/100/16/e1655.abstract.
Simonsen CZ, Yoo AJ, Sørensen LH, Juul N, Johnsen SP, Andersen G, et al. Effect of general anesthesia and conscious sedation during Endovascular therapy on infarct growth and clinical outcomes in acute Ischemic stroke: a randomized clinical trial. JAMA Neurol. 2018;75(4):470–7. https://doi.org/10.1001/jamaneurol.2017.4474.
Löwhagen Hendén P, Rentzos A, Karlsson JE, Rosengren L, Leiram B, Sundeman H, et al. General anesthesia versus conscious sedation for endovascular treatment of acute Ischemic stroke. Stroke. 2017;48(6):1601–7. https://doi.org/10.1161/STROKEAHA.117.016554.
Schönenberger S, Uhlmann L, Hacke W, Schieber S, Mundiyanapurath S, Purrucker JC, et al. Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular Thrombectomy: a randomized clinical trial. JAMA. 2016;316(19):1986–96. https://doi.org/10.1001/jama.2016.16623.
Chabanne R, Geeraerts T, Begard M, Balança B, Rapido F, Degos V, et al. Outcomes after endovascular therapy with procedural sedation vs general anesthesia in patients with acute Ischemic stroke: the AMETIS randomized clinical trial. JAMA Neurol. 2023;80(5):474–83. https://doi.org/10.1001/jamaneurol.2023.0413.
Maurice A, Eugène F, Ronzière T, Devys JM, Taylor G, Subileau A, et al. General anesthesia versus sedation, both with hemodynamic control, during Intraarterial treatment for stroke: the GASS randomized trial. Anesthesiology. 2022;136(4):567–76. https://doi.org/10.1097/ALN.0000000000004142.
Campbell BCV, van Zwam WH, Goyal M, Menon BK, Dippel DWJ, Demchuk AM, et al. Effect of general anesthesia on functional outcome in patients with anterior circulation ischaemic stroke having endovascular thrombectomy versus standard care: a meta-analysis of individual patient data. Lancet Neurol. 2018;17(1):47–53. https://doi.org/10.1016/S1474-4422(17)30407-6.
Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. 2020; https://doi.org/10.1161/STROKEAHA.120.028956.
Kappelhof M, Ospel JM, Cimflova P, Kashani N, Singh N, McDonough R, et al. Worldwide anaesthesia use during endovascular treatment for medium vessel occlusion stroke. Interv Neuroradiol. 2021;28(4):469–75. https://doi.org/10.1177/15910199211041487.
Cappellari M, Pracucci G, Forlivesi S, Saia V, Nappini S, Nencini P, et al. General anesthesia versus conscious sedation and local anesthesia during thrombectomy for acute Ischemic stroke. Stroke. 2020;51(7):2036–44.
Meyer L, Stracke CP, Broocks G, Wallocha M, Elsharkawy M, Sporns PB, et al. Effect of anesthetic strategies on distal stroke thrombectomy in the anterior and posterior cerebral artery. J Neurointerv Surg. 2024; https://doi.org/10.1136/jnis-2023-020210. https://jnis.bmj.com/content/early/2023/05/03/jnis-2023-020210.
Siegler JE, Shaikh H, Khalife J, Oak S, Zhang L, Abdalkader M, et al. Aspiration versus stent-retriever as first-line endovascular therapy technique for primary medium and distal Intracranial occlusions: a propensity-score matched multicenter analysis. Stroke. 2023; https://doi.org/10.1161/SVIN.123.000931.
Radu RA, Costalat V, Fahed R, Ghozy S, Siegler JE, Shaikh H, et al. First pass effect as an independent predictor of functional outcomes in medium vessel occlusions: An analysis of an international multicenter study. Eur Stroke J. 2023; https://doi.org/10.1177/23969873231208276.
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet. 1998;352(9136):1245–51. https://doi.org/10.1016/S0140-6736(98)08020-9.
Schönenberger S, Hendén PL, Simonsen CZ, Uhlmann L, Klose C, Pfaff JAR, et al. Association of general anesthesia vs procedural sedation with functional outcome among patients with acute Ischemic stroke undergoing Thrombectomy: a systematic review and meta-analysis. JAMA. 2019;322(13):1283–93.
Terceño M, Bashir S, Cienfuegos J, Murillo A, Vera-Monge VA, Pardo L, et al. General anesthesia versus conscious sedation during endovascular treatment in posterior circulation large vessel occlusion: a systematic review and meta-analysis. Eur Stroke J. 2023;8(1):85–92. https://doi.org/10.1177/23969873221127738.
Han H, Wang Y, Wang H, Sun H, Wang X, Gong J, et al. General anesthesia vs. local anesthesia during endovascular treatment for acute large vessel occlusion: a propensity score-matched analysis. Front Neurol. 2021;12:801024.
Amini M, van Leeuwen N, Eijkenaar F, van de Graaf R, Samuels N, van Oostenbrugge R, et al. Estimation of treatment effects in observational stroke care data: comparison of statistical approaches. BMC Med Res Methodol. 2022;22(1):1–12. https://doi.org/10.1186/s12874-022-01590-0.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
R.W. Regenhardt serves on a DSMB for a trial sponsored by Rapid Medical, serves as site PI for studies sponsored by Penumbra and Microvention, and receives stroke research grant funding from the National Institutes of Health, Society of Vascular and Interventional Neurology, and Heitman Stroke Foundation. A. Guenego reports consultancy for Rapid Medical and Phenox, not directly related to the present work. F. Clarençon reports conflicts of interest with Medtronic, Balt Extrusion (consultant), ClinSearch (core lab), Penumbra, Stryker (payment for reading) and Artedrone (Board) ; all not directly related to the present work. N. Henninger received support from NINDS NS131756, during the conduct of the study. D.S. Liebeskind is consultant as Imaging Core Lab to Cerenovus, Genentech, Medtronic, Stryker, Rapid Medical. T.N. Nguyen reports advisory board with Idorsia. L.L.L. Yeo reports Advisory work for AstraZeneca, Substantial support from NMRC Singapore and is a medical advisor for See-mode, Cortiro and Sunbird Bio, with equity in Ceroflo. All unrelated to the present work. C.J. Griessenauer reports a proctoring agreement with Medtronic and research funding by Penumbra. G. Marnat reports conflicts of interest with Microvention Europe, Stryker Neurovascular, Balt (consulting), Medtronic, Johnson & Johnson and Phenox (paid lectures), all not directly related to the present work. I. Sibon reports conflict of interest with Medtronic, Sanofi, Bayer, Boehringer-Ingelheim, Novartis, Novo-nordisk, BMS-Pfizer (Board and paid lectures), all not directly related to the present work. V. Yedavalli is a consultant for RAPID (Ischemaview, Menlo Park, CA). A. Vagal is a consultant for Viz AI. She is also PI of the Imaging core lab for the ENDOLOW study funded by Cerenovus (monies go to the institution). A. Gopinathan reports conflicts of interest with Microvention, Stryker Neurovascular, Medtronic, BD, and Penumbra (paid lectures, workshops, and proctoring), all not directly related to the present work. R. A. Radu, V. Costalat, M. Romoli, B. Musmar, J.E. Siegler, S. Ghozy, J. Khalife, H. Salim, H. Shaikh, N. Adeeb, H.H. Cuellar-Saenz, A.J. Thomas, R. Kadirvel, M. Abdalkader, P. Klein, J.J. Heit, J.D. Bernstock, A.B. Patel, J.D. Rabinov, C.J. Stapleton, N.M. Cancelliere, T.R. Marotta, V. Mendes Pereira, K. El Naamani, A. Amllay, S.I. Tjoumakaris, P. Jabbour, L. Meyer, J. Fiehler, T.D. Faizy, H. Guerreiro, A. Dusart, F. Bellante, G. Forestier, A. Rouchaud, C. Mounayer, A.L. Kühn, A.S. Puri, C. Dyzmann, P.T. Kan, M. Colasurdo, J. Berge, X. Barreau, S. Nedelcu, T. Ota, S. Dofuku, B.Y. Tan, J.C. Martinez-Gutierrez, S. Salazar-Marioni, S. Sheth, L. Renieri, C. Capirossi, A. Mowla, L.M. Chervak, P. Khandelwal, A. Biswas, M. Elhorany, K. Premat, I. Valente, A. Pedicelli, A.M. Alexandre, J.P. Filipe, R. Varela, M. Quintero-Consuegra, N.R. Gonzalez, M.A. YMD, J. Jesser, C. Weyland, A. ter Schiphorst, P. Harker, Y. Aziz, B. Gory, C. Paul Stracke, C. Hecker, M. Killer-Oberpfalzer, C.-Y. Hsieh, I. Tancredi, R. Fahed, B. Lubicz, M.A. Essibayi, A. Baker, D. Altschul, L. Scarcia, E. Kalsoum and A.A. Dmytriw for the MAD-MT Consortium declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Radu, R.A., Costalat, V., Romoli, M. et al. Outcomes with General Anesthesia Compared to Conscious Sedation for Endovascular Treatment of Medium Vessel Occlusions: Results of an International Multicentric Study. Clin Neuroradiol (2024). https://doi.org/10.1007/s00062-024-01415-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00062-024-01415-1